Abstract
After a thorough search through the database as PubMed database and Embase database, the clinical experimental articles have been selected out on the effects of early surgery on the treatment of active native infective endocarditis. The quality of the trials included in this study was assessed by researcher according to the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0. A meta-analysis was carried out in terms of clinical efficacy criteria by RevMan 5.3 software. Based on the results, we cautiously conclude that early surgery used for active native infective endocarditis could reduce in-hospital mortality, follow-up mortality, and IE-related mortality.
1. Introduction
The real incidence of infective endocarditis is hard to be obtained because of the population characteristics and other reasons. The incidence would be between 2 and 100 episodes/100,000 person-years [1, 2]. Infective endocarditis (IE) has poor prognosis, with the in-hospital mortality of 20% or even higher [3]. Since the use of penicillin, medical treatment has been performed in IE patients. Although medical treatment reduced the cases of death, the mortality of IE patients was still high. Because of the limitation in medical treatment, surgical therapy has been used for the treatment in some patients with IE. In 1960s, surgical therapy has been performed in IE patients. In the last 3 decades, more and more patients have received surgical treatment. In some western countries, surgery has been performed in around 50% of the patients with IE [4]. Surgery has been the major therapy for IE patients. The main indications for surgery in the treatment of IE were as follows: heart failure from structure destruction, persistent sepsis hardly to be controlled by formal medical therapy, large vegetation with embolism events, cardiac abscesses, ventricular arrhythmia, and so forth. A series of articles has been reported about comparison of outcomes between surgical therapy and medical treatment alone in recent years.
Better outcomes have been reported from surgical therapy in most of the articles. Conventionally, surgery should be performed after 4–6 weeks antibiotic treatment, except in some urgent cases, to reduce recurrence rate. This therapy was defined as “conventional therapy” in some articles. However, there were still many problems. During the long duration of medical treatment before surgery, embolic events, heart failure, formation of abscess cavity, and other complications were observed. And the mortality rate was still high. In consideration of all the problems above, optimal timing for surgery is the focus domain nowadays. In last 3 decades, the idea of “early surgery” has been set up. Although the definition of “early surgery” has not been unified, surgery performed in active phase has been used in some researches as the definition of “early surgery”. Early surgery has been recommended by some articles, with mortality of 6%–25%, and the long-term survival rate was about 70% [5, 6]. It could reduce mortality, embolic events, and improve heart function of patients with IE. And the recurrence rate in early surgery was not elevated. But in some other articles, the results were still debated, with no better prognosis [7]. In consideration of the low incidence of IE and ethics reasons, RCT research in IE patients was rare. Except for one RCT study, the conclusion has been derived mostly from retrospective studies. The conclusion may be influenced by following factors: hidden group, treatment bias, survivor bias, referral bias, and some other confounding factors. Some techniques have been used in reducing bias, such as propensity score analysis, Cox proportional hazards regression technique, and Biprobit technique. However, these methods were all statistical techniques and could not resolve all the drawbacks above. As a result, it was still controversial in whether early surgical therapy could result in better outcomes. And in 2015 ESC guidelines for the management of IE, although early surgery was recommended, the level of evidence was still level B [8].
For the above considerations, meta-analysis could make efforts in this domain. There has been some meta-analysis articles published years before, and no articles with high quality were published recently. In the concern of different mortality between native valve endocarditis (NVE) and prosthetic valve endocarditis (PVE), we focused on the effect of surgical and early surgical therapy for the patients with NVE. Meta-analysis has been used in our study to estimate the effect of early surgical therapy for the patients with NVE.
2. Methods
2.1. Search Strategy
PubMed and Embase databases were searched for English and Chinese language including the articles published during January 1990 to June 2015. The following Medical Subject Heading terms and/or keywords were used as “endocarditis”, “early surgery”, and “infective endocarditis surgery”. Studies comparing early surgery with conventional therapy in patients with IE were included. Two authors reviewed the trials, ensured that they met inclusion criteria, and abstracted the data.
2.2. Eligibility Criteria
2.2.1. Types of Studies
We included randomized controlled trials and retrospective study.
