Abstract
Background:
The analgesic benefit of transversus abdominis plane (TAP) blocks for cesarean delivery remains controversial. In our study, we compared the analgesic efficacy of TAP block using local anesthetic bupivacaine and adjunct fentanyl with bupivacaine alone in patients undergoing elective cesarean section.
Methods:
Our study was a randomized, double-blind, controlled clinical trial where sixty patients undergoing elective cesarean delivery under subarachanoid block (2 ml of 0.5% bupivacaine) were randomized into two groups, A and B. At the end of the surgical procedure, bilateral TAP block was performed guided by the ultrasound. Group A received 38 ml of 0.25% bupivacaine and 2 ml of 50 μg of fentanyl, whereas Group B received 38 ml of 0.25% bupivacaine + 2 ml of normal saline. The total volume was divided equally and administered bilaterally. Each patient was assessed for 24 h after TAP block, for time to rescue analgesia, pain using visual analog scale (VAS) score at rest and on movement, hemodynamic parameters (heart rate and blood pressure), nausea, vomiting, and sedation. Diclofenac 75 mg was given as rescue analgesia when the patient complained of pain or when VAS score >4.
Results:
Prolonged postoperative analgesia was noticed with both the groups, with a mean time to rescue analgesia of approximately 6.5 h. There was no significant difference in time to rescue analgesia (6.49 ± 0.477 vs. 6.5 ± 0.480) when both the groups were compared among themselves. The pain scores among the two groups when compared did not show any added benefit. Incidence of nausea, vomiting, and sedation when compared between both the groups showed no difference.
Conclusion:
The TAP block as a part of a multimodal analgesic regimen definitely has a role in providing superior analgesia in the postoperative period. However, adjunct fentanyl to local anesthetic bupivacaine was found to have no added advantage when quality and duration of analgesia was compared.
Keywords: Fentanyl adjuvant, postlower segment cesarean section, transversus abdominis plane block
INTRODUCTION
There is a gradual rise in the number of cesarean sections performed worldwide. It is a global trend and accounts for more than one-fourth of all births worldwide.[1,2] This makes cesarean section one of the commonly performed surgical procedures. Substantial pain and distress is anticipated following a major surgical procedure such as cesarean section. Effective postoperative pain management is of particular importance in this subgroup to facilitate early ambulation, infant care, and maternal-infant bonding.[3]
An important component of pain and discomfort is expected from the abdominal wall incision.[4] Regional anesthetic techniques such as local anesthetic infiltration, ilioinguinal nerve blocks, abdominal field blocks, and transversus abdominis plane (TAP) blocks have been described to alleviate pain from the abdominal wall incision.
The anterolateral abdominal wall is innervated by thoraco-lumbar nerves T7 to L1 which traverse through the plane between the layers of the transversus abdominis and internal oblique muscles.[5] TAP block was first described by Rafi in 2001. TAP block is a regional anesthetic technique in which a local anesthetic agent is deposited in the TAP to block the sensory nerves supplying the anterior abdominal wall.[6] The TAP block has shown considerable analgesic benefit compared to placebo in numerous prospective randomized controlled trials for cesarean section.[7] Most studies compared TAP block with systemic or oral analgesics, and some studies compared different percentages of local anesthetics (LA) used in the TAP block. Only a few studies have studied adjuncts to LA in TAP block. Fentanyl, an opioid, has been used as an adjunct in subarachnoid blocks. Several studies have shown that the addition of fentanyl to local anesthetic improves the quality of analgesia and prolongs the duration of subarachnoid block.[8]
Our study was conducted to compare the efficacy of adjunct fentanyl in TAP block based on the hypothesis that fentanyl when administered along with bupivacaine will improve the quality of postoperative analgesia and also prolongs the duration of blockade.
