Abstract
Objective
Prehospital provider assessment of the use of anticoagulant or antiplatelet medications in older adults with head trauma is important. These patients are at increased risk for traumatic intracranial hemorrhage and therefore field triage guidelines recommend transporting these patients to centers capable of rapid evaluation and treatment. Our objective was to evaluate EMS ascertainment of anticoagulant and antiplatelet medication use in older adults with head trauma.
Methods
A retrospective study of older adults with head trauma was conducted throughout Sacramento County. All 5 transporting EMS agencies and all 11 hospitals in the county were included in the study, which ran from January 2012 to December 2012. Patients ≥55 years who were transported to a hospital by EMS after head trauma were included. We excluded patients transferred between two facilities, patients with penetrating head trauma, prisoners, and patients with unmatched hospital data. Anticoagulant and antiplatelet use were categorized as: warfarin, direct oral anticoagulants (DOAC; dabigatran, rivaroxaban, and apixaban), aspirin, and other antiplatelet agents (e.g., clopidogrel, ticagrelor). We calculated the percent agreement and kappa statistic for binary variables between EMS and emergency department (ED)/hospital providers. A kappa statistic ≥0.60 was considered acceptable agreement.
Results
After excluding 174 (7.6%) patients, 2,110 patients were included for analysis; median age was 73 years (interquartile range 62–85 years) and 1,259 (60%) were male. Per ED/hospital providers, the use of any anticoagulant or antiplatelet agent was identified in 595 (28.2%) patients. Kappa statistics between EMS and ED/hospital providers for the specific agents were: 0.76 (95% CI 0.71–0.82) for warfarin, 0.45 (95% CI 0.19–0.71) for DOAC agents, 0.33 (95% CI 0.28–0.39) for aspirin, and 0.51 (95% CI 0.42–0.60) for other antiplatelet agents.
Conclusions
The use of antiplatelet or anticoagulant medications in older adults who are transported by EMS for head trauma is common. EMS and ED/hospital providers have acceptable agreement with preinjury warfarin use but not with DOAC, aspirin, and other antiplatelet use.
Keywords: Emergency Medical Services, Anticoagulants, Platelet Aggregation Inhibitors, Medication Reconciliation, Head Injuries, Closed
BACKGROUND
Traumatic brain injury (TBI) accounts for an estimated 2.2 million emergency department (ED) visits, 280,000 hospitalizations and more than 50,000 deaths in the US at an estimated cost of $60 billion annually.1,2 With an aging population, older adults represent an increasing proportion of TBI patients treated at hospitals.3 Older adults have higher morbidity and mortality after TBI than younger patients due to anatomical differences, co-morbidities, and more frequent use of anticoagulant and antiplatelet medications.1,3–5 The concurrent use of these medications in the setting of head trauma is especially problematic, increasing the risk for traumatic intracranial hemorrhage (tICH) and post-traumatic disability and death.6–8 Rapid diagnosis of tICH with cranial computed tomography (CT) is critical to determine the need for reversal of anticoagulant and antiplatelet effects with medications and blood products. Patients who have a delay in reversal have increased morbidity and mortality.9 In patients on warfarin requiring immediate neurosurgical intervention, rapid and efficacious reversal to an appropriate international normalized ratio (INR) level is essential as INR levels >1.25 increase postoperative mortality.10–12
Accuracy of medication history in patients with preinjury anticoagulant or antiplatelet use and head trauma is crucial. Clinicians who are unaware that their patient is taking one of these medications may not obtain appropriate diagnostic imaging.13,14 Recommendations for cranial CT imaging after head trauma is much more liberal in anticoagulated patients compared to patients not on these medications.13,16 Many of these patients are initially well-appearing and have low impact mechanisms of injury such as ground level falls, but have significant tICH requiring neurosurgical interventions and specialized critical care.17–20 Older adults have low trauma center utilization but a high rate of interfacility transfers.21 In the prehospital setting, however, a number of barriers exist to accurate medication ascertainment including the acuity of the clinical presentation, limited access to prior medical records and medication lists, limited availability of family or translators, and unfamiliarity with medications by patients and their families. In addition, prehospital providers may be unaware of the names and uses of some of the newer anticoagulant or antiplatelet medications. Older adults with head trauma are particularly prone to these barriers, and they often have inaccurate and delayed medication reconciliation.22
Our objective for this study was to evaluate emergency medical services (EMS) medication ascertainment of preinjury anticoagulant and antiplatelet use in older adults with head trauma. EMS medication ascertainment was compared to a reference standard of ED and hospital medication ascertainment.