2.2.2. Participants
The patients diagnosed with active native infective endocarditis clearly.
2.2.3. Interventions
Early surgery was defined as follows: (1) surgery performed in active phase; (2) the duration between surgery and entrance to hospital was not more than 4 weeks; and (3) surgery performed during initial hospitalization.
2.2.4. Outcomes Measures
The outcomes assessed in this meta-analysis are the mortality rates of IE patients in different groups.
2.3. Data Extraction and Quality Assessment
The qualities of the data were assessed by two independent researchers. The third researcher would be invited for discussion whenever different opinions appeared. The quality of the trials included in this study was assessed by each researcher according to the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0.
2.4. Statistical Analysis
Risk ratio (RR) and 95% confidence intervals (CI) were used for counting data as effect size. Chi-square test would be applied to the heterogeneity. Fixed-effect model would be adopted when P > 0.1 or I2 < 50%. Random-effect model would be used when P < 0.1 or I2 > 50%. The statistics analysis was performed with Review Manager 5.3.
3. Results
3.1. Description of the Included Trails
3.1.1. Study Selection
A total of 107 reports were identified by our electronic database search and through other sources. After removing articles with different definitions (n = 4), without comparison between groups (n = 73), with the data from PVE patients that could not be excluded from NVE patients (n = 20). Finally, ten studies [9–18] met our inclusion criteria and were included in the present analysis (Figure 1).
Figure 1.
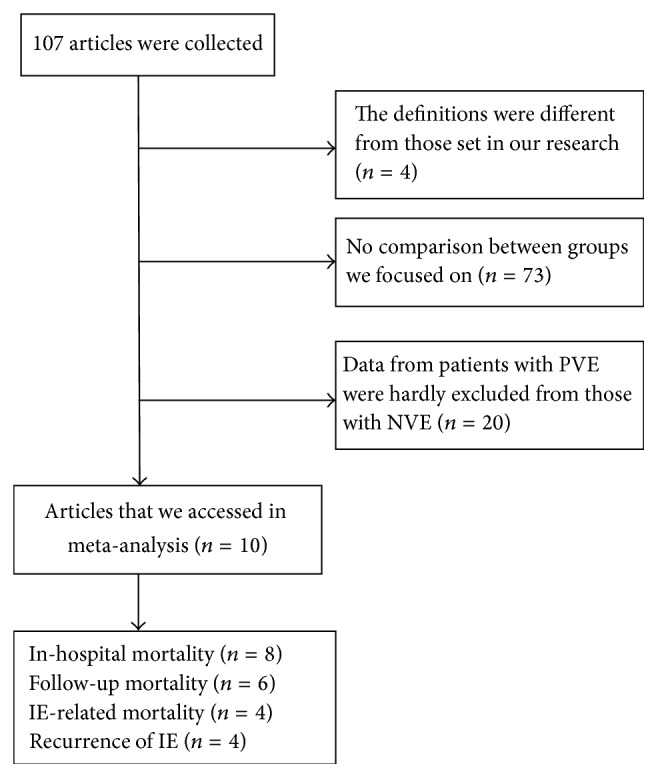
Flow chart of literature retrieval and trial selection.
3.1.2. Characteristics of Included Studies
They are shown in Table 1.
Table 1.
Characteristics of the 10 trials.
