Abstract
A variety of techniques and materials for the rehabilitation and reconstruction of traumatized maxillary ridges prior to dental implants placement have been described in literature. Autogenous bone grafting is considered ideal by many researchers and it still remains the most predictable and documented method. The aim of this report is to underline the effectiveness of using allogeneic bone graft for managing maxillofacial trauma. A case of a 30-year-old male with severely atrophic maxillary ridge as a consequence of complex craniofacial injury is presented here. Augmentation procedure in two stages was performed using allogeneic and autogenous bone grafts in different areas of the osseous defect. Four months after grafting, during the implants placement surgery, samples of both sectors were withdrawn and submitted to histological evaluation. On the examination of the specimens, treated by hematoxylin and eosin staining, the morphology of integrated allogeneic bone grafts was revealed to be similar to the autologous bone. Our clinical experience shows how the allogeneic bone graft presented normal bone tissue architecture and is highly vascularized, and it can be used for reconstruction of severe trauma of the maxilla.
Keywords: Maxillofacial injuries, Bone transplantation, Facial reconstruction
Introduction
Maxillofacial trauma can be related to several causes like ballistic or avulsion injuries to the face creating bone defects hard to be reconstructed.1, 2, 3, 4, 5 Maxillofacial traumatology is complex to be managed for the different involved anatomical features. To reduce morbidity and mortality, quick diagnosis and management of severe head trauma and concomitant injuries remains an important part of the initial assessment and treatment plan of severely facial traumatized patients.6, 7, 8, 9 At the emergency care unit, the first approach should evidence the cause and distribution of facial trauma and the concomitant possible injuries in order to help in the optimization of the initial clinical treatment and definition of the right time to involve oral surgeon.6, 8, 9, 10, 11 Rarely the fractures of the facial skeleton are associated with life-threatening hemorrhage; however in such condition, surgeons should arrest the hemorrhage before complete investigation. At this point, a careful evaluation of the other important systems is performed.8, 9, 10, 11, 12, 13
A variety of techniques and materials for the rehabilitation of traumatized maxillary ridges prior to dental implants placement have been described in literature.13, 14, 15 Despite many reconstructive methods available, autologous grafts are considered to be the “gold standard” because of their advantages of osteogenesis, osteoinduction, and osteoconduction.16
The osteogenic potential, no risk of antigenic reaction and cross-contamination are the major considerations in promoting it as the “gold standard” for augmentation procedures. However, there are limitations to the use of this type of bone grafts, such as restricted availability of the donor sites and additional morbidity caused by surgical harvesting procedure.17
Recent studies have shown that the use of allogeneic bone grafts represents a valid alternative and is suitable also for augmentation procedures of severely atrophic maxillary ridges. Allogeneic bone grafts obtained from individuals with different genetic loads, but from the same species, are biocompatible and exhibit good postoperative response.18 The aim of this study was to demonstrate that the allogeneic bone grafts provide good support for the placement of endosseous dental implants and can be considered an excellent alternative to the use of autogenous bone grafts for the atrophic maxillary ridge reconstruction.
Case report
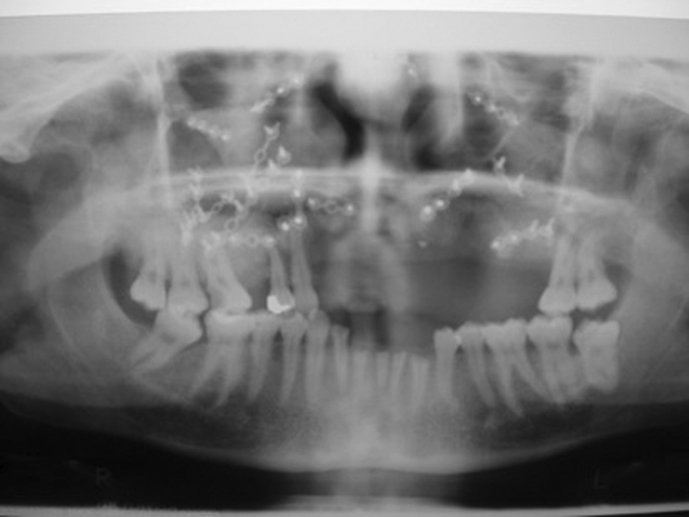
A case of a 30-year-old male with severely atrophic maxillary ridge as a consequence of complex craniofacial injury is presented here. On clinical and radiological examination the patient presented flat ridge with insufficient height and width, with total loss of the alveolar ridge. Based on this preoperative evaluation the case was classified as stage V of the Cawood and Howell classification of the edentulous jaws (Fig. 1, Fig. 2). Augmentation procedure in two stages was performed using allogeneic and autogenous bone grafts in different sectors of the osseous defect.
