Abstract
Background
Detailed recognition of the three-dimensional (3-D) deformity in acetabular dysplasia is important to help guide correction at the time of reorientation during periacetabular osteotomy (PAO). Common plain radiographic parameters of acetabular dysplasia are limited in their ability to characterize acetabular deficiency precisely. The 3-D characterization of such deficiencies with low-dose CT may allow for more precise characterization.
Questions/purposes
The purposes of this study were (1) to determine the variability in 3-D acetabular deficiency in acetabular dysplasia; (2) to define subtypes of acetabular dysplasia based on 3-D morphology; (3) to determine the correlation of plain radiographic parameters with 3-D morphology; and (4) to determine the association of acetabular dysplasia subtype with patient clinical characteristics including sex, range of motion, and femoral version.
Methods
Using our hip preservation database, we identified 153 hips (148 patients) that underwent PAO from October 2013 to July 2015. Among those, we noted 103 hips in 100 patients with acetabular dysplasia (lateral center-edge angle < 20°) and who had a Tönnis grade of 0 or 1. Eighty-six patients (86%) underwent preoperative low-dose pelvic CT scans at our institution as part of the preoperative planning for PAO. It is currently our standard to obtain preoperative low-dose pelvic CT scans (0.75–1.25 mSv, equivalent to three to five AP pelvis radiographs) on all patients before undergoing PAO unless a prior CT scan was performed at an outside institution. Hips with a history of a neuromuscular disorder, prior trauma, prior surgery, radiographic evidence of joint degeneration, ischemic necrosis, or Perthes-like deformities were excluded. Fifty hips in 50 patients met inclusion criteria and had CT scans available for review. These low-dose CT scans of 50 patients with symptomatic acetabular dysplasia undergoing evaluation for surgical planning of PAO were then retrospectively studied. CT scans were analyzed quantitatively for acetabular coverage, relative to established normative data for acetabular coverage, as well as measurement of femoral version. The cohort included 45 females and five males with a mean age of 26 years (range, 13–49 years).
Results
Lateral acetabular deficiency was present in all patients, whereas anterior deficiency and posterior deficiency were variable. Three patterns of acetabular deficiency were common: anterosuperior deficiency (15 of 50 [30%]), global deficiency (18 of 50 [36%]), and posterosuperior deficiency (17 of 50 [34%]). The presence of a crossover sign or posterior wall sign was poorly predictive of the dysplasia subtype. With the numbers available, males appeared more likely to have a posterosuperior deficiency pattern (four of five [80%]) compared with females (13 of 45 [29%], p = 0.040). Hip internal rotation in flexion was significantly greater in anterosuperior deficiency (23° versus 18°, p = 0.05), whereas external rotation in flexion was significantly greater in posterosuperior deficiency (43° versus 34°, p = 0.018). Acetabular deficiency pattern did not correlate with femoral version, which was variable across all subtypes.
Conclusions
Three patterns of acetabular deficiency commonly occur among young adult patients with mild, moderate, and severe acetabular dysplasia. These patterns include anterosuperior, global, and posterosuperior deficiency and are variably observed independent of femoral version. Recognition of these distinct morphologic subtypes is important for diagnostic and surgical treatment considerations in patients with acetabular dysplasia to optimize acetabular correction and avoid femoroacetabular impingement.
Introduction
Acetabular dysplasia is recognized as a common cause of hip pain in young adults and, in some patients, a cause of hip osteoarthritis later in life [13, 20]. Deficiency of the bony acetabulum results in hip instability and acetabular rim overload with subsequent damage to the labrum and articular cartilage [9]. Classic descriptions of acetabular dysplasia include anterosuperior acetabular deficiency. However, acetabular retroversion has been reported in approximately one in seven hips with dysplasia [12]. Symptomatic acetabular dysplasia is increasingly treated with periacetabular osteotomy (PAO) in an attempt to reorient the underlying acetabular coverage.