METHODS
Study Design
This was a countywide, retrospective study at 5 EMS agencies and 11 hospitals. The study was approved by the UC Davis Institutional Review Board, the Dignity Health Sacramento-Sierra Regional Institutional Review Board, the Kaiser Permanente Northern California Institutional Review Board, and the Sutter Health Central Area Institutional Review Committee.
Study Setting and Subjects
This study was conducted primarily in Sacramento County, which encompasses 994 square miles and has a resident population of 1,445,327 (2010 census). Sacramento County is served by 5 advanced life support EMS agencies that respond to all 9-1-1 medical emergencies. Over 2,400 EMS personnel are certified or accredited by the Sacramento County EMS Agency, including approximately 1,050 Paramedics and 1,400 Emergency Medical Technicians. The county has 9 general acute care hospitals and access to 2 additional hospitals in the adjacent county. We included these two out-of-county acute care hospitals since Sacramento County EMS agencies routinely transport patients to these two hospitals. Cumulatively, these hospitals have a capacity of approximately 240 ED beds and 3,400 total staffed in-patient beds. One hospital is a Level I adult trauma center and 3 are Level II adult trauma centers. In 2011, there were 3,345 major trauma victims admitted to the 4 designated trauma centers from incidents within Sacramento County.
We included patients 55 years and older with head trauma who were transported to a hospital by EMS from January 1, 2012 to December 31, 2012. The age cutoff of 55 years was chosen based on recommendations of the National Expert Panel on Field Triage, 2011.18 The risk for death after injury increases after age 55.18 The patient cohort was identified using billing data of the EMS agencies and the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) diagnosis codes 959.01 (head injury unspecified) or 959.09 (injury of face and neck). Other head injury ICD-9 diagnostic codes were not used (e.g., 851 to 854 [traumatic intracranial hemorrhage]) as these codes require CT imaging for appropriate diagnosis. We excluded patients transferred by EMS from another receiving facility (interfacility transport), patients with penetrating head trauma, prisoners, and patients with unmatched hospital data.
Study Protocol and Measurements
All EMS agencies used similar prehospital patient care report (PCR) forms that included transport information, patient demographics, medical history, history of present illness, vital signs, physical examination findings, treatments, and assessments. Three of the EMS agencies used paper PCR forms and two of the agencies used electronic PCR forms. All medications were written or typed in.
A trained research coordinator abstracted the following data from EMS charts: patient identifiers (name, date of birth), transport characteristics (date of transport, EMS agency, level of transport, level of EMS provider, receiving hospital), antiplatelet and anticoagulant use in the past week (listed anywhere in the EMS chart), mechanism of injury, and clinical characteristics (initial Glasgow Coma Scale [GCS] score, reported dementia, reported intoxication). Anticoagulants included warfarin or direct oral anticoagulants (DOAC; dabigatran, rivaroxaban or apixaban). Antiplatelets included aspirin or other antiplatelet agents (clopidogrel, ticlodipine, prasugrel, dipyridamole, cilostazol, and ticagrelor).
Eligible EMS patient transports were linked to ED and hospital records using patient identifiers (name, date of birth, and date of transport). For the linked hospital visit, we reviewed ED and hospital electronic records including ED physician notes, hospital admission and discharge physician notes, and medication reconciliation lists and abstracted the following data: patient demographics (age, sex, ethnicity, race), antiplatelet and anticoagulant use, and INR levels.
Data Analysis
We formatted the data and recoded the variables using STATA 13.1 statistical software (STATA Corp, College Station, TX). Descriptive statistics were used to characterize the study population overall and within each indication category. Non-normal interval data were reported with medians and interquartile ranges.
For each anticoagulant and antiplatelet category (warfarin, DOAC, aspirin, and other antiplatelet agent) we calculated the percent present per EMS, the overall agreement, the percent specific agreement within each response option, and the kappa statistic (with 95% confidence intervals [CI]) using normal approximation methods.23 We considered a kappa statistic of 0.60 or higher to have acceptable agreement.24,25
We conducted three sensitivity analyses. First, we compared EMS medication ascertainment of preinjury warfarin use to initial elevated INR levels (greater than 1.2) because the use of ED and hospital provider medication ascertainment may not be accurate as a reference standard. The INR level is an objective reference standard for warfarin use, but its use is limited in warfarin patients with subtherapeutic levels, patients who did not have an INR level obtained, and patients with elevated INR levels due to other factor deficiencies such as chronic liver disease rather than warfarin use. Second, we explored differences in medication ascertainment between different agencies by stratifying the warfarin, aspirin, and other antiplatelet agent groups by EMS agency and generated a plot of the kappa statistics with CIs. Third, we stratified EMS and ED/hospital agreement for preinjury warfarin use by level of transport (Advanced Life Support [ALS] vs. Basic Life Support [BLS]) and level of EMS provider (paramedic vs. non-paramedic) to evaluate for differences in level of training on medication ascertainment. For the 2nd and 3rd sensitivity analyses, we did not include the kappa statistics for the DOAC group due to the small number of patients with preinjury DOAC use during the study period.