| Studies | Sample (T/C) | Diagnosis standard | Age (T/C) |
Intervention group | Control group | Follow-up (median, year) |
Outcome |
|---|---|---|---|---|---|---|---|
| Holenarasipur et al. 2003 | 109/109 | Modified Duke criteria | 53 ± 15/55 ± 19 | Early surgery | Conventional treatment | 0.5 | Follow-up mortality |
| Kim et al. 2010 | 64/68 | Modified Duke criteria | 45.9 ± 15.9/51.1 ± 17.4 | Early surgery | Conventional treatment | 3.8 | In-hospital mortality; follow-up mortality; IE-related mortality; recurrence of IE |
| Wang et al. 2014 | 70/169 | Modified Duke criteria | 41.6 ± 12.0/45.6 ± 17.2 | Early surgery | Conventional treatment | 2 | In-hospital mortality; follow-up mortality; IE-related mortality; recurrence of IE |
| Kang et al. 2012 | 37/39 | Modified Duke criteria | 45.5 ± 14.9/47.8 ± 17.5 | Early surgery | Conventional treatment | 0.5 | In-hospital mortality; follow-up mortality; IE-related mortality; recurrence of IE |
| Shunsuke et al. 2011 | 57/57 | Modified Duke criteria | 55 ± 18/53 ± 17 | Early surgery | Conventional treatment | 5.5 | In-hospital mortality; follow-up mortality; IE-related mortality; recurrence of IE |
| Tahaniyat et al. 2010 | 720/832 | Modified Duke criteria | 53/61 | Early surgery | Conventional treatment | Unclear | In-hospital mortality |
| Christopher et al. 2005 | 610/906 | Modified Duke criteria | 54.7 ± 15.2/61.1 ± 17.4 | Early surgery | Conventional treatment | Unclear | In-hospital mortality |
| Sendhil et al. 2005 | 29/32 | Modified Duke criteria | 22–80/23–80 | Received antibiotics for <2 weeks before surgery | Received antibiotics for 2–4 weeks before surgery | 3.1 | Follow-up mortality |
| Bruno et al. 2004 | 72/74 | Modified Duke criteria | Unclear | Early surgery | Conventional treatment | Unclear | In-hospital mortality |
| Yasuhiro et al. 1991 | 57/108 | O'Brien Pesanti | 15.9 (0,85) | Early surgery | Conventional treatment | Unclear | In-hospital mortality |
3.1.3. Quality of the Included Studies
It is shown in Table 2.
Table 2.
Quality of the included studies.
| Studies | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|
| Holenarasipur et al. 2003 | High risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Kim et al. 2010 | High risk | High risk | Unclear | Low risk | Low risk | Low risk |
| Wang et al. 2014 | High risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Kang et al. 2012 | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Shunsuke et al. 2011 | High risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Tahaniyat et al. 2010 | High risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Christopher et al. 2005 | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Sendhil et al. 2005 | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Bruno et al. 2004 | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Yasuhiro et al. 1991 | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
3.2. The Effect of Early Surgery
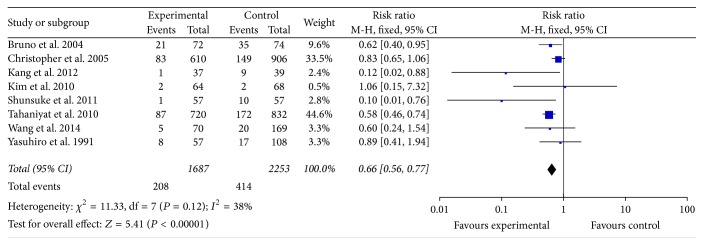
3.2.1. In-Hospital Mortality
The in-hospital mortality was reported in 8 studies that involved 3940 participants. All of these studies reported in-hospital mortality with early surgery compared with conventional medicine. Some of these studies reported evidence that early surgery reduced in-hospital mortality (RR = 0.66, 95% CI; 0.56, 0.77). There was no heterogeneity among the 8 studies (P = 0.12, I2 = 38%) (Figure 2).
Figure 2.
In-hospital mortality between two groups.
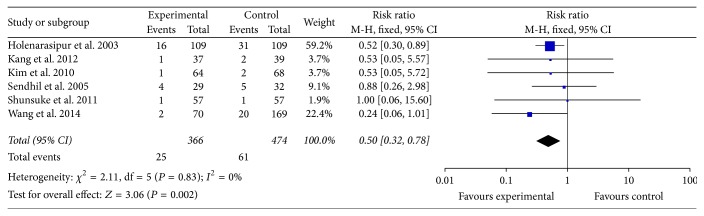
3.2.2. Follow-Up Mortality
The follow-up mortality was reported in 6 studies that involved 840 participants. All of these studies reported follow-up mortality with early surgery compared with conventional medicine. Some of these studies reported evidence that early surgery reduced follow-up mortality (RR = 0.50, 95% CI; 0.32, 0.78). There was no heterogeneity among the 6 studies (P = 0.83, I2 = 0%) (Figure 3).