Precise understanding of the bony deficiency pattern is particularly important for accurate surgical correction of the underlying deformity. PAO is a well-established treatment for acetabular dysplasia with the ability to reorient the acetabulum in all three planes. Acetabular correction appears to play a role in the outcomes of PAO, but ideal targets for correction remain to be better defined. However, plain radiographs are limited in their ability to assess and characterize acetabular morphology [4]. Plain radiographic parameters, including the crossover sign and posterior wall sign, are commonly used to assess acetabular version. The crossover sign generally indicates acetabular retroversion but does not differentiate if this is the result of anterior overcoverage or posterior undercoverage. Zaltz et al. [21] demonstrated poor specificity of the crossover sign on plain radiographs for underlying acetabular retroversion. Similarly, Larson et al. [10] demonstrated that a crossover sign and posterior wall sign are common findings in “normal” hips. The posterior wall sign indicates posterior undercoverage but does not differentiate subtle undercoverage from severe undercoverage. Accurate and precise characterization of acetabular morphology remains important for guiding surgical reorientation of the dysplastic hip.
Three-dimensional (3-D) characterization of bony anatomy from MRI has traditionally been difficult. Only recently have techniques allowed for such modeling from MRI, but these techniques remain labor-intensive and not routinely available. Three-dimensional imaging with CT remains the gold standard for characterization of bony anatomy. Recent advances in low-dose CT imaging now allow for decreased radiation exposure, roughly equivalent to three to five (0.75–1.25 mSv) AP pelvis radiographs [14]. Normative data from CT have been recently reported for detailed regional acetabular coverage in normal asymptomatic populations [10]. The 3-D characterization of bony deficiency in acetabular dysplasia, however, has not yet been well defined.
The purposes of the current study were (1) to determine the variability in 3-D acetabular deficiency in acetabular dysplasia; (2) to define subtypes of acetabular dysplasia based on 3-D morphology; (3) to determine the correlation of plain radiographic parameters with 3-D morphology; and (4) to determine the association of acetabular dysplasia subtype with patient clinical characteristics including sex, range of motion (ROM), and femoral version.
Patients and Methods
Using our hip preservation database, we identified 153 hips (148 patients) that underwent PAO from October 2013 to July 2015. From that group, 103 hips in 100 patients had symptomatic (pain and functional limitations) acetabular dysplasia (lateral center-edge angle [LCEA] < 20°) and a Tönnis grade of 0 or 1 on plain AP pelvis radiography [4]. LCEA and acetabular inclination were measured on AP pelvis radiographs. Eighty-six of these patients (86%) underwent preoperative low-dose pelvic CT scans at our institution as part of the preoperative planning for PAO. Hips with a history of a neuromuscular disorder, prior trauma, prior surgery, radiographic evidence of joint degeneration, ischemic necrosis, Perthes-like deformities (large aspherical femoral head, a short femoral neck, and a high-riding greater trochanter) [9, 11], and inadequate imaging were excluded. In the cases of bilateral procedures, only the first surgical side was included. Fifty hips in 50 patients ultimately met inclusion criteria. It is currently our standard to obtain preoperative low-dose pelvic CT scans (0.75–1.25 mSv, equivalent to three to five AP pelvis radiographs) on all patients before undergoing PAO unless a prior CT scan was performed at an outside institution.
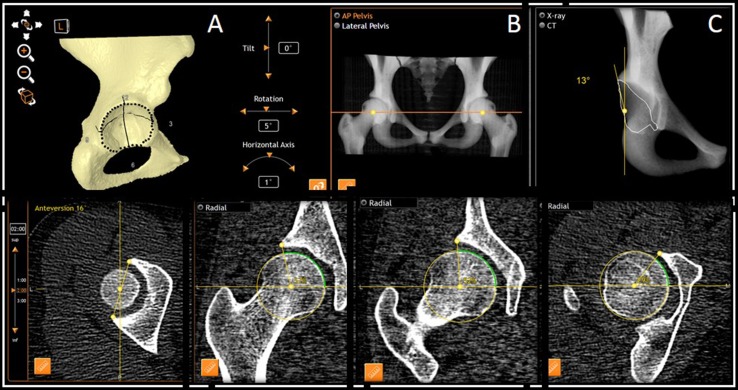
CT scans were analyzed using computer modeling software (Dyonics Plan Hip Impingement Planning System; Smith & Nephew, Andover, MA, USA). Acetabular coverage was assessed with pelvic rotation and obliquity corrected to a neutral position. Acetabular coverage was assessed with the pelvic tilt in its neutral supine resting position. Acetabular anatomy was characterized with a standard clockface position where the 3:00 position is anterior and corresponds to the psoas U indentation at this location (as well as the 6:00 position corresponding to the inferior margin of the acetabular fossa) [11]. Acetabular coverage was characterized with the measurement of radial coverage at each 15-minute clockface position from 9:00 to 12:00 to 3:00 (Fig. 1). Acetabular version was measured at the 1:00, 2:00, and 3:00 positions with the 1:00 position corresponding to cranial (superior) acetabular version and the 3:00 position to central acetabular version. Simulated AP pelvis radiographs were used for characterization of the presence of a crossover sign or posterior wall sign to remove the effect of alterations in pelvic tilt and rotation that are frequently present on AP pelvis radiographs. Femoral version was defined by the axis of the femoral neck and the posterior condylar axis of the knee. Femoral version was classified as increased anteversion (> 20°), normal anteversion (5°–20°), and relative retroversion (< 5°).