RESULTS
Characteristics of the Subjects
We excluded 174 (7.6%) patients; 173 for unmatched hospital data and 1 with penetrating head trauma. Thus 2,110 patients were included for analysis. The median age was 73 years (interquartile range 62–85 years) and 1,259 (60%) were male. The most common mechanism of injury was fall from standing height or less (68%). The majority of patients had an initial GCS score by EMS of 15 (81%). Complete patient characteristics are reported in Table 1. The range of enrolled transports by EMS agency was 104 to 952 transports. Complete EMS provider characteristics are reported in Table 2.
Table 1.
Patient Characteristics, n=2110
| Characteristic | n (%) |
|---|---|
| Age, median (interquartile range) | 73 (62–85) |
| Male sex | 1259 (60) |
| Race | |
| • White | 1403 (66) |
| • Black | 172 (8) |
| • Asian | 182 (9) |
| • American Indian/Alaskan Native | 11 (0.52) |
| • Pacific Islander/Native Hawaiian | 27 (1.3) |
| • Other | 169 (8) |
| • Not reported | 205 (10) |
| Hispanic | 141 (6.7) |
| Initial prehospital Glasgow Coma Scale score of 15 a | 1638 (81) |
| Mechanism of injury | |
| • Direct blow to head | 107 (5) |
| • Fall from greater than standing height | 81 (4) |
| • Fall from standing height or less | 1445 (68) |
| • Motor vehicle collision >35 miles per hour | 117 (6) |
| • Motor vehicle collision ≤35 miles per hour | 186 (9) |
| • Auto vs. pedestrian/bicyclist | 58 (3) |
| • Other mechanism of injury | 57 (3) |
| • Unknown mechanism | 59 (3) |
| Pre-hospital intubation or use of bag valve mask device | 4 (0.2) |
| Reported dementia | 254 (12) |
| Reported intoxication | 213 (10) |
| Primary language is not English | 129 (6.1) |
| • If language was not English, prehospital provider was able to obtain an medication history | 76 (58.9) |
| ➢ Using some English | 31 (41) |
| ➢ Translated | 41 (54) |
| ➢ Other means | 4 (5) |
missing GCS scores in 61 patients
Table 2.
EMS Provider Characteristics, n=2110 transports
| Characteristic | n (%) |
|---|---|
| EMS Agency | |
| • Agency 1 | 278 (13) |
| • Agency 2 | 150 (7) |
| • Agency 3 | 104 (5) |
| • Agency 4 | 952 (45) |
| • Agency 5 | 626 (30) |
| Advance Life Support transport | 1199 (57) |
| EMS provider was paramedic | 1567 (74) |
Abbreviations: EMS, Emergency Medical Services
Main Results
EMS providers recorded the use of any anticoagulant or antiplatelet medication in 349 patients (16.5%). Warfarin use was recorded in 123 patients (5.8%), direct oral anticoagulant use in 7 patients (0.33%), aspirin use in 184 patients (8.7%), and other antiplatelet use in 59 patients (2.8%). ED and hospital providers recorded the use of any anticoagulant or antiplatelet medication use in 595 patients (28.2%). Warfarin use was identified in 168 patients (8.0%), direct oral anticoagulant use in 15 patients (0.71%), aspirin use in 372 patients (17.6%), and 115 patients (5.5%) with other antiplatelet agent use. Overall agreement for any anticoagulant or antiplatelet medication use between EMS providers and ED and hospital providers was 90.5% with a kappa statistic of 0.45 (95% CI 0.41 to 0.49).
Only warfarin use (kappa 0.76) had acceptable agreement between EMS and ED/hospital providers while DOAC (kappa 0.45), aspirin (kappa 0.33), and other antiplatelet use (kappa 0.51) did not meet our acceptable agreement threshold (kappa 0.60 or higher). Percent agreement and the kappa statistic for each subgroup of preinjury anticoagulant and antiplatelet use are reported in Table 3 and eTable 1 (Online Supplement).
Table 3.