Fig. 1.
Three-dimensional evaluation of the residual bone of the jaws after the maxillofacial reconstruction and screw fixation. A large defect is still presented in the upper jaw frontal area.
Fig. 2.
Orthopanoramic view underlines the bone defect in the frontal area. Even the screw fixation solved the trauma a large bone reconstruction is needed.
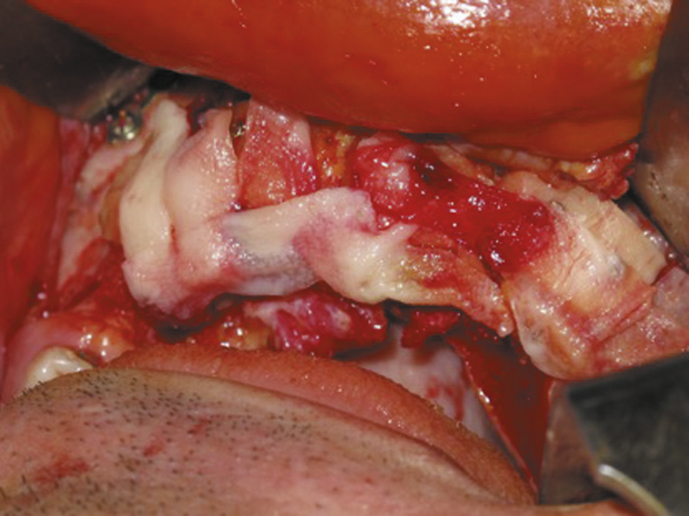
The reconstructive procedure was performed one year after the injury using autologous and graft of allogeneic bone for vertical and horizontal augmentation of the premaxilla. The choice of using both the type of graft was directed to avoid large homologous bone resection for the iliac crest. The possibility of choice of homologous bone is a condition that gives the surgeons the opportunity of using large amount of bone for bone defects reconstruction. The allogeneic bone was ordered from the Rizzoli Transplant Institute, Bologna. The used bones have been stored between −40 and −100 °C for up to 5 years. Bone is a commonly transplanted tissue, second only to blood. Bone tissue is donated both after death and from patients undergoing joint replacement surgery and other bone operations. The donor and bone are carefully screened for disease to ensure the bone is healthy (Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7).
Fig. 3.
Clinical view of the upper jaw atrophic ridge before the reconstruction.
Fig. 4.
A particular of the homologous bone graft from the iliac crest, applied like onlay graft to the maxillary atrophic ridge.
Fig. 5.
Clinical view of the onlay graft (mixed autologous and homologous) applied for the ridge reconstruction.
Fig. 6.
Soft tissue management by applying platelet rich fibrin for healing promotion.
Fig. 7.
Soft tissue management by using periosteal flap in order to cover all the regenerated area.
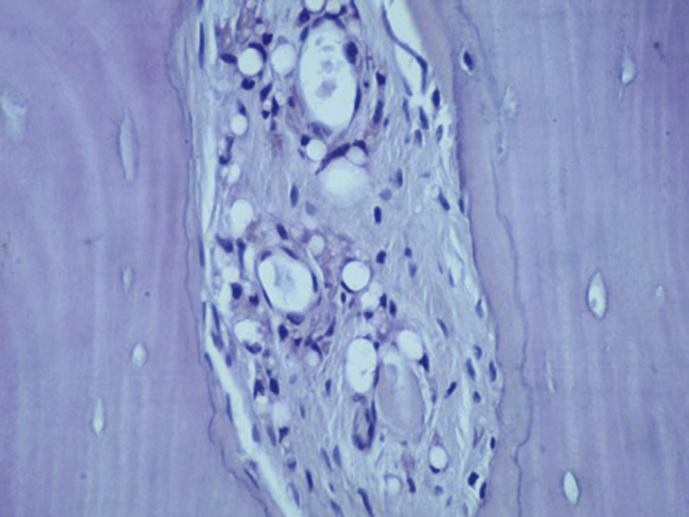
Four months after grafting, during the implants placement surgery, samples of both sectors were withdrawn and submitted to histological evaluation. On the examination of the specimens, treated by hematoxylin and eosin staining, the morphology of integrated allogeneic bone grafts was revealed to be similar to the autologous bone. Moreover, the allogeneic bone graft presented normal bone tissue architecture and the presence of several lacunae in entire bone tissue (Fig. 8, Fig. 9). For this reason next dental implants and prosthesis positioning have been successfully positioned.
