Figure 3. of Ocular Surface Immune Response.
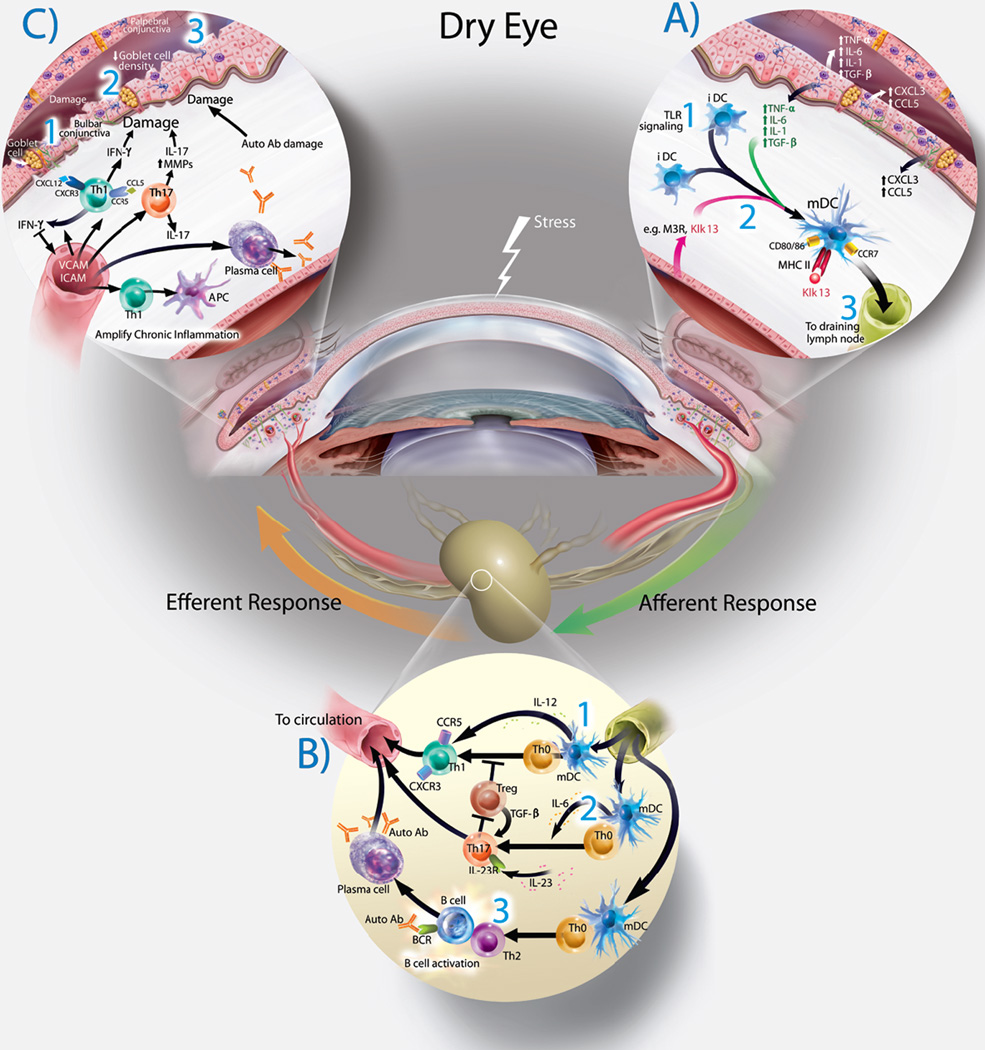
A— Exposure of the ocular surface to desiccating stress or pathogen associated molecular products (PAMPS) initiates an initial non-specific innate immune response with secretion of multiple cytokines and chemokines. Initiation of Adaptive Immune Response— The Afferent Arm of the Immune Response (right side): 1— Initial Toll-Like Receptor (TLR) signaling and antigen exposure on the ocular surface results in antigen uptake and processing by immature dendritic cells (iDS’s). 2— As the dendritic cells mature (mDC’s), antigens are processed and presented to the cell surface. These cell utilize the chemokine receptor CCR7 to leave the ocular surface and travel to the regional draining lymph nodes via ocular surface lymphatics.
B— Lymph Node (Bottom). The dendritic cells arrive in the lymph node and encounters a population of naive T-cells (Th0). The fate of these naive T cells is determined by the antigens, local environment and the specific cytokines secreted. 1— Th-1 cells are generated by DC secretion of IL-12. 2— Th-17 cells are generated by DC secretion of IL-6 and IL-23. 3— Th2 cells are generated by secretion of TSLP. Th-2 cells interact and activate B-cells which can mature (exposure to auto-antibodies) which mature the B-cells into antibody secreting Plasma Cells. All of these primed and targeted T cells will “home” via the systemic circulation to the LFU as part of the Efferent Arm of the Immune Response (left side).
C— Once these cells arrive at the ocular surface, they encounter adhesion molecules, leave the vessels and are activated by the constant presence of specific antigen. These cells then secrete a multitude of cytokines (IFN-γ, IL-17, etc. and MMPs). This creates the chronic immune response found in dry eye.