METHODS
After obtaining Ethical and Institutional Committee clearance, American Society of Anesthesiologists Classes I–II patients, scheduled to undergo elective lower segment cesarean section, were recruited into this prospective randomized double-blinded controlled trial. Written informed consent was obtained from patients before inclusion in this study. Patients with history of allergy to local anesthetic drug, infection at the site of block placement, coagulopathy, history of neurologic or psychiatric disease, history of active liver or renal disease, or patient refusing to participate in the study were excluded from study groups. Patients were randomized into two groups of thirty each: Group A (38 ml of 0.25% bupivacaine + 2 ml of 50 µg fentanyl) and Group B (38 ml of 0.25% bupivacaine + 2 ml of normal saline). Preanesthetic assessment was done prior to surgery. Written informed consent was obtained after explaining the procedure to the patients in the language they understood. Patients were shifted to operation theatre (O.T) complex. Noninvasive monitors such as electrocardiogram, noninvasive blood pressure, and pulse oximeter were connected. Intravenous (iv) access was established using 18-gauge iv cannula and infusion of crystalloids (Ringer's Lactate) was started. All patients received subarachnoid block with 2 ml of 0.5% bupivacaine (heavy). Patients were randomly allocated to undergo TAP block (Group A) with either 38 ml of 0.25% bupivacaine + 50 µg of fentanyl or TAP block (Group B) with 38 of 0.25% bupivacaine + 2 ml of normal saline at the end of surgical procedure. Total volume was divided into two equal doses (20 ml each) to be administered on either side. The allocation sequence was generated by random number table. The patient, anesthesiologist, and staff providing postoperative care were blinded to group assignment. Both the groups also received prophylactic anti emetic ondansetron 4 mg iv. Qualified anesthesiologist who is trained in ultrasound-guided nerve block performed all TAP blocks. Full aseptic precautions were observed and a Sonosite portable ultrasound machine with 5 cm high-frequency linear array probe was utilized. The probe was positioned transverse to the abdomen in the mid-axillary line between the lower border of the ribs and the iliac crest. The external oblique, internal oblique, transversus abdominis muscles, and the transversus abdominis fascia were visualized. Under continuous in-plane ultrasound guidance, a 22 g 100 mm Stimuplex needle was inserted between internal oblique and transversus abdominis muscles into the posterior aspect of the fascial plane. After negative aspiration and distension of the fascial plane by hydro dissection, 20 mL of the study solution was injected under ultrasound guidance. This procedure was repeated on the contralateral side of the abdomen with the remaining 20 mL of study solution. After completion of the block, the patients were shifted out of the O.T. Diclofenac 75 mg intramuscular was given as rescue analgesic at request of the patient, and time to rescue analgesic was noted. Total dose of diclofenac used in 24 h was also noted. Hemodynamic parameters were assessed for 24 h from the time of administration of block at 0, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h intervals. Pain both at rest and at movement using visual analog scale (0–10; 0 = no pain, 10 = max pain) was also assessed. The severity of nausea was assessed by a categorical scale (0 = none, 1 = mild, 2 = moderate, 3 = severe). Sedation was assessed using 4-point sedation scale: 0 = awake and alert, 1 = sleepy but responding to verbal commands, 2 = asleep but still arousable, 3 = deep sleep.
Statistical analysis
Data were analyzed using SPSS (Statistical Package for Social Sciences); computer software version 18 (SPSS Inc., Chicago, IL, USA). Continuous variables were analyzed using independent t-test. For comparing proportion between two groups, Chi-square test was applied and a P < 0.05 was considered significant.
RESULTS AND OBSERVATIONS
Sixty patients were recruited in the study, of these thirty were randomized to undergo TAP block with 0.25% bupivacaine 38 ml + 2 ml of normal saline and remaining thirty with 38 ml of 0.25% bupivacaine + 2 ml of 50 µg fentanyl.
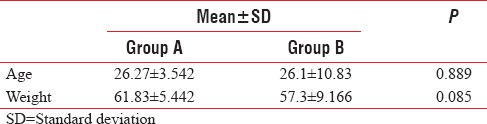
The distribution of age and weight among the two groups were comparable [Table 1].
Table 1.
Mean age and weight of Groups A and B
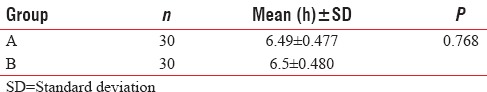
Comparison of time to rescue analgesia
Time to rescue analgesia was the primary outcome in our study. The mean time (in hours) to rescue analgesia was found to be 6.49 ± 0.477 and 6.5 ± 0.480 for Groups A and B, respectively. T-test was used to test the significant difference of mean time between the two groups. Groups A and B when compared the difference in mean time to rescue analgesia was not statistically significant [Table 2].
Table 2.
Mean time to rescue analgesia in h
Comparison of pain score at rest
The table below shows mean pain scores at rest between the Groups A and B. On comparing the mean pain scores between the two groups, the results obtained had no statistical significance, thus showing that Groups A and B had similar pain scores at 0, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h [Table 3].
Table 3.
Mean pain scores at rest 0, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h
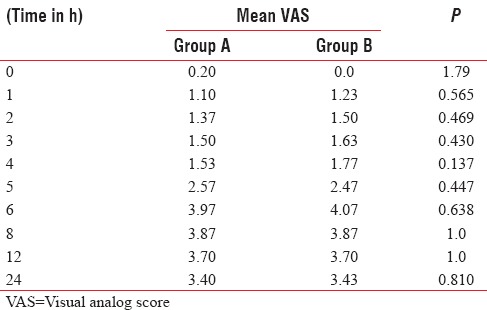
Figure 1 shows the mean pain scores on movement between the Groups A and B. On comparing the mean pain scores between the two groups, the results obtained had no statistical significance, thus showing that Groups A and B had similar pain scores at 0, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h.
