Abstract
Hypoxia induces proliferation and invasion in cancer cells via hypoxia-inducible factor (HIF)-1α. The cell adhesion molecule cluster of differentiation (CD) 44 has been associated with increased cell invasion and metastasis. Whether hypoxia regulates the expression of CD44 in gastric cancer cells remains to be established. In the current study, the effects of hypoxia on HIF-1α and CD44 expression levels in human gastric cell lines SGC-7901 and BGC-823 were evaluated. The cells were cultured in 1% O2 for 1 week and then treated with 20 nM rapamycin for 72 h. Cell viability was evaluated using the Cell Counting kit-8 assay, and cell invasion was detected by the Transwell invasion assay. The protein and messenger (m) RNA expression levels of HIF-1α and CD44 were detected using western blotting and reverse transcription-quantitative polymerase chain reaction, respectively. The results revealed that cell viability and invasion increased under hypoxic conditions, but decreased following rapamycin treatment in SGC-7901 and BGC-823 cells. Hypoxia also increased the protein and mRNA expression levels of HIF-1α and CD44 in these two cell lines. However, this hypoxia-induced increase in HIF-1α and CD44 protein and mRNA expression levels was inhibited by rapamycin. These findings suggest that hypoxia induced the proliferation and invasion of SGC-7901 and BGC-823 cells. Furthermore, CD44 expression levels were potentially associated with HIF-1α expression levels. Therefore, in gastric cancer cells, hypoxia may regulate CD44 expression via HIF-1α in order to promote cell proliferation and invasion.
Keywords: gastric cancer cell, hypoxia, cluster of differentiation 44, hypoxia-inducible factor-1α
Introduction
Cluster of differentiation (CD) 44 transmembrane glycoproteins are cell-adhesion molecules that are associated with cancer cell aggressiveness and metastasis (1,2). In numerous types of cancer, including gastric cancer, CD44 has been associated with increased invasion, metastasis and poor prognosis (3,4). This molecule has also been identified as a marker of stem-like gastric cancer cells (5,6); however, its role in this phenotype remains to be defined.
Previous studies have suggested that hypoxia provides a suitable niche for stem cells to maintain their precursor status (7,8). Hypoxic tumor microenvironments induce phenotypic changes that make cancer cells aggressive (9,10), refractory to treatment (11) and likely to metastasize (12). These phenotypic changes are mediated by hypoxia-inducible factors (HIFs) (12). HIF is a heterodimer consisting of an oxygen-dependent α subunit and a constitutively expressed β subunit (9). Previous studies have demonstrated that HIF-1α is overexpressed in gastric cancer (13–15); furthermore, HIF-1α is associated with metastatic potential in gastric cancer cells via undefined underlying mechanisms (10).
HIF-1α is a regulator of CD44 in breast cancer cells under hypoxic conditions; HIF-1α increases CD44 expression levels and the number of CD44-positive cells (16). In gastric cancer cells, a significant correlation between HIF-1α expression levels and the immunohistochemical staining pattern of CD133 has been observed (17). However, whether HIF-1α regulates CD44 expression levels in gastric cancer cells remains to be established. The present study examined the effects of hypoxia on HIF-1α and CD44 expression levels in the moderately differentiated gastric cancer cell line SGC-7901 and in the poorly differentiated gastric cancer cell line BGC-823. In addition, the effects of HIF-1α downregulation on CD44 expression levels were evaluated in these gastric cancer cell lines.
Materials and methods
Cell culture and hypoxia treatment
The human gastric cancer cell lines SGC-7901 and BGC-823 were obtained from the China Center for Type Culture Collection (Wuhan, China). All cell lines were maintained in RPMI 1640 medium (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal calf serum (Gibco; Thermo Fisher Scientific, Inc.) under normoxic or hypoxic conditions for 7 days. Subsequently, the cells were treated with 20 nM rapamycin (Sigma-Aldrich; Merck Millipore, Darmstadt, Germany) for 72 h at 37°C in a humidified atmosphere of 5% CO2 and 95% air. Rapamycin was used to downregulate the expression levels of HIF-1α (18). For hypoxic exposure, tumor cells were incubated in an hypoxic incubator (BINDER GmbH, Tuttlingen, Germany) containing 1% O2, which was balanced by CO2 and nitrogen.