Agreement between EMS vs. ED/hospital providers for preinjury anticoagulant or antiplatelet use
| Preinjury medication | n (%) per EMS providers | Overall agreement, % | Positive agreement, % | Negative agreement, % | Kappa statistic (95% CI) |
|---|---|---|---|---|---|
| Warfarin | 123 (5.8) | 96.9 | 67.3 | 99.5 | 0.76 (0.71–0.82) |
| DOAC a | 7 (0.3) | 99.4 | 33.3 | 99.9 | 0.45 (0.19–0.71) |
| Aspirin | 184 (8.7) | 84.5 | 30.6 | 96.0 | 0.33 (0.28–0.39) |
| Other antiplatelet agent b | 115 (5.5) | 96.1 | 40.0 | 99.3 | 0.51 (0.42–0.60) |
Abbreviations: EMS, Emergency Medical Services; ED, emergency department
Direct oral anticoagulant, includes dabigatran, rivaroxaban, and apixaban
Other antiplatelet agent includes clopidogrel, ticlodipine, prasugrel, dipyridamole, cilostazol, or ticagrelor
Sensitivity Analyses
When an elevated INR (>1.2) was used as the reference standard for warfarin use, EMS providers had an overall percent agreement of 95.4% (positive agreement of 70.8%, negative agreement of 97.5%) and a kappa statistic of 0.68 (95% CI 0.62–0.74).
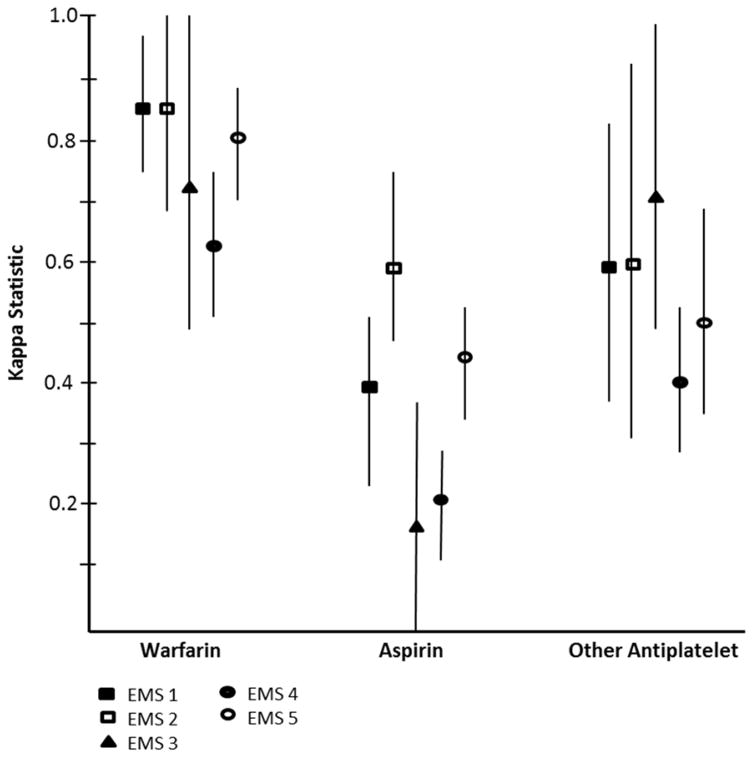
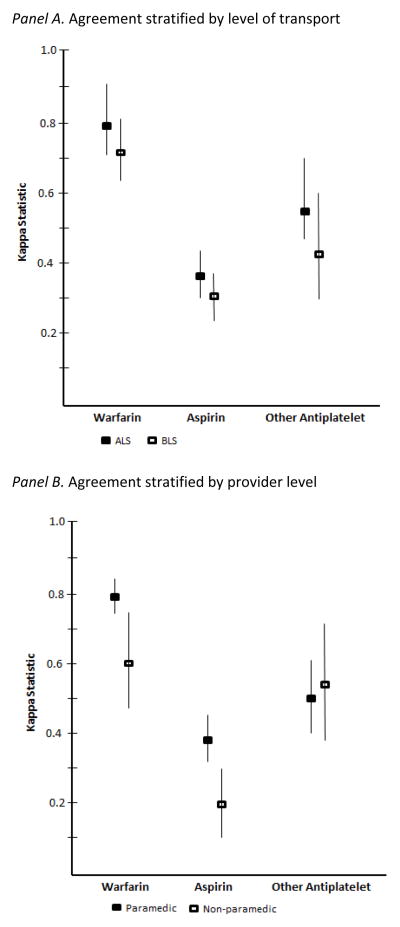
As demonstrated in Figure 1, the differences in agreement between warfarin and the other anticoagulant and antiplatelet agents were overall consistent within each EMS agency. Stratifying agreement by level of transport (ALS vs. BLS) suggested no difference in agreement between ALS and BLS transport (Figure 2, Panel A). However, stratifying by provider level (paramedic vs. non-paramedic) suggested a higher level of agreement with warfarin and aspirin use for paramedics compared to non-paramedics but no difference with other antiplatelet agents (Figure 2, Panel B). Complete agreement measurements presented in eTable 2 (Online Supplement).