Fig. 8.
The autogenous bone block shows marked staining differences from the host trabecular bone and in particular, it shows a lower affinity for the stains. The block is surrounded by newly formed bone (acid fuchsin-toluidine blue).
Fig. 9.
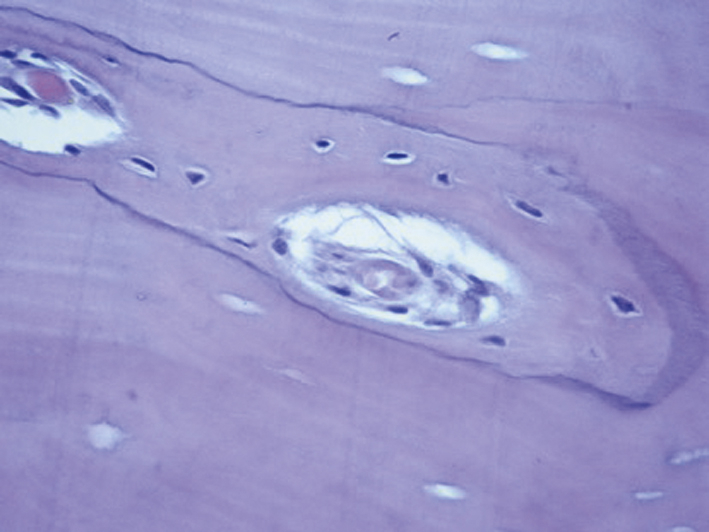
A good amount of newly formed bone can be observed even in the homologous bone (acid fuchsin-toluidine blue).
Discussion
Several studies have investigated the distribution and frequency of maxillofacial trauma.19, 20, 21, 22 Even if only few evaluations exist about the incidence of maxillofacial injuries in a general population of severely traumatized and injured patients the data of most of the underlying publications were collected twenty years ago and safety precautions have since significantly improved.23, 24, 25, 26 Some recent published studies recorded how the orbital (78%) and maxillary (70%) fractures were the most common facial bone fractures reported in politraumatized patient. It seems that the whole maxillary fractures in the form of LeFort fractures occurred in one fourth of the patients collected, in which LeFort III fractures are the most common type.27, 28, 29, 30
The management of large bone defects caused by trauma, degenerative or congenital diseases and tumor lesions is one of the greatest challenges in current orthopedic and maxillofacial research, making the development of effective bone regeneration therapies a major topic. Although the amount of available autogenous cancellous bone is naturally limited, and graft harvesting from the iliac crest leads to significant donor-site morbidity, autogenous bone grafts combining osteogenic, osteoconductive and osteoinductive properties is still considered the gold standard for bone substitutes. The osseous regeneration capacity is limited in older patients especially, and donor site morbidity increases. In addition to bone applications, current bone regeneration strategies include cell-based or stem cell-based treatments, the application of bioactive factors such as BMP-2 and BMP-7, different biologic or artificial scaffolds and various combinations. Several animal studies and clinical trials demonstrated how the BMP-2 application might reduce the possibility of harvested autologous bone for recreated the bone defects.16, 18, 31, 32
Allografts have been widely used in orthopaedic surgery for a long time for many clinical applications including tumours and trauma. Bone allografts provide a safe and efficient alternative to the autologous bone and at the same time avoid the second grafting surgical site avoiding pain and discomfort for the patient. The use of allogeneic biostatic tissue grafts is beneficial; however, it may involve some risk, e.g. due to possible transmission of infectious diseases and syndromes related.33
Different bone graft materials have been predictable used for guided bone regeneration and maxillary large bone defects reconstruction. The recent years have brought introduction of advanced medicinal products, which, apart from the scaffold, contain autologous osteogenic cells.31, 32, 33 These results underlined how the clinical and histological features of the allografts seems to be comparable with the autologous bone graft in maxillary atrophic ridge reconstruction.