Figure 3.
Follow-up mortality between two groups.
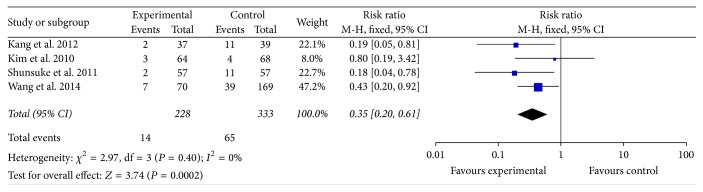
3.2.3. IE-Related Mortality
The IE-related mortality was reported in 4 studies that involved 561 participants. All of these studies reported IE-related mortality with early surgery compared with conventional medicine. Some of these studies reported evidence that early surgery reduced IE-related mortality (RR = 0.35, 95% CI; 0.20, 0.61). There was no heterogeneity among the 6 studies (P = 0.40, I2 = 0%) (Figure 4).
Figure 4.
IE-related mortality between two groups.
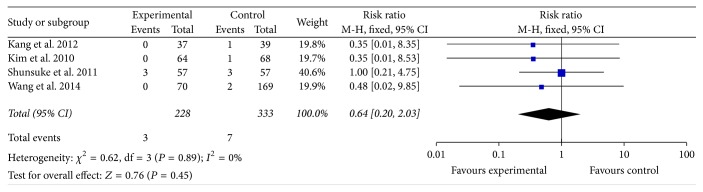
3.2.4. Recurrence of IE
The recurrence of IE was reported in 4 studies that involved 561 participants. All of these studies reported recurrence of IE with early surgery compared with conventional medicine. The result showed that early surgery was no better or worse at reducing recurrence of IE (RR = 0.64, 95% CI; 0.20, 2.03). There was no heterogeneity among the 4 studies (P = 0.89, I2 = 0%) (Figure 5).
Figure 5.
Recurrence of IE between two groups.
3.3. Funnel Plot of Publication Bias
Funnel plot analysis was conducted based on eight studies included, and this plot is summarized in Figure 6. The outcome suggests that there was little publication bias.
Figure 6.
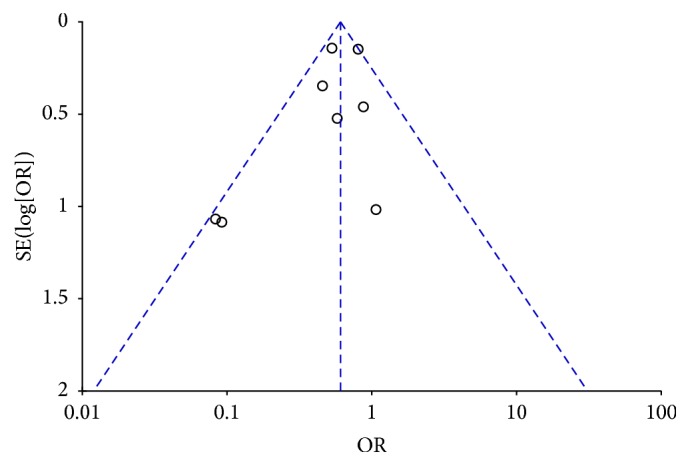
Funnel plot.
4. Discussion
4.1. Efficacy Analysis of Early Surgery
In Figure 2, the in-hospital mortality in early surgery group was as 66% as that in conventional group. In Figure 3, the follow-up mortality in early surgery group was only as half as that in conventional group. We could also find that the IE-related mortality in early surgery group was as 35% as that in conventional group from Figure 4. From all the mentioned above, patients in early surgery group had better outcome than those in conventional group. In propensity matched cohort study, the mortality of patients in early surgery group also seems to be lower.