Cell proliferation assay
The Cell Counting kit-8 (CCK-8; Dojindo Molecular Technologies, Inc., Kumamoto, Japan) assay was used to evaluate cell viability, according to the manufacturer's protocol. Cells were seeded onto 96-well plates at a density of 5×103 cells/well and incubated for 24 h, and subsequently incubated in culture medium containing 20 nM rapamycin at 37°C in a humidified atmosphere of 5% CO2 and 95% air. CCK-8 solution (10 µl) was added to each well at 24, 48 and 72 h. The color intensity was evaluated using a microplate reader (Beijing Liuyi Biotechnology Co., Ltd., Beijing, China) at an absorbance wavelength of 450 nm. All experiments were performed in triplicate and repeated independently three times.
Cell migration and invasion assays
These assays were performed according to a previously described protocol (19). Briefly, Transwell units with 8.0-µm-pore polycarbonate filters (Corning Incorporated, Corning, NY, USA) were precoated with 50 µl of 1:5 diluted Matrigel (BD Biosciences, Franklin Lakes, NJ, USA). A total volume of 200 µl of gastric cancer cell suspension, which contained ~1×105 rapamycin-treated cells, was added to the upper compartment of the precoated units. The units were then transferred to the wells of the culture plate and incubated for 24 h at 37°C. Subsequently, the cells and Matrigel on the upper surface of the membrane were removed. Cells that had migrated to the underside were stained with 0.1% crystal violet for 15 min at room temperature, and cell numbers were determined using light microscopy. Five randomly selected fields were counted per insert.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
The gastric cancer cell lines were maintained with medium containing 20 nM rapamycin under normoxic or hypoxic conditions for 72 h. Total RNA was then isolated using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.), according to the manufacturer's protocol. The corresponding complementary DNA (cDNA) was synthesized using the PrimeScript™ RT Reagent kit (Takara Biotechnology Co., Ltd., Dalian, China). RT-qPCR was performed using SYBR® premix Ex Taq™ (Takara Biotechnology Co., Ltd.) and gene-specific primers in the Rotor-Gene 3000 system (Qiagen, Inc., Valencia, CA, USA). The PCR reaction mixtures contained 12.5 µl Premix Ex Taq™, 0.2 µM PCR primers, 0.4 µM SYBR Green I and 0.08 µM cDNA. All primers were designed using Primer Premier 5.0 (Premier Biosoft International, Palo Alto, CA, USA), and their sequences and annealing temperatures are presented in Table I. GAPDH was used as the housekeeping gene for normalization of the mRNA expression levels. Fold changes in the expression levels for each mRNA were calculated using the 2−∆∆Cq method (20).
Table I.
Oligonucleotide primer sequences and reverse transcription-quantitative polymerase chain reaction thermocycling conditions.
| Cycling conditions | ||
|---|---|---|
| Target gene primer sequence, 5′-3′ | Number of cycles | Annealing temperature, °C (time) |
| Cluster of differentiation 44 | ||
| F: CAAGCAATAGGAATGATGTC | 45 | 60 (15 sec) |
| R: GGTCACTGGGATGAAGGT | ||
| Hypoxia-inducible factor-1α | ||
| F: GGGAGAAAATCAAGTCGTGC | 45 | 60 (20 sec) |
| R: AGCAAGGAGGGCCTCTGATG | ||
| GAPDH | ||
| F: GCACCGTCAAGGCTGAGAAC | 45 | 60 (15 sec) |
| R: TGGTGAAGACGCCAGTGGA | ||
F, forward; R, reverse.