To sum up, the gravity of all maxillofacial injuries lies in the fact that they pose an immediate threat to life as a consequence of its proximity to both the airway and brain. All the same, each case is unique; thus, the management is exacting even for the most experienced of professionals. In any given scenario no treatment approach can be described as being sure and flawless. This study with long term results clearly demonstrates that the allogeneic bone grafts provide good support for next placement of endosseous dental implants and can be considered an excellent alternative to the use of autogenous bone grafts in cases of facial trauma and important facial bone loss.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Telfer M.R., Jones G.M., Shepherd J.P. Trends in the aetiology of maxillofacial fractures in the United Kingdom (1977-1987) Br J Oral Maxillofac Surg. 1991;29:250–255. doi: 10.1016/0266-4356(91)90192-8. [DOI] [PubMed] [Google Scholar]
- 2.Chen S.C., Lin F.Y., Chang K.J. Body region prevalence of injury in alcohol- and non-alcohol-related traffic injuries. J Trauma. 1999;47:881–884. doi: 10.1097/00005373-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Fischer K., Zhang F., Angel M.F. Injuries associated with mandible fractures sustained in motor vehicle collisions. Plast Reconstr Surg. 2001;108:328–331. doi: 10.1097/00006534-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Cannell H., Paterson A., Loukota R. Maxillofacial injuries in multiply injured patients. Br J Oral Maxillofac Surg. 1996;34:303–308. doi: 10.1016/s0266-4356(96)90007-8. [DOI] [PubMed] [Google Scholar]
- 5.Follmar K.E., Debruijn M., Baccarani A. Concomitant injuries in patients with panfacial fractures. J Trauma. 2007;63:831–835. doi: 10.1097/TA.0b013e3181492f41. [DOI] [PubMed] [Google Scholar]
- 6.Gautam V., Leonard E.M. Bony injuries in association with minor head injury: lessons for improving the diagnosis of facial fractures. Injury. 1994;25:47–49. doi: 10.1016/0020-1383(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 7.Scheyerer M.J., Dutschler J., Billeter A. Effect of elevated serum alcohol level on the outcome of severely injured patients. Emerg Med J. 2014;31:813–817. doi: 10.1136/emermed-2013-202804. [DOI] [PubMed] [Google Scholar]
- 8.Hadjizacharia P., O'Keeffe T., Plurad D.S. Alcohol exposure and outcomes in trauma patients. Eur J Trauma Emerg Surg. 2011;37:169–175. doi: 10.1007/s00068-010-0038-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bataineh A.B. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/s1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 10.Lee K.H. Interpersonal violence and facial fractures. J Oral Maxillofac Surg. 2009;67:1878–1883. doi: 10.1016/j.joms.2009.04.117. [DOI] [PubMed] [Google Scholar]
- 11.Haug R.H., Prather J., Indresano A.T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 12.Hwang K., You S.H. Analysis of facial bone fractures: an 11-year study of 2094 patients. Indian J Plast Surg. 2010;43:42–48. doi: 10.4103/0970-0358.63959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maiorana C., Beretta M., Rancitelli D. Histological features and biocompatibility of bone and soft tissue substitutes in the atrophic alveolar ridge reconstruction. Case Rep Dent. 2016;2016:3608602. doi: 10.1155/2016/3608602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cicciù M. A window view from the orient on trauma involving the inner maxillofacial region: from China to the global community with love. J Craniofac Surg. 2016;27:6. doi: 10.1097/SCS.0000000000002280. [DOI] [PubMed] [Google Scholar]
- 15.Laino L., Iezzi G., Piattelli A. Vertical ridge augmentation of the atrophic posterior mandible with sandwich technique: bone block from the chin area versus corticocancellous bone block allograft–clinical and histological prospective randomized controlled study. Biomed Res Int. 2014;2014:982104. doi: 10.1155/2014/982104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cicciù M., Herford A.S., Cicciù D. Recombinant human bone morphogenetic protein-2 promote and stabilize hard and soft tissue healing for large mandibular new bone reconstruction defects. J Craniofac Surg. 2014;25:860–862. doi: 10.1097/SCS.0000000000000830. [DOI] [PubMed] [Google Scholar]