Figure 1.
Agreement stratified by EMS agency and medication
Figure 2. Agreement stratified by level of transport and provider level.
Panel A. Agreement stratified by level of transport
Panel B. Agreement stratified by provider level
DISCUSSION
Our study compared EMS to ED/hospital medication ascertainment of preinjury anticoagulant and antiplatelet use in older adults with head trauma. Our study included 1 year of data from 5 EMS agencies and 11 receiving hospitals which accounted for the entire county’s 9-1-1 volume. The results of our study demonstrated two key findings. First, preinjury use of any antiplatelet or anticoagulant medication in older adults with head trauma was common – ED and hospital providers recorded that over 28% of patients were taking these medications. Second, only EMS medication ascertainment for preinjury warfarin use had an acceptable level of agreement with ED and hospital providers. Medication ascertainment for DOAC, aspirin, and other antiplatelet agent use had kappa statistics less than 0.60.
For EMS providers, obtaining an accurate medication history in patients with preinjury anticoagulant or antiplatelet use in the setting of head trauma is important. Older adults with preinjury anticoagulant or antiplatelet use are often initially well-appearing and have low impact mechanisms of injury (e.g., ground level falls) and thus do not routinely meet physiological, anatomical, or mechanism of injury criteria for field triage to a trauma center.17,18 However, these patients not infrequently have life-threatening tICH requiring emergent neurosurgical interventions and specialized critical care.19,20 The most recent field triage guidelines (2011) were modified to highlight the risk for rapid neurological deterioration in older adults with preinjury anticoagulant or antiplatelet use.18 Step four of these triage guidelines include the statement that patients with head trauma and either anticoagulant use or bleeding disorders are at high risk for rapid deterioration and EMS providers should consider transporting these patients to a trauma center.18
To our knowledge, this is the first study that evaluated EMS medication ascertainment of preinjury anticoagulant and antiplatelet use across a broad cohort of older adults with head trauma. The characteristics of our patient population were similar to prior studies of older adults with head trauma – the majority of patients presented to the ED after a ground level fall and with a normal mental status.14,26,27 Evans et al reported 60% of older adults presenting to the ED after a fall had preinjury use of anticoagulant or antiplatelet agents.28 However, the study included only patients triaged to the trauma resuscitation room and thus these patients more likely to be severely injured compared to our study. We identified one prior study that compared prehospital and ED medication reconciliation.29 Damlien et al found a 62% rate of clinically relevant medication discrepancies between prehospital and ED medication reconciliation. Age 60 years or older was an independent risk factor for having a clinically relevant medication discrepancy.
Our results suggest that prehospital medication ascertainment is better in patients with preinjury warfarin use than in patients with preinjury aspirin or other antiplatelet agents use. This may be due to EMS providers having greater awareness of the bleeding issues from warfarin and being more vigilant in identifying preinjury warfarin use than antiplatelet agents. Many head injury guidelines highlight the risk of intracranial bleeding in patients with warfarin use but they do not consider antiplatelet agents an indication for cranial imaging.13,15,16 Preinjury clopidogrel use in the setting of blunt head trauma, however, has been shown to have a higher risk for tICH than preinjury warfarin use.14 The higher level of agreement with warfarin compared to aspirin or other antiplatelet agents may also be due to patients reporting warfarin use to prehospital providers more accurately than reporting antiplatelet use. Older adults are particularly at risk for providing inaccurate medication histories.30 In addition, frequent INR checks in patients taking warfarin and their perceived risks of bleeding may make patients more aware of warfarin use than antiplatelet use.31
The threshold of a kappa statistic ≥0.60 for acceptable interrater agreement is based on precedent.24,25 Different thresholds of acceptability (e.g., kappa statistic ≥ 0.50) or use of the lower bound of the 95% confidence interval of the kappa statistic (≥ 0.40) have also been used.32–34 Several instances where the percent agreement was high (>80%) but the kappa statistic was fair or moderate (0.21 to 0.60) occurred due to what is known as the “kappa paradox”.35 In situations where the prevalence is very low or very high, the resulting kappa statistic may not fully reflect the reliability of the measure, necessitating the use of other measures such as percent agreement.36 The kappa paradox is particularly true for the evaluation of DOAC use. Due to the small number of patients taking DOAC agents at the time of our study, the measures of agreement for DOAC use has wide confidence intervals. Our study included patients from 2012, thus many of the DOAC agents were very new to the market (dabigatran [2010], rivaroxaban [2011] and apixaban [2012] for nonvalvular atrial fibrillation; rivaroxaban for venous thromboembolism prophylaxis [2011; knee or hip surgery] and treatment [2012]). With increasing use of the DOAC agents, future studies should be directed at evaluating prehospital medication ascertainment of these medications.37
Given the importance of identifying all medications that increase the risk for tICH, future work may include using enhanced electronic patient care records such as drop down lists or disease specific alerts.38 Our sensitivity analysis stratifying by level of EMS provider suggested a higher level of agreement with warfarin and aspirin use with paramedics compared to non-paramedics. This finding suggests that prehospital medication ascertainment might be improved either by enhanced education and training and/or by attempting to increase the proportion of transfers for which a paramedic does the PCR documentation.