Fig. 1A–E.
Three-dimensional acetabular morphology characterization is shown at (A) acetabular rim points and (B) pelvic orientation; (C) characterization of presence or absence of crossover sign and posterior wall sign; (D) acetabular version measurement at 1:00, 2:00, and 3:00; and (E) radial acetabular coverage measurement; examples at 12:00, 1:00, and 3:00.
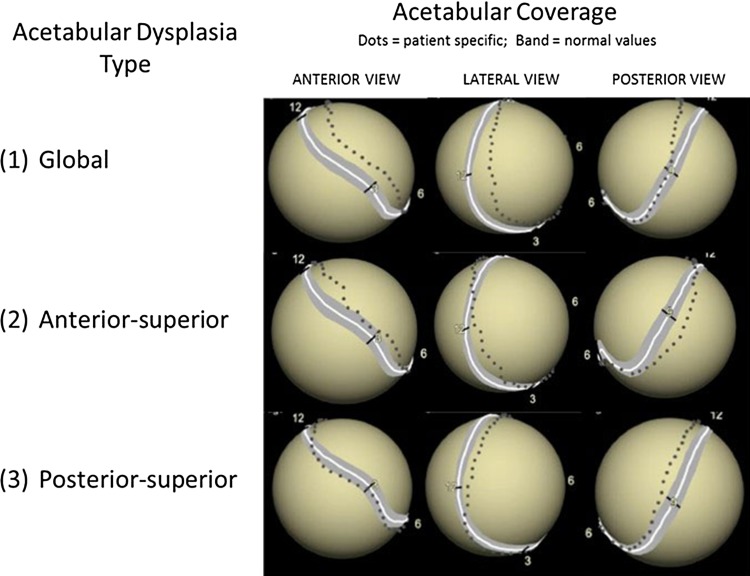
Acetabular deficiency was characterized by comparison of radial coverage values from 9:00 to 3:00 to normative data on acetabular coverage [8]. All measurements were performed by a single reader (JJN). The intraobserver reliability of all radiographic parameters was assessed in a subset of 10 patients with reads separated by greater than 2 weeks. All parameters had excellent intraobserver reliability (intraclass correlation coefficient range of parameters 0.8–1.0). The mean normative coverage ± 1 SD was considered normal. Coverage maps (Fig. 2) were used to identify regions of acetabular deficiency. Regions were defined as anterior (1:30–3:00), lateral (10:30–1:30), and posterior (9:00–10:30). Bony undercoverage was defined by three or more consecutive 15-minute locations with undercoverage within a region (Fig. 2).
Fig. 2.
Acetabular dysplasia subtype and 3-D coverage case examples identify regions of acetabular deficiency. Regions were defined as anterior (1:30–3:00), lateral (10:30–1:30), and posterior (9:00–10:30). Bony undercoverage was defined by three or more consecutive 15-minute locations with undercoverage.
We defined three subtypes of acetabular dysplasia based on patterns observed: anterosuperior (AS) deficiency, global (G) deficiency, and posterosuperior (PS) deficiency. Characterization of the regions of maximal acetabular deficiency was used for classification. Hips with anterosuperior deficiency had primarily undercoverage anteriorly and laterally. Hips with global deficiency had lateral undercoverage with variable degrees of, but similar, anterior and posterior undercoverage. Hips with posterosuperior deficiency had undercoverage primarily laterally and posteriorly.