- 17.Petrauskaite O., Gomes Pde S., Fernandes M.H. Biomimetic mineralization on a macroporous cellulose-based matrix for bone regeneration. Biomed Res Int. 2013;2013:452750. doi: 10.1155/2013/452750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herford A.S., Tandon R., Stevens T.W. Immediate distraction osteogenesis: the sandwich technique in combination with rhBMP-2 for anterior maxillary and mandibular defects. J Craniofac Surg. 2013;24:1383–1387. doi: 10.1097/SCS.0b013e318292c2ce. [DOI] [PubMed] [Google Scholar]
- 19.Adeyemo W.L., Rabiu K.A., Okoturo T.M. Orofacial injuries associated with eclampsia in patients presenting at a Nigerian Tertiary hospital. J Obstet Gynaecol. 2012;32:54–57. doi: 10.3109/01443615.2011.613495. [DOI] [PubMed] [Google Scholar]
- 20.McDade A.M., McNicol R.D., Ward-Booth P. The aetiology of maxillo-facial injuries with special reference to the abuse of alcohol. Int J Oral Maxillofac Surg. 1982;11:152–155. doi: 10.1016/s0300-9785(82)80002-1. [DOI] [PubMed] [Google Scholar]
- 21.Olasoji H.O., Tahir A., Arotiba G.T. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40:140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 22.Dongas P., Hall G.M. Mandibular fracture patterns in Tasmania ten years of mandibular fractures: an analysis of 2137 cases. Aust Dent J. 2002;47:131–137. doi: 10.1111/j.1834-7819.2002.tb00316.x. [DOI] [PubMed] [Google Scholar]
- 23.Sojot A.J., Meisami T., Sandor G.K. A review of 246 cases. J Can Dent Assoc. 2001;67:640–644. [PubMed] [Google Scholar]
- 24.Luce E.A., Tubb T.D., Moore A.M. Review of 1,000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63:26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Ansari M.H. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987–2001) J Craniomaxillofac Surg. 2004;32:28–34. doi: 10.1016/j.jcms.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Bauer T.W., Muschler G.F. Bone graft materials. An overview of the basic science. Clin Orthop Relat Res. 2000;371:10–27. [PubMed] [Google Scholar]
- 27.Roberts T.T., Rosenbaum A.J. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8:114–124. doi: 10.4161/org.23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giannoudis P.V., Dinopoulos H., Tsiridis E. Bone substitutes: an update. Injury. 2005;36(Suppl 3):S20–S27. doi: 10.1016/j.injury.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 29.Li C.M., Ho Y.R., Liu Y.C. Transmission of human immunodeficiency virus through bone transplantation: a case report. J Formos Med Assoc. 2001;100:350–351. [PubMed] [Google Scholar]
- 30.Graham S.M., Leonidou A., Aslam-Pervez N. Biological therapy of bone defects: the immunology of bone allo-transplantation. Expert Opin Biol Ther. 2010;10:885–901. doi: 10.1517/14712598.2010.481669. [DOI] [PubMed] [Google Scholar]
- 31.Cicciù M., Herford A.S., Juodžbalys G. Recombinant human bone morphogenetic protein type 2 application for a possible treatment of bisphosphonates-related osteonecrosis of the jaw. J Craniofac Surg. 2012;23:784–788. doi: 10.1097/SCS.0b013e31824dbdd4. [DOI] [PubMed] [Google Scholar]
- 32.Cicciù M., Herford A.S., Stoffella E. Protein-signaled guided bone regeneration using titanium mesh and Rh-BMP2 in oral surgery: a case report involving left mandibular reconstruction after tumor resection. Open Dent J. 2012;6:51–55. doi: 10.2174/1874210601206010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cicciù M., Herford A.S., Bramanti E. Guillain-Barré syndrome: report of two rare clinical cases occurring after allergenic bone grafting in oral maxillofacial surgery. Int J Clin Expe Pathol. 2015;8:7614–7616. [PMC free article] [PubMed] [Google Scholar]