These results are consistent with some other studies published before [19–21]. As mentioned in the articles, the baseline characteristics are different between the two groups. In early surgery group, more patients get severe cardiac damage, heart failure, and abscesses. And in conventional therapy group, patients get more coexisting diseases, like cerebral vascular disease, diabetes mellitus, and so forth. This is consistent with the report from Mourvillier et al.
Heart failure could be found in 42–60% of IE patients [22], and nearly 60% of IE patients received surgical treatment because of heart failure from structure destruction [23]. As reported before, patients with IE, with indication for surgical treatment, would get better cardiac function by early surgery [24]. In conventional therapy group, patients who should get surgical treatment usually get surgery after 4–6 weeks' medical treatment. During this period, structure destruction would develop, like aortic valve and mitral valve regurgitation. Destruction of cardiac structure would lead to deterioration of cardiac function. Patients with cardiac abscesses could also get benefit from early surgery. Furthermore, many cardiac abscesses and fistulae are found during surgery, without any presurgery evidence. And early surgery could get much benefit in these patients, in avoiding of the fatal condition. As a result, early surgery could get better cardiac function. Patients in early surgery group would get lower mortality rate for this reason.
Furthermore, embolic events, with the incidence of even up to 50%, are severe complications of IE, including cerebral embolism, kidney embolism, and spleen embolism. Embolic events are mostly found two weeks after discovery of cardiac vegetations [25, 26]. After the antibiotic duration of 4–6 weeks, the incidence of embolic events would get high, especially in the patients with silent embolism. Because of these conditions, early surgery could reduce the incidence of embolic events, which is consistent with Kang et al.'s report [12], and could lead to the lower mortality rate.
Nowadays, diagnostic methods and medical treatments in IE patients have developed much. No promotion of recurrence rate of IE had been observed in early surgery group in Figure 5. These results denoted that early surgery in NVE patients would be safe, and long-term antibiotic treatment would get no benefit.
4.2. Limitation
The included studies were mainly retrospective study; confounding factors may limit our interpretation. Considerable differences in baseline characteristics exist among the included studies, including regional variations and microbiological differences, and heterogeneity in clinical trials also existed. In our results, statistical heterogeneity was relatively small, with the I2 as follows: 38% in in-hospital mortality, 0% in follow-up mortality, 0% in IE-related mortality, and 0% in recurrence of IE. As in the situations mentioned above, there was heterogeneity in our research; however, most researches denoted early surgery therapy would get better outcome. As a result, early surgery would reduce mortality rate in IE patients. Among the articles that we have read, which focus on this controversial subject, our present study would be the first meta-analysis which makes comparison of the outcomes between early surgery therapy and conventional therapy in the patients with native valve infective endocarditis. Our research suggests the superiority of early surgery therapy. This finding should be used as hypothesis generating and as basis for further well designed randomized trials.
4.3. Prospects for Early Surgery
As mentioned above, early surgery could get better cardiac function, lower embolic events, and lower mortality. Recurrence of IE is catastrophic. Nowadays, antimicrobial therapy has developed greatly, and the methods of investigation of pathogens have been much developed. PCR technique has also been used to find pathogens [27]. Early surgery will not elevate the incidence of reinfection, which has been proved by some researches [12]. As a result, long-term duration is not necessary in respect of reinfection.
According to our results, early surgery in NVE patients will not elevate the incidence of reinfection and reduce mortality rate. This finding is consistent with the recommendations in 2015 ESC IE guidelines and should be used as basis for further well designed researches.
5. Conclusion
The current limited evidence showed that when compared with conventional medicine, early surgery could reduce in-hospital mortality, follow-up mortality, and IE-related mortality.
Acknowledgments
This research was funded by National Natural Science Foundation of China (81600208).
Disclosure
The funders had no role in study design and data collection and analysis, decision to publish, or preparation of the paper.
Competing Interests
The authors declare that there is no conflict of interests regarding the publication of this article.