The mean age of patients in the cohort was 26 years (range, 13–49 years). The cohort included 60% right hips (n = 30) and 40% left hips (n = 20). Ninety percent (n = 45) of hips were in female patients, whereas five (10%) were in male patients. The mean LCEA was 14° ± 5°, whereas the mean acetabular inclination was 16° ± 5°. A positive crossover sign was present in 13 of 50 (26%) hips, whereas a positive posterior wall sign was present in 26 of 50 (52%). The mean femoral version was 19° ± 13°. Increased femoral anteversion (> 20°) was present in 17 of 50 (34%), whereas relative femoral retroversion (< 5°) was present in seven of 50 (14%). The mean femoral neck-shaft angle was 137° ± 6°. Clinical hip ROM was recorded by a single surgeon (JCC) at the time of preoperative evaluation, including internal rotation in 90° of flexion (IRF) and external rotation in 90° of flexion (ERF). Twenty-three hips (46%) had mild acetabular dysplasia, whereas 27 hips (54%) had moderate to severe dysplasia. Twenty-three hips (46%) had an acetabular inclination ≤ 15°, whereas 27 hips (54%) had an acetabular inclination > 15°. Overall, 34% of hips had a LCEA < 15° and acetabular inclination > 15°.
Univariate statistical analysis was used to compare continuous and categorical variables between dysplasia subtypes. Chi-square test was used to compare categorical variables (or Fisher’s exact test). Student’s t-test (two groups) or one-way analysis of variance (more than two groups) was used to compare continuous variables between groups. A p value < 0.05 was considered significant.
Results
Lateral acetabular deficiency was present in all patients (relative to normative coverage), whereas anterior deficiency and posterior deficiency were variable. Radial coverage at 12:00 averaged 17° ± 5°. Acetabular version at the 1:00, 2:00, and 3:00 positions averaged 5°, 10°, and 18°, respectively. Cranial acetabular retroversion (< 0° at 1:00) was present in 11 of 50 (22%) hips. Anterior acetabular deficiency was present in 32 of 50 hips (64%), whereas posterior acetabular deficiency was present in 34 of 50 hips (68%).
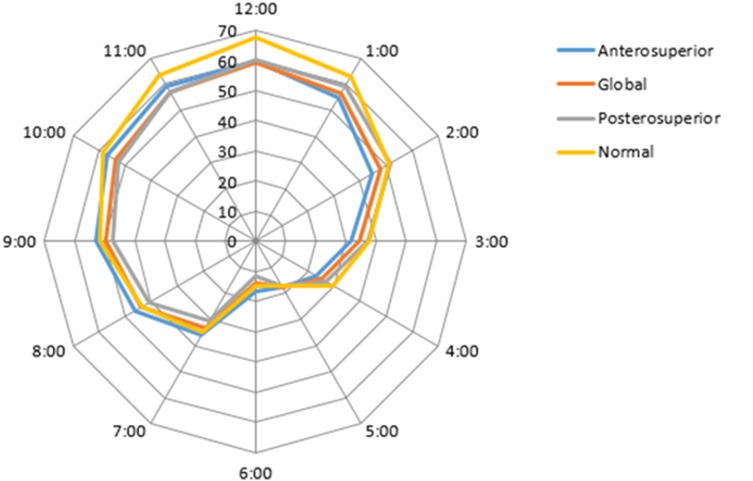
Acetabular deficiency was subclassified as global deficiency in 18 of 50 (36%) hips, anterosuperior deficiency in 15 of 50 hips (30%), and posterosuperior deficiency in 17 of 50 hips (34%) (Table 1; Fig. 1). Radial coverage values of the 9:00 posterior to 3:00 anterior positions varied by subtype of acetabular dysplasia (Table 2; Fig. 3). Hips with anterosuperior deficiency had less coverage from the 1:00 to 3:00 positions (all p < 0.002) while having greater coverage at the 9:00 to 11:00 (all p < 0.001) positions compared with other hips (Table 2). Hips with posterosuperior deficiency had more coverage from the 1:00 to 3:00 positions while having less coverage at the 9:00 to 10:00 (all p < 0.001) positions compared with other hips (Table 2).