Western blot analysis
Using the TRIzol® reagent, total protein was extracted from the cells. The protein concentration was evaluated using a Protein Assay kit (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The proteins (50 mg/well) were separated by 12% SDS-PAGE and then electrophoretically transferred onto nitrocellulose membranes. The membranes were blocked with 5% bovine serum albumin (Gibco; Thermo Fisher Scientific, Inc.) at room temperature and then probed overnight at 4°C using polyclonal antibodies against CD44 (ab51037; Abcam, Cambridge, UK) and HIF-1α (sc-10790; Santa Cruz Biotechnology, Inc., Dallas, TX, USA) at a final dilution of 1:200 (w/v). The anti-GAPDH antibody (sc-25778, Santa Cruz Biotechnology, Inc.) was used overnight at 4°C at a final dilution of 1:600 (w/v). The membranes were then washed in PBS with Tween-20 and incubated with peroxidase-conjugated anti-rabbit immunoglobulin G [dilution, 1:3,000 (w/v); BA1054; Wuhan Boster Biological Technology, Ltd., Wuhan, China) (21) for 30 min at room temperature. The bands were visualized using an enhanced chemiluminescence kit (P0018; Beyotime Institute of Biotechnology, Haimen, China), and their optical densities were evaluated using a photo documentation and imaging system (BIO-ID VL, Conn, France).
Statistical analysis
All data were expressed as the mean ± standard deviation. Using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA), one-way analysis of variance and the Student's t-test were employed to analyze the data. P<0.05 was considered to indicate a statistically significant difference.
Results
The viability of the gastric cancer cell lines is promoted by hypoxia and inhibited by rapamycin
Compared with the normoxia control group (Fig. 1), hypoxia significantly increased the viability of SGC-7901 and BGC-823 cells after 72 h of incubation (P=0.001 and P=0.009, respectively). Hypoxia-induced increases in cell viability were inhibited by rapamycin treatment (P=0.001 and P=0.01, respectively).
Figure 1.
Effect of rapamycin on (A) SGC-7901 and (B) BGC-823 cell proliferation under hypoxic conditions. Results are presented as the mean ± standard deviation. All experiments were performed in triplicate and repeated independently three times. *P<0.05, hypoxia control group vs. normoxia control group; #P<0.05, hypoxia control group vs. hypoxia plus rapamycin group. OD450; optical density at 450 nm.
Cell migration and invasion in gastric cancer cell lines is induced by hypoxia and inhibited by rapamycin
To examine the effects of hypoxia and rapamycin pretreatment on the biological behavior of the cells, migration and invasion assays were performed. As presented in Fig. 2, significantly higher numbers of invasive cells were observed following hypoxia treatment. Hypoxia induced 1.3- and 1.9-fold increases in the number of invasive SGC-7901 and BGC-823 cells, respectively (P=0.001 and P=0.005, respectively). However, rapamycin pretreatment significantly decreased these invasive cell numbers by 29 and 24%, respectively (P=0.001 and P=0.008, respectively).
Figure 2.
Effect of rapamycin on (A) SGC-7901 (B) and BGC-823 cell migration and invasion under hypoxic conditions. Results are presented as the mean + standard deviation. All experiments were performed in triplicate and repeated independently three times. *P<0.05, hypoxia control group vs. normoxia control group; #P<0.05, hypoxia control group vs. hypoxia plus rapamycin group.
HIF-1α mRNA expression is induced by hypoxia and inhibited by rapamycin in gastric cancer cell lines
Hypoxia increased the mRNA expression levels of HIF-1α in SGC-7901 and BGC-823 cells (P=0.001 and P=0.001, respectively; Fig. 3). To downregulate the mRNA expression of HIF-1α, the two gastric cancer cell lines were treated with rapamycin. Under hypoxic conditions, treatment with rapamycin significantly reduced the mRNA expression levels of HIF-1α by 40 and 30% in SGC-7901 and BGC-823 cells, respectively (P=0.001 and P=0.001, respectively).
Figure 3.
Effect of hypoxia and rapamycin on the mRNA expression levels of HIF-1α in (A) SGC-7901 and (B) BGC-823 cells. Results are presented as the mean + standard deviation and were normalized to GAPDH. All experiments were performed in triplicate and repeated independently three times. **P<0.01, hypoxia control group vs. normoxia control group; ##P<0.01, hypoxia control group vs. hypoxia plus rapamycin group. HIF-1α, hypoxia-inducible factor-1α; mRNA, messenger RNA.