Figure 1.
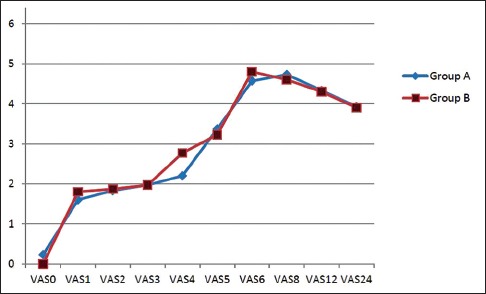
Mean pain scores on movement at 0, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h.
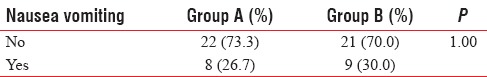
The incidence of nausea and vomiting was compared among the two groups. The difference was not statically significant [Table 4].
Table 4.
Incidence of nausea and vomiting in the two groups
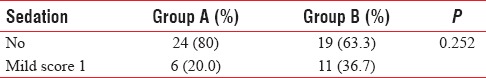
The sedation scores of the two groups were compared. It was found that all the patients who were sedated had only a score of 1, i.e., mild sedation. Hence, the patients could be placed into two groups, either mildly sedated or not sedated at all. The difference was not statistically significant [Table 5].
Table 5.
Incidence of sedation in percentage
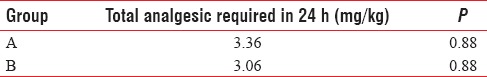
Comparison of total analgesic requirement
The amount of diclofenac consumed in 24 h by both the groups was compared. It was found that in both the groups, total analgesic requirement did not show any statistical significance [Table 6].
Table 6.
Analgesic requirement in both the groups
DISCUSSION
TAP block is a relatively new regional anesthetic technique, in which neural afferents supplying the anterolateral abdominal wall are blocked by introducing a local anesthetic in the TAP.[6] TAP block as a part of postoperative multimodal analgesic regimen is slowly gaining popularity. Its potential in enhancing quality and duration of analgesia following various lower abdominal surgeries is well established.[9] Our study proved that TAP block prolonged duration of analgesia (~6.5 h) as was evident from standard studies. But when both the groups were compared for the mean time to rescue analgesia, there was no significant difference in the time to rescue analgesia between the two groups. This probably suggests that addition of fentanyl to bupivacaine in the TAP block did not have any added benefit in prolonging analgesia. Similar finding was noticed in a study done by Bollag et al. where they used clonidine as an adjunct to bupivacaine in the TAP block for postoperative analgesia in elective cesarean section.[10]
Fentanyl as an adjunct to LA in TAP block has not been evaluated. Though fentanyl has had a definitive role as an adjunct to LA in neuraxial blocks, in almost all studies, it invariably improved the quality as well as duration of the blockade.[11] In animals, the presence of peripheral opioid receptors has been reported; however, it is quite unclear whether functional opioid receptors exist in human peripheral tissue.[12,13,14] Several studies have attempted to determine whether functional opioid receptors exists in human peripheral tissue. Role of fentanyl as an adjunct to local anesthetic in peripheral blocks is controversial. Some of the studies concluded there were significant improvement in duration of analgesia like in subarachnoid blocks, while others were of the opinion that opioids have no effect when used as an adjunct in peripheral nerve blocks. Fletcher et al. were of the opinion that the addition of fentanyl to lidocaine with adrenaline (1:200,000) for axillary plexus block produced no clinical effects. Racz et al.[15] were also of the opinion that addition of morphine to local anesthetic (mixture of lidocaine and bupivacaine) for axillary brachial plexus block changed neither the onset nor the quality or duration of block. While studies by Karakaya et al. and Nishikawa et al. showed significant increase in duration of action with the fentanyl group.[16,17] The possible mechanism of action of fentanyl at peripheral level could be three. First, fentanyl could have direct action on the peripheral receptors. Second, fentanyl could have diffused to epidural and subarachnoid spaces from the brachial plexus sheath (brachial plexus block) to produce its effect. Third, peripheral uptake of fentanyl into systemic circulation.[12]
The results of our study were comparable to those of a study by Fletcher et al. They evaluated the effects of additive fentanyl to lidocaine in axillary brachial plexus block, in patients scheduled for orthopedic surgeries of the fore arm. They concluded that the addition of fentanyl to local anesthetic had no clinical benefit in axillary brachial plexus block.[18]
The mean requirement of diclofenac in 24 h in group A was around 3.3 mg/kg body weight and Group B was around 3.06 mg/kg body weight. Both the groups required approximately the same amount of diclofenac, again signifying that fentanyl added to bupivacaine in TAP block had no analgesic benefit. Opioids are known to produce nausea, vomiting and sedation. However, in our study groups, the incidence of both nausea and sedation were insignificant. This probably suggests that fentanyl when administered as an adjunct to local anesthetic in TAP block had only minimal systemic absorption to cause central activation of the opioid receptors.