Table 1.
Acetabular dysplasia subtype and dysplasia severity
| Acetabular dysplasia subtype | Total (n = 50) |
Mild dysplasia (LCEA 15°-20°) (n = 23) |
Moderate to severe dysplasia (LCEA < 15°) (n = 27) |
Male (n = 5) |
Female (n = 45) |
|---|---|---|---|---|---|
| Anterosuperior deficiency | 15/50 (30%) | 6/23 (26%) | 9/27 (33%) | 0/5 (0%) | 15/45 (33%) |
| Global deficiency | 18/50 (36%) | 7/23 (30%) | 11/27 (41%) | 1/5 (20%) | 17/45 (38%) |
| Posterosuperior deficiency | 17/50 (34%) | 10/23 (43%) | 7/27 (26%) | 4/5 (80%)* | 13/ (29%)* |
* p = 0.040 Fisher’s exact test; LCEA = lateral center-edge angle.
Table 2.
Radial acetabular coverage by acetabular dysplasia subtype
| Acetabular coverage by clockface (%)† |
Total (n = 50) |
Anterosuperior deficiency (n = 15) |
Global deficiency (n = 18) |
Posterosuperior deficiency (n = 17) |
|---|---|---|---|---|
| 9:00 (posterior) | 50 ± 3 | 53 ± 2* | 50 ± 2 | 47 ± 2* |
| 10:00 | 55 ± 3 | 57 ± 2* | 54 ± 3 | 53 ± 4* |
| 11:00 | 58 ± 3 | 59 ± 2* | 57 ± 4 | 57 ± 2 |
| 12:00 | 60 ± 3 | 59 ± 2 | 59 ±3 | 60 ± 3 |
| 1:00 | 57 ± 3 | 55 ± 3* | 57 ± 3 | 59 ± 2* |
| 2:00 | 48 ± 4 | 45 ± 2* | 48 ± 3 | 51 ± 3* |
| 3:00 (anterior) | 34 ± 3 | 31 ± 3* | 34 ± 3 | 37 ± 2* |
* p < 0.05; †values indicate femoral head coverage percentage at each clockface position.
Fig. 3.
Mean radial acetabular coverage by acetabular dysplasia subtype demonstrates the radial coverage of the three acetabular dysplasia subtypes relative to normal. Acetabular coverage was characterized with the measurement of radial coverage at each 15-minute clockface position from 9:00 to 12:00 to 3:00.
The presence or absence of a radiographic crossover sign (7% AS, 22% G, 47% PS; p = 0.031) and posterior wall sign (20% AS, 44% G, 88% PS; p < 0.001) was associated with acetabular dysplasia subtype (Table 3). However, these radiographic findings poorly predicted underlying dysplasia subtype with a crossover sign and posterior wall sign both most commonly present in posterosuperior deficiency but occurring in all three subtypes. Anterosuperior deficiency most commonly had a negative crossover sign and negative posterior wall sign (80% [12 of 15]). Global deficiency most commonly had a negative crossover sign with a negative (44% [eight of 18]) or positive (33% [six of 18]) posterior wall sign. Posterosuperior deficiency most commonly had a negative posterior wall sign with a negative (47% [eight of 17]) or positive (41% [seven of 17]) crossover sign. No difference in dysplasia subtype was present between different severities of acetabular dysplasia. Hips with acetabular inclination greater than 15° most commonly were classified as anterosuperior deficiency (41% [11 of 27]), whereas hips with acetabular inclination ≤ 15° were most commonly classified as posterosuperior deficiency (48% [11 of 23]) (p = 0.097).
Table 3.