References
- 1.Thuny F., Grisoli D., Collart F., Habib G., Raoult D. Management of infective endocarditis: challenges and perspectives. The Lancet. 2012;379(9819):965–975. doi: 10.1016/s0140-6736(11)60755-1. [DOI] [PubMed] [Google Scholar]
- 2.Bashore T. M., Cabell C., Fowler V., Jr., et al. Update on infective endocarditis. Current Problems in Cardiology. 2006;31(4):274–352. doi: 10.1016/j.cpcardiol.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Winston L. G., Bolger A. F. Modern epidemiology, prophylaxis, and diagnosis and therapy for infective endocarditis. Current Cardiology Reports. 2006;8(2):102–108. doi: 10.1007/s11886-006-0020-3. [DOI] [PubMed] [Google Scholar]
- 4.Tornos P., Iung B., Permanyer-Miralda G., et al. Infective endocarditis in Europe: lessons from the Euro heart survey. Heart. 2005;91(5):571–575. doi: 10.1136/hrt.2003.032128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexiou C., Langley S. M., Stafford H., Lowes J. A., Livesey S. A., Monro J. L. Surgery for active culture-positive endocarditis: determinants of early and late outcome. Annals of Thoracic Surgery. 2000;69(5):1448–1454. doi: 10.1016/s0003-4975(00)01139-5. [DOI] [PubMed] [Google Scholar]
- 6.Hasbun R., Vikram H. R., Barakat L. A., Buenconsejo J., Quagliarello V. J. Complicated left-sided native valve endocarditis in adults: risk classification for mortality. The Journal of the American Medical Association. 2003;289(15):1933–1940. doi: 10.1001/jama.289.15.1933. [DOI] [PubMed] [Google Scholar]
- 7.Tleyjeh I. M., Ghomrawi H. M. K., Steckelberg J. M., et al. The impact of valve surgery on 6-month mortality in left-sided infective endocarditis. Circulation. 2007;115(13):1721–1728. doi: 10.1161/CIRCULATIONAHA.106.658831. [DOI] [PubMed] [Google Scholar]
- 8.Habib G., Lancellotti P., Iung B. 2015 ESC guidelines on the management of infective endocarditis: a big step forward for an old disease. Heart. 2016;102(13):992–994. doi: 10.1136/heartjnl-2015-308791. [DOI] [PubMed] [Google Scholar]
- 9.Kim D. H., Kang D.-H., Lee M.-Z., et al. Impact of early surgery on embolic events in patients with infective endocarditis. Circulation. 2010;122:S17–S22. doi: 10.1161/CIRCULATIONAHA.109.927665. [DOI] [PubMed] [Google Scholar]
- 10.Cabell C. H., Abrutyn E., Fowler V. G., Jr., et al. Use of surgery in patients with native valve infective endocarditis: results from the International Collaboration on Endocarditis Merged Database. American Heart Journal. 2005;150(5):1092–1098. doi: 10.1016/j.ahj.2005.03.057. [DOI] [PubMed] [Google Scholar]
- 11.Funakoshi S., Kaji S., Yamamuro A., et al. Impact of early surgery in the active phase on long-term outcomes in left-sided native valve infective endocarditis. The Journal of Thoracic and Cardiovascular Surgery. 2011;142(4):836.e1–842.e1. doi: 10.1016/j.jtcvs.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 12.Kang D.-H., Kim Y.-J., Kim S.-H., et al. Early surgery versus conventional treatment for infective endocarditis. New England Journal of Medicine. 2012;366(26):2466–2473. doi: 10.1056/NEJMoa1112843. [DOI] [PubMed] [Google Scholar]
- 13.Lalani T., Cabell C. H., Benjamin D. K., et al. Analysis of the impact of early surgery on in-hospital mortality of native valve endocarditis: use of propensity score and instrumental variable methods to adjust for treatment-selection bias. Circulation. 2010;121(8):1005–1013. doi: 10.1161/circulationaha.109.864488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mourvillier B., Trouillet J.-L., Timsit J.-F., et al. Infective endocarditis in the intensive care unit: clinical spectrum and prognostic factors in 228 consecutive patients. Intensive Care Medicine. 2004;30(11):2046–2052. doi: 10.1007/s00134-004-2436-9. [DOI] [PubMed] [Google Scholar]