CONCLUSION
The TAP block as a part of a multimodal analgesic regimen definitely has a role in providing superior analgesia in the postoperative period. However, adjunct fentanyl to local anesthetic bupivacaine was found to have no added advantage when quality and duration of analgesia was compared.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21:98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- 2.Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, Bergel E. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: An ecological study. Birth. 2006;33:270–7. doi: 10.1111/j.1523-536X.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 3.Faragher RA. Post-Operative Pain Management Following Caesarean Delivery. 1st ed. Philadelphia PA: Saunders Elsevier; 2006. pp. 225–38. [Google Scholar]
- 4.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 5.Netter FH. Back and spinal cord. In: Netter FH, editor. Atlas of Human Anatomy. Summit, New Jersey: The Ciba-Geigy Corporation; 1989. pp. 145–55. [Google Scholar]
- 6.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 7.Ismail S. Multimodal analgesia for cesarean section: Evolving role of transversus abdominis plane block. J Obstet Anaesth Crit Care. 2012;2:67–8. [Google Scholar]
- 8.Hunt CO, Naulty JS, Bader AM, Hauch MA, Vartikar JV, Datta S, et al. Perioperative analgesia with subarachnoid fentanyl-bupivacaine for cesarean delivery. Anesthesiology. 1989;71:535–40. doi: 10.1097/00000542-198910000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Amr YM, Amin SM. Comparative study between effect of pre- versus post-incisional transversus abdominis plane block on acute and chronic post-abdominal hysterectomy pain. Anesth Essays Res. 2011;5:77–82. doi: 10.4103/0259-1162.84199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bollag L, Richebe P, Siaulys M, Ortner CM, Gofeld M, Landau R. Effect of transversus abdominis plane block with and without clonidine on post-cesarean delivery wound hyperalgesia and pain. Reg Anesth Pain Med. 2012;37:508–14. doi: 10.1097/AAP.0b013e318259ce35. [DOI] [PubMed] [Google Scholar]
- 11.Yaksh TL. Multiple opioid receptor systems in brain and spinal cord: Part I. Eur J Anaesthesiol. 1984;1:171–99. [PubMed] [Google Scholar]
- 12.Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995;332:1685–90. doi: 10.1056/NEJM199506223322506. [DOI] [PubMed] [Google Scholar]
- 13.Sibinga NE, Goldstein A. Opioid peptides and opioid receptors in cells of the immune system. Annu Rev Immunol. 1988;6:219–49. doi: 10.1146/annurev.iy.06.040188.001251. [DOI] [PubMed] [Google Scholar]
- 14.Fields HL, Emson PC, Leigh BK, Gilbert RF, Iversen LL. Multiple opiate receptor sites on primary afferent fibres. Nature. 1980;284:351–3. doi: 10.1038/284351a0. [DOI] [PubMed] [Google Scholar]
- 15.Racz H, Gunning K, Della Santa D, Forster A. Evaluation of the effect of perineuronal morphine on the quality of postoperative analgesia after axillary plexus block: A randomized double-blind study. Anesth Analg. 1991;72:769–72. doi: 10.1213/00000539-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Karakaya D, Büyükgöz F, Baris S, Güldogus F, Tür A. Addition of fentanyl to bupivacaine prolongs anesthesia and analgesia in axillary brachial plexus block. Reg Anesth Pain Med. 2001;26:434–8. doi: 10.1053/rapm.2001.24675. [DOI] [PubMed] [Google Scholar]
- 17.Nishikawa K, Kanaya N, Nakayama M, Igarashi M, Tsunoda K, Namiki A. Fentanyl improves analgesia but prolongs the onset of axillary brachial plexus block by peripheral mechanism. Anesth Analg. 2000;91:384–7. doi: 10.1097/00000539-200008000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Fletcher D, Kuhlman G, Samii K. Addition of fentanyl to 1.5% lidocaine does not increase the success of axillary plexus block. Reg Anesth. 1994;19:183–8. [PubMed] [Google Scholar]