Acetabular parameters by acetabular dysplasia subtype
| Radiographic parameter | Total (n = 50) |
Anterosuperior deficiency (n = 15) |
Global deficiency (n = 18) |
Posterosuperior deficiency (n = 17) |
p value |
|---|---|---|---|---|---|
| Crossover sign | 13/50 (26%) | 1/15 (7%) | 4/18 (22%) | 8/17 (47%) | 0.031 |
| Posterior wall sign | 26/50 (52%) | 3/15 (20%) | 8/18 (44%) | 15/17 (88%) | < 0.001 |
| Acetabular version at clockface position | |||||
| 1:00 | 5° | 10° ± 6° | 5° ± 7° | −1° ± 6° | < 0.001 |
| 2:00 | 10° | 15° ± 3° | 10° ± 3° | 5° ± 4° | < 0.001 |
| 3:00 | 18° | 22° ± 3° | 18° ± 3° | 14° ± 3° | < 0.001 |
| Femoral version | 19° | 21° ± 10° | 17° ± 14° | 20° ± 14° | 0.607 |
| < 5° | 19/50 (38%) | 5/15 (33%) | 9/18 (50%) | 5/17 (29%) | 0.524 |
| 5°–20° | 14/50 (28%) | 6/15 (40%) | 3/18 (17%) | 5/17 (29%) | |
| > 20° | 17/50 (34%) | 4/15 (27%) | 6/18 (33%) | 7/17 (41%) |
Posterosuperior deficiency was present in four of five males (80%; 95% confidence interval [CI], 44%–100%) compared with 13 of 45 females (29%; 95% CI, 15%–42%; p = 0.040 Fisher’s exact test). No difference in pattern of acetabular deficiency was present between hips with mild versus moderate to severe dysplasia (Table 1). With the numbers available, we did not see any difference in posterosuperior acetabular deficiency between the mildly and the moderately to severely dysplastic hips (44% versus 26%, p = 0.192). No difference in femoral version was observed with the numbers available among the three subtypes of acetabular dysplasia. Hip IRF was greater in hips with anterosuperior deficiency compared with other patterns (23° ± 8° versus 18° ± 9°, p = 0.05). Hip ERF was greater in hips with global deficiency compared with other patterns (43° ± 12° versus 34° ± 15°, p = 0.018).
Discussion
An understanding of the pattern of bony deficiency of hips with acetabular dysplasia is important to optimize the accuracy and precision of bony reorientation. The current study characterizes 3-D deformity in hips with acetabular dysplasia relative to normative acetabular coverage. Hips with mild, moderate, and severe acetabular dysplasia demonstrate variable patterns of acetabular deficiency and version. Three patterns of acetabular deficiency are present in roughly similar proportions and include anterosuperior deficiency, global deficiency, and posterosuperior deficiency. Patterns of acetabular deficiency appear to be associated with sex (posterosuperior deficiency is more common among males) and other clinical characteristics (differences in hip IRF and ERF between acetabular deficiency patterns) while not being associated with femoral version.
The current study has several limitations. The sample size of 50 hips limits the precision of estimates of the prevalence of dysplasia subtype and the power of statistical comparisons between smaller subgroups. Males with acetabular dysplasia are less common than females with only five patients in the current study. The current study provides some data in this male subgroup, but larger studies are needed to better characterize this subgroup. However, the current sample size does allow for adequate demonstration of the variability of coverage patterns and allows estimates of the prevalence of disease patterns. Additionally, it is possible that other patterns of acetabular deficiency exist but were not present in the current cohort. Radiographic CT measurements in the current study were performed by a single individual and excellent intraobserver reliability was demonstrated in a subset of patients. Interobserver reliability may be less and could result in differences in the current data, but the computer-assisted nature of CT measurements in the current software would make this less likely. Acetabular morphology has been demonstrated to be influenced by pelvic position [16, 17]. In the current study, acetabular morphology was analyzed in its supine state rather than using correction to the anterior pelvis plane or correction to the standing position. This supine position allows for the most similar comparisons to previous literature on the morphology of the dysplastic hip.
In this initial study, we describe the variation in acetabular deficiency that occurs between hips including deficiency in the anterior, lateral, and posterior locations. The increased recognition and treatment of symptomatic acetabular dysplasia in the young adult underscore the importance of accurate deformity characterization in this population. Overcorrection of acetabular dysplasia with PAO has been shown to potentially result in restricted ROM and iatrogenic femoroacetabular impingement. Variability in the acetabular morphology in dysplastic hips has been previously investigated with early investigation focused on consequences for THA [3, 15]. Cranial (superior) acetabular retroversion has been reported to be present in 17% of dysplastic hips [6, 12]. Li and Ganz [12] noted the importance of assessment of cranial acetabular retroversion rather than central retroversion, which would often appear normal. In their study (based on plain radiographs), patterns of deficiency observed were most commonly anterolateral deficiency, but they also observed isolated anterior, lateral, and posterolateral deficiency patterns.