Our results should be interpreted in the context of some limitations. First, this was a retrospective study and subject to the inherent limitations of using retrospective data.39 Second, ED and hospital documentation of medication use as the reference standard may be problematic. ED and hospital medication ascertainment may also be subject to the same limitations as prehospital medication ascertainment (e.g., patients who are poor historians or acutely injured). However, we conducted a sensitivity analysis using an elevated INR as the reference standard for patients on warfarin and found similar agreement measurements. Third, data is provided only on documented use of anticoagulants and antiplatelets. It is possible that EMS providers knew that a patient was taking a particular anticoagulant or antiplatelet medication and verbalized this to ED staff, however did not document it on medical records. Finally, the results of this study are based on data primarily from one county and may not be generalizable to other EMS systems. However, we included EMS agencies and hospitals that differed by volume of transports and trauma center designation and thus represents a heterogeneous EMS system.
CONCLUSIONS
The use of antiplatelet or anticoagulant medications in older adults with blunt head trauma and transported by EMS is common. EMS and ED/hospital providers have acceptable agreement with when assessing for a patient’s use of warfarin but not with DOAC, aspirin, and other antiplatelet agent use.
Supplementary Material
Acknowledgments
This work was funded by the Centers for Disease Control and Prevention (CDC), grant number U01CE002177. The findings and conclusion of this research are those of the authors and do not represent the official views of the US Department of Health and Human Services (DHHS) and the CDC. The inclusion of individuals, programs, or organizations in this article does not constitute endorsement by the US federal government, DHHS, or CDC.
Dr. Nishijima was supported through Mentored Clinical Research Training Program Award (Grant Number UL1TR000002 and linked award KL2TR000134) from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
We would like to acknowledge Megan Gilbert, Nicole B. Kreutzberg, Renee P. Trajano, Linda Marks, Lindsey Holloway, Dennis Carter, Hernando Garzon, MD, and Mathew Foley, MD for their assistance with administrative aspects of the study. We appreciate the assistance of James A. Chenoweth, MD and Kiarash Shahlaie, MD, PhD for their critical commentary of the manuscript.