- 15.Wang H., Zhang S., Tian Z., Guo L. The impact of early surgery on long-term outcome of patients with left-sided infective endocarditis. Zhonghua Nei Ke Za Zhi. 2014;53(6):450–454. [PubMed] [Google Scholar]
- 16.Balasubramanian S. K., Behranwala A., Devbhandari M., et al. Predictors of mortality in early surgical intervention for active native valve endocarditis and significance of antimicrobial therapy: a single-center experience. Journal of Heart Valve Disease. 2005;14(1):15–22. [PubMed] [Google Scholar]
- 17.Vikram H. R., Buenconsejo J., Hasbun R., Quagliarello V. J. Impact of valve surgery on 6-month mortality in adults with complicated, left-sided native valve endocarditis: a propensity analysis. The Journal of the American Medical Association. 2003;290(24):3207–3214. doi: 10.1001/jama.290.24.3207. [DOI] [PubMed] [Google Scholar]
- 18.Soma Y., Handa S., Iwanaga S. Medical treatment or surgical intervention? A cooperative retrospective study on infective endocarditis—timing of operation. Japanese Circulation Journal. 1991;55(8):799–803. doi: 10.1253/jcj.55.799. [DOI] [PubMed] [Google Scholar]
- 19.Aksoy O., Sexton D. J., Wang A., et al. Early surgery in patients with infective endocarditis: a propensity score analysis. Clinical Infectious Diseases. 2007;44(3):364–372. doi: 10.1086/510583. [DOI] [PubMed] [Google Scholar]
- 20.Sy R. W., Bannon P. G., Bayfield M. S., Brown C., Kritharides L. Survivor treatment selection bias and outcomes research a case study of surgery in infective endocarditis. Circulation: Cardiovascular Quality and Outcomes. 2009;2(5):469–474. doi: 10.1161/CIRCOUTCOMES.109.857938. [DOI] [PubMed] [Google Scholar]
- 21.Hill E. E., Herregods M.-C., Vanderschueren S., Claus P., Peetermans W. E., Herijgers P. Outcome of patients requiring valve surgery during active infective endocarditis. Annals of Thoracic Surgery. 2008;85(5):1564–1569. doi: 10.1016/j.athoracsur.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Nadji G., Rusinaru D., Rémadi J.-P., Jeu A., Sorel C., Tribouilloy C. Heart failure in left-sided native valve infective endocarditis: characteristics, prognosis, and results of surgical treatment. European Journal of Heart Failure. 2009;11(7):668–675. doi: 10.1093/eurjhf/hfp077. [DOI] [PubMed] [Google Scholar]
- 23.Revilla A., López J., Vilacosta I., et al. Clinical and prognostic profile of patients with infective endocarditis who need urgent surgery. European Heart Journal. 2007;28(1):65–71. doi: 10.1093/eurheartj/ehl315. [DOI] [PubMed] [Google Scholar]
- 24.Funakoshi S., Kaji S., Yamamuro A., et al. Impact of early surgery in the active phase on long-term outcomes in left-sided native valve infective endocarditis. Journal of Thoracic and Cardiovascular Surgery. 2011;142(4):836.e1–842.e1. doi: 10.1016/j.jtcvs.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 25.Thuny F., Disalvo G., Belliard O., et al. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation. 2005;112(1):69–75. doi: 10.1161/circulationaha.104.493155. [DOI] [PubMed] [Google Scholar]
- 26.Vilacosta I., Graupner C., SanRomán J., et al. Risk of embolization after institution of antibiotic therapy for infective endocarditis. Journal of the American College of Cardiology. 2002;39(9):1489–1495. doi: 10.1016/s0735-1097(02)01790-4. [DOI] [PubMed] [Google Scholar]
- 27.Raoult D., Casalta J. P., Richet H., et al. Contribution of systematic serological testing in diagnosis of infective endocarditis. Journal of Clinical Microbiology. 2005;43(10):5238–5242. doi: 10.1128/JCM.43.10.5238-5242.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]