CD44 mRNA expression levels are increased by hypoxia and decreased by rapamycin in gastric cancer cell lines
Whether hypoxia is able to modulate the expression levels of CD44 mRNA was subsequently examined. Hypoxia induced 3.0- and 2.2-fold increases in CD44 mRNA expression levels in SGC-7901 and BGC-823 cells, respectively (P=0.01 and P=0.001, respectively; Fig. 4). Treatment with rapamycin under hypoxic conditions decreased CD44 mRNA expression levels by 45 and 52% in SGC-7901 and BGC-823 cells, respectively (P=0.007 and P=0.03, respectively; Fig. 4).
Figure 4.
Effects of hypoxia and rapamycin on the mRNA expression levels of CD44 in (A) SGC-7901 and (B) BGC-823 cells. Results are presented as the mean + standard deviation and were normalized to GAPDH. All experiments were performed in triplicate and repeated independently three times. **P<0.01, hypoxia control group vs. normoxia control group; ##P<0.01, hypoxia control group vs. hypoxia plus rapamycin group. CD44, cluster of differentiation 44; mRNA, messenger RNA.
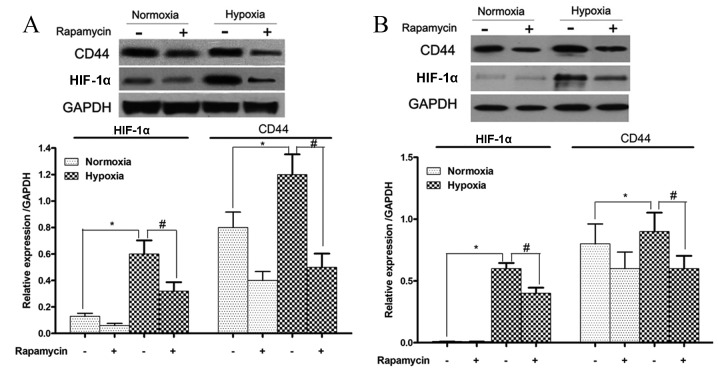
HIF-1α and CD44 protein expression levels are increased during hypoxia and reduced by rapamycin in gastric cancer cell lines
The protein expression levels of HIF-1α and CD44 in SGC-7901 and BGC-823 cells that were treated with or without rapamycin under hypoxic conditions were also examined. HIF-1α and CD44 protein expression levels were significantly induced by hypoxia in these two cell lines (SGC-7901 cells, P=0.001 and P=0.03, respectively; and BGC-823 cells, P=0.029 and P=0.032, respectively; Fig. 5). However, these increases in HIF-1α and CD44 protein expression levels were significantly reduced upon rapamycin treatment (SGC-7901 cells, P=0.009 and P=0.01, respectively; and BGC-823 cells, P=0.02 and P=0.037, respectively; Fig. 5).
Figure 5.
Effect of hypoxia and rapamycin on the protein expression levels of HIF-1α and CD44 in (A) SGC-7901 and (B) BGC-823 cells. Representative western blot and densitometry analyses are presented. HIF-1α and CD44 expression levels were normalized to GAPDH. Results are presented as the mean + standard deviation. All experiments were performed in triplicate and repeated independently three times. *P<0.05, hypoxia control group vs. normoxia control group; #P<0.05, hypoxia control group vs. hypoxia plus rapamycin group. CD44, cluster of differentiation 44; HIF-1α, hypoxia inducible factor-1α.
Discussion
Gastric cancer is a major global malignancy and the second leading cause of cancer mortality, with estimated 951,600 new stomach cancer cases and 723,100 mortalities occurring worldwide in 2012 (22). There is currently no effective treatment for highly advanced gastric cancer or recurrent gastric cancer, and the survival rates are low (23). Treatments are frequently ineffective due to high levels of heterogeneity between cases (24,25). The cancer stem cell (CSC) hypothesis may provide novel approaches for eradicating the cause of cell heterogeneity, which is associated with therapeutic resistance, relapse and distant metastasis (26,27). Therefore, the establishment of a treatment that targets CSCs to radically cure cancer is an important goal, and the identification of gastric CSCs may aid the development of gastric cancer therapies in the future.