Footnotes
Author Contribution:
Conception: DN, SG, TW, RM, TB, AB, AE, RF, CH, JM, JB, VC, DS, DV, DB, JH
Performance: DN, SG, TW, RM, TB, AB, AE, RF, CH, JM
Analysis: DN, SG
Writing of the manuscript: All authors
Meeting Presentation:
Presented at the Society of Academic Emergency Medicine Annual Meeting, New Orleans, LA May 2016
References
- 1.Faul MXL, Wal MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths 2002–2006. US Department of Health and Human Services, CDC; Atlanta, GA: 2010. [Google Scholar]
- 2.Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95(5):986–95. doi: 10.1016/j.apmr.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma. 2009;66(3):942–50. doi: 10.1097/TA.0b013e3181978e7b. [DOI] [PubMed] [Google Scholar]
- 4.Rathlev NK, Medzon R, Lowery D, Pollack C, Bracken M, Barest G, Wolfson AB, Hoffman JR, Mower WR. Intracranial pathology in elders with blunt head trauma. Acad Emerg Med. 2006;13(3):302–7. doi: 10.1197/j.aem.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Mushkudiani NA, Engel DC, Steyerberg EW, Butcher I, Lu J, Marmarou A, Slieker F, McHugh GS, Murray GD, Maas AI. Prognostic value of demographic characteristics in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24(2):259–69. doi: 10.1089/neu.2006.0028. [DOI] [PubMed] [Google Scholar]
- 6.Li J, Brown J, Levine M. Mild head injury, anticoagulants, and risk of intracranial injury. Lancet. 2001;357(9258):771–2. doi: 10.1016/S0140-6736(00)04163-5. [DOI] [PubMed] [Google Scholar]
- 7.Mina AA, Knipfer JF, Park DY, Bair HA, Howells GA, Bendick PJ. Intracranial complications of preinjury anticoagulation in trauma patients with head injury. J Trauma. 2002;53(4):668–72. doi: 10.1097/00005373-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Jones K, Sharp C, Mangram AJ, Dunn EL. The effects of preinjury clopidogrel use on older trauma patients with head injuries. Am J Surg. 2006;192(6):743–5. doi: 10.1016/j.amjsurg.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 9.Ivascu FA, Howells GA, Junn FS, Bair HA, Bendick PJ, Janczyk RJ. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. 2005;59(5):1131–7. doi: 10.1097/01.ta.0000189067.16368.83. [DOI] [PubMed] [Google Scholar]
- 10.Boulis NM, Bobek MP, Schmaier A, Hoff JT. Use of factor IX complex in warfarin-related intracranial hemorrhage. Neurosurgery. 1999;45(5):1113–8. doi: 10.1097/00006123-199911000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Kawamata T, Takeshita M, Kubo O, Izawa M, Kagawa M, Takakura K. Management of intracranial hemorrhage associated with anticoagulant therapy. Surg Neurol. 1995;44(5):438442. doi: 10.1016/0090-3019(95)00249-9. [DOI] [PubMed] [Google Scholar]
- 12.Yasuda CL, Morita ME, Nishimori FY, Yasuda AM, Alves HL. Chronic subdural hematoma: study of 161 patients and the relationship with coagulation abnormalities. Arq Neuropsiquiatr. 2003;61(4):1011–4. doi: 10.1590/s0004-282x2003000600023. [DOI] [PubMed] [Google Scholar]
- 13.Jagoda AS, Bazarian JJ, Bruns JJ, Jr, Cantrill SV, Gean AD, Howard KP, Ghajar J, Riggio S, Wright DW, Wears RL, Bakshy A, Burgess P, Walk MM, Whitson RR. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52(6):714–48. doi: 10.1016/j.annemergmed.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 14.Nishijima DK, Offerman SR, Ballard DW, Vinson DR, Chettipally UK, Rauchwerger AS, Reed ME, Holmes JF Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460–8. e461–7. doi: 10.1016/j.annemergmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Head injury: Triage, assessment, investigation and early management of head injury in infants, children, and adults. National Collaborative Centre for Acute Care and National Institute for Health and Clinical Excellence; [Accessed March 20, 2016]. http://www.nice.org.uk/nicemedia/pdf/CG56NICEGuideline.pdf. [Google Scholar]
- 16.Vos PE, Battistin L, Birbamer G, Gerstenbrand F, Potapov A, Prevec T, Stephan ChA, Traubner P, Twijnsra A, Vecsie L, von Wild K European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207–19. doi: 10.1046/j.1468-1331.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 17.Brewer ES, Reznikov B, Liberman RF, Baker RA, Rosenblatt MS, David CA, Flacke S. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J Trauma. 2011;70(1):E1–5. doi: 10.1097/TA.0b013e3181e5e286. [DOI] [PubMed] [Google Scholar]
- 18.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20. [PubMed] [Google Scholar]
- 19.Reynolds FD, Dietz PA, Higgins D, Whitaker TS. Time to deterioration of the elderly, anticoagulated, minor head injury patient who presents without evidence of neurologic abnormality. J Trauma. 2003;54(3):492–6. doi: 10.1097/01.TA.0000051601.60556.FC. [DOI] [PubMed] [Google Scholar]