Tannast et al. also demonstrated high variability of acetabular coverage in dysplastic hips based on plain radiographs [18]. Their study reported three different morphologic subtypes of acetabular deficiency: anterior deficiency in 56%, global deficiency in 33%, and posterior deficiency in 11%. Several studies have previously characterized the dysplastic acetabulum on CT [1, 2, 5, 7, 19]. Anda et al. [2] investigated the acetabular morphology in hip dysplasia with CT and reported anterior deficiency in two-thirds and posterior deficiency in one-third. Akiyama et al. [1] reported the CT characterization of acetabular dysplasia and subclassified as anterior, global, or posterior deficiency based on the anterior and posterior acetabular sector angle. van Bosse et al. [19] recently reported the 3-D characterization of 48 dysplastic hips. They characterized the elongated nature of the dysplastic morphology and identified mean differences between dysplastic and normal hips, but did not identify patterns of deformity in subgroups of dysplastic hips. Haddad et al. [7] previously reported the variability of acetabular deficiency in 10 dysplastic hips that used radial coverage analysis similar to the current study.
In our current classification, a hip is characterized based on the predominant pattern of dysplasia rather than the isolated presence of dysplasia of any severity at several locations. A hip with moderate to severe anterior and lateral deficiency with mild posterior deficiency is classified as anterosuperior deficiency in the current study while likely labeled global deficiency in previous classifications. Recognition of the primary pattern of underlying deficiency may best guide the acetabular reorientation to normalize acetabular coverage. In the current study, global deficiency and posterosuperior deficiency were present as commonly as classic anterosuperior deficiency. The posterior coverage in hips with anterosuperior deficiency was similar to normal controls (Table 2). The anterior coverage in hips with anterosuperior deficiency was similar to normal controls (Table 2). These subtypes generally correlate with underlying acetabular version including anterosuperior (anteversion), global (neutral version), and posterosuperior (retroversion) deficiency.
Plain radiographic parameters including dysplasia severity by LCEA or acetabular inclination as well as the crossover sign and posterior wall sign were not highly predictive of underlying acetabular dysplasia subtype. Thus, the subtype of acetabular dysplasia was not able to be accurately characterized with these radiographic parameters. Low-dose CT may play a role in preoperative planning in the setting of acetabular dysplasia to maximize deformity correction at the time of PAO. More precise characterization of anterior and posterior wall morphology on plain radiographs beyond the crossover sign and posterior wall sign may improve the ability of plain radiographs and intraoperative fluoroscopy to identify acetabular dysplasia subtypes; however, further investigation is needed to determine the potential benefit.
Acetabular dysplasia subtype was associated with several factors. Despite only having a small number of males in the current cohort, male sex was associated with the presence of posterosuperior acetabular deficiency (present in 80% of hips). Despite the small numbers in this subgroup, the difference was statistically significant with larger but nonoverlapping confidence intervals. Larger cohorts of male patients with dysplasia are needed to more accurately characterize the prevalence of this pattern of dysplasia. Femoral version was not associated with the acetabular deficiency pattern and was variable in all patterns (Table 3). Additionally, hip rotational ROM was correlated with acetabular deficiency pattern with anterosuperior deficiency having higher IRF and global deficiency having higher ERF. This finding in the setting of no difference in femoral version would suggest the ROM is primarily the result of the acetabular morphology. In the current study, femoral version was variable across all three acetabular dysplasia subtypes and demonstrated no differences between groups. Clearly other factors such as femoral version, capsular laxity, and proximal femoral morphology play a role in ROM. This highlights the consideration for femoroacetabular impingement in hips with posterosuperior deficiency in which the anterior acetabular coverage may be normal and approximately 30% of hips have relative femoral retroversion. This further emphasizes the need for further comprehensive characterization of anatomy including the preoperative anatomy and consideration for surgical correction.