- 20.Rockswold GL, Leonard PR, Nagib MG. Analysis of management in thirty-three closed head injury patients who “talked and deteriorated”. Neurosurgery. 1987;21(1):51–5. doi: 10.1227/00006123-198707000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Faul M, Xu L, Sasser SM. Hospitalized Traumatic Brain Injury: Low Trauma Center Utilization and High Interfacility Transfers among Older Adults. Prehosp Emerg Care. 2016:1–10. doi: 10.3109/10903127.2016.1149651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller SL, Miller S, Balon J, Helling TS. Medication reconciliation in a rural trauma population. Ann Emerg Med. 2008;52(5):483–91. doi: 10.1016/j.annemergmed.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Graham P, Bull B. Approximate standard errors and confidence intervals for indices of positive and negative agreement. J Clin Epidemiol. 1998;51(9):763–71. doi: 10.1016/s0895-4356(98)00048-1. [DOI] [PubMed] [Google Scholar]
- 24.Stiell IG, McKnight RD, Greenberg GH, Nair RC, McDowell I, Wallace GJ. Interobserver agreement in the examination of acute ankle injury patients. Am J Emerg Med. 1992;10(1):14–7. doi: 10.1016/0735-6757(92)90117-g. [DOI] [PubMed] [Google Scholar]
- 25.Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33(4):437–47. doi: 10.1016/s0196-0644(99)70309-4. [DOI] [PubMed] [Google Scholar]
- 26.Miller J, Lieberman L, Nahab B, Hurst G, Gardner-Gray J, Lewandowski A, Natsui S, Watras J. Delayed intracranial hemorrhage in the anticoagulated patient: A systematic review. J Trauma Acute Care Surg. 2015;79(2):310–3. doi: 10.1097/TA.0000000000000725. [DOI] [PubMed] [Google Scholar]
- 27.Nishijima DK, Offerman SR, Ballard DW, Vinson DR, Chettipally UK, Rauchwerger AS, Reed ME, Holmes JF Clinical Research in Emergency Services and Treatment (CREST) Network. Risk of traumatic intracranial hemorrhage in patients with head injury and preinjury warfarin or clopidogrel use. Acad Emerg Med. 2013;20(2):140–5. doi: 10.1111/acem.12074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans D, Pester J, Vera L, Jeanmonod D, Jeanmonod R. Elderly fall patients triaged to the trauma bay: age, injury patterns, and mortality risk. Am J Emerg Med. 2015;33(11):1635–8. doi: 10.1016/j.ajem.2015.07.044. [DOI] [PubMed] [Google Scholar]
- 29.Damlien L, Davidsen N, Nilsen M, Godo A, Moger TA, Viktil KK. Drug safety at admission to emergency department: an innovative model for PRIOritizing patients for MEdication Reconciliation (PRIOMER) Eur J Emerg Med. 2015 doi: 10.1097/MEJ.0000000000000355. forthcoming. [DOI] [PubMed] [Google Scholar]
- 30.Kessels RP. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–22. doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palacio AM, Kirolos I, Tamariz L. Patient values and preferences when choosing anticoagulants. Patient Prefer Adherence. 2015;9:133–8. doi: 10.2147/PPA.S64295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004;2(8):1247–55. doi: 10.1111/j.1538-7836.2004.00790.x. [DOI] [PubMed] [Google Scholar]
- 33.Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224–32. doi: 10.1016/s0196-0644(03)00823-0. [DOI] [PubMed] [Google Scholar]
- 34.Gorelick MH, Atabaki SM, Hoyle J, Dayan PS, Holmes JF, Holubkov R, Monroe D, Callahand JM, Kuppermann N Pediatric Emergency Care Applied Research Network. Interobserver agreement in assessment of clinical variables in children with blunt head trauma. Acad Emerg Med. 2008;15(9):812–8. doi: 10.1111/j.1553-2712.2008.00206.x. [DOI] [PubMed] [Google Scholar]
- 35.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543–9. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 36.Thompson WD, Walter SD. A reappraisal of the kappa coefficient. J Clin Epidemiol. 1988;41(10):949–58. doi: 10.1016/0895-4356(88)90031-5. [DOI] [PubMed] [Google Scholar]
- 37.Patel PA, Zhao X, Fonarow GC, Lytle BL, Smith EE, Xian Y, Bhatt DL, Peterson ED, Schwamm LH, Hernandez AF. Novel Oral Anticoagulant Use Among Patients With Atrial Fibrillation Hospitalized With Ischemic Stroke or Transient Ischemic Attack. Circ Cardiovasc Qual Outcomes. 2015;8(4):383–92. doi: 10.1161/CIRCOUTCOMES.114.000907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lurio J, Morrison FP, Pichardo M, Berg R, Buck MD, Wu W, Kitson K, Mostashari F, Calman N. Using electronic health record alerts to provide public health situational awareness to clinicians. J Am Med Inform Assoc. 2010;17(2):217–9. doi: 10.1136/jamia.2009.000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64(3):292–8. doi: 10.1016/j.annemergmed.2014.03.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.