Lateral acetabular deficiency was consistently present in hips with acetabular dysplasia, whereas anterior deficiency and posterior deficiency were variables. Three patterns of acetabular deficiency were common: anterosuperior deficiency (30%), global deficiency (36%), and posterosuperior deficiency (34%). Patterns of acetabular deficiency, however, do not correlate with femoral version. An understanding of acetabular dysplasia subtype is important to the underlying hip pathophysiology and considerations for precise surgical reorientation. Recognition of the underlying pattern of acetabular dysplasia may assist in planning acetabular reorientation and recognition of reduction maneuvers to optimize acetabular position to avoid overcoverage resulting in femoroacetabular impingement or undercoverage resulting in persistent instability.
Footnotes
Each author certifies that he, or a member of his immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Washington University School of Medicine, St Louis, MO, USA.
Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
References
- 1.Akiyama M, Nakashima Y, Fujii M, Sato T, Yamamoto T, Mawatari T, Motomura G, Matsuda S, Iwamoto Y. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol. 2012;41:1411–1418. doi: 10.1007/s00256-012-1368-7. [DOI] [PubMed] [Google Scholar]
- 2.Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr. 1991;15:115–120. doi: 10.1097/00004728-199101000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Argenson J-NA, Flecher X, Parratte S, Aubaniac J-M. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–45. [DOI] [PubMed]
- 4.Clohisy JC, Carlisle JC, Beaulé PE, Kim Y-J, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90:1428–1434. doi: 10.1302/0301-620X.90B11.20073. [DOI] [PubMed] [Google Scholar]
- 6.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 7.Haddad FS, Garbuz DS, Duncan CP, Janzen DL, Munk PL. CT evaluation of periacetabular osteotomies. J Bone Joint Surg Br. 2000;82:526–531. doi: 10.1302/0301-620X.82B4.10174. [DOI] [PubMed] [Google Scholar]
- 8.Janzen DL, Aippersbach SE, Munk PL, Sallomi DF, Garbuz D, Werier J, Duncan CP. Three-dimensional CT measurement of adult acetabular dysplasia: technique, preliminary results in normal subjects, and potential applications. Skeletal Radiol. 1998;27:352–358. doi: 10.1007/s002560050397. [DOI] [PubMed] [Google Scholar]
- 9.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 10.Larson CM, Moreau-Gaudry A, Kelly BT, Byrd JWT, Tonetti J, Lavallee S, Chabanas L, Barrier G, Bedi A. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473:1247–1254. doi: 10.1007/s11999-014-4055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee WA, Saroki AJ, Loken S, Trindade CAC, Cram TR, Schindler BR, LaPrade RF, Philippon MJ. Radiographic identification of arthroscopically relevant acetabular structures. Am J Sports Med. 2016;44:67–73. doi: 10.1177/0363546515612083. [DOI] [PubMed] [Google Scholar]
- 12.Li PLS, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 13.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Nepple JJ, Martel JM, Kim Y-J, Zaltz I. Clohisy JC; ANCHOR Study Group. Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res. 2012;470:3313–3320. doi: 10.1007/s11999-012-2510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40. [PubMed] [Google Scholar]
- 16.Ross J, Nepple J, Philippon M, Kelly B, Larson C, Bedi A. The influence of pelvic tilt on common acetabular parameters and range of motion in patients with femoroacetabular impingement (FAI) Arthroscopy. 2013;29:e203. doi: 10.1016/j.arthro.2013.09.044. [DOI] [Google Scholar]
- 17.Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med. 2014;42:2402–2409. doi: 10.1177/0363546514541229. [DOI] [PubMed] [Google Scholar]
- 18.Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2014;473:1234–1246. doi: 10.1007/s11999-014-4038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Bosse H, Wedge JH, Babyn P. How are dysplastic hips different? A three-dimensional CT study. Clin Orthop Relat Res. 2014;473:1712–1723. doi: 10.1007/s11999-014-4103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76. [PubMed] [Google Scholar]
- 21.Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2463–2470. doi: 10.1007/s11999-012-2689-5. [DOI] [PMC free article] [PubMed] [Google Scholar]