CD44 is a transmembrane glycoprotein and a cell-adhesion molecule. It has been reported to serve important roles in extracellular matrix adhesion, motility, matrix degradation, proliferation and cell survival (28–30). These functions are involved in cancer pathology, including tumor progression and metastasis. In severe combined immunodeficient mice, CD44-positive gastric cancer cells have been demonstrated to exhibit high tumorigenic ability and the stem cell properties of self-renewal and differentiation (6). This suggests that CD44 may be a potential biomarker of gastric CSCs.
In the current study, hypoxia was able to promote the proliferation, migration and invasion of gastric cancer cells. This result was consistent with a previous study demonstrating that the hypoxic microenvironment upgrades the stem-like properties of gastric cancer cells by promoting invasion and metastasis (31). HIF-1α has been revealed to regulate specific surface markers, including CD133 and CD24, in several cancer cell types (32–34). However, an association between HIF-1α and CD44 in gastric cancer cells has not yet been reported. The current study hypothesized that HIF-1α also regulated the expression levels of CD44 in gastric cancer cells. The results demonstrated that hypoxia increased the mRNA and protein expression levels of HIF-1α in two gastric cancer cell lines. Furthermore, the mRNA and protein expression levels of CD44 were also increased. As a downstream molecule in the mammalian target of rapamycin (mTOR) signaling pathway, the mRNA and protein expression levels of HIF-1α were reduced upon treatment with rapamycin, which is an inhibitor of mTOR, under hypoxic conditions (33). In addition, the downregulation of HIF-1α expression decreased CD44 expression levels and significantly inhibited the proliferation and invasive ability of gastric cancer cells. This suggests that hypoxia may regulate the expression levels of CD44 via HIF-1α and influence the proliferation and invasion activity of gastric cancer cells.
The molecular mechanism underlying the HIF-1α-mediated regulation of CD44 expression levels remains to be elucidated. Certain studies have suggested that HIF-1α activation regulates the Wnt/β-catenin signaling pathway, which activates the expression of target genes and contributes to the enhanced invasion of hypoxic gastric cancer cells (35–37). CD44 is a target gene of the Wnt/β-catenin signaling pathway (38); therefore, the mechanism by which HIF-1α regulates CD44 may be associated with the Wnt/β-catenin signaling pathway in gastric cancer. Further studies are required to investigate these underlying mechanisms in gastric cancer.
In conclusion, the results of the present study suggest that, in gastric cancer cells, hypoxia may potentially regulate CD44 expression via HIF-1α in order to promote cell proliferation and invasion, which may be a potential target for the treatment of gastric cancer in the future.
Acknowledgements
The present study was supported by the Youth Science and Technology Talent Project of Hubei Health Department (grant no. QJX2012-21).
References
- 1.Götte M, Yip GW. Heparanase, hyaluronan and CD44 in cancers: A breast carcinoma perspective. Cancer Res. 2006;66:10233–10237. doi: 10.1158/0008-5472.CAN-06-1464. [DOI] [PubMed] [Google Scholar]
- 2.Peng ST, Su CH, Kuo CC, Shaw CF, Wang HS. CD44 crosslinking-mediated matrix metalloproteinase-9 relocation in breast tumor cells leads to enhanced metastasis. Int J Oncol. 2007;31:1119–1126. [PubMed] [Google Scholar]
- 3.Go SI, Ko GH, Lee WS, Kim RB, Lee JH, Jeong SH, Lee YJ, Hong SC, Ha WS. CD44 Variant 9 serves as a poor prognostic marker in early gastric cancer, but not in advanced gastric cancer. Cancer Res Treat. 2016;48:142–152. doi: 10.4143/crt.2014.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao X, Cao D, Jin M, Jia Z, Kong F, Ma H, Wang Y, Jiang J. CD44 but not CD24 expression is related to poor prognosis in non-cardia adenocarcinoma of the stomach. BMC Gastroenterol. 2014;14:157. doi: 10.1186/1471-230X-14-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xue Z, Yan H, Li J, Liang S, Cai X, Chen X, Wu Q, Gao L, Wu K, Nie Y, Fan D. Identification of cancer stem cells in vincristine preconditioned SGC7901 gastric cancer cell line. J Cell Biochem. 2012;113:302–312. doi: 10.1002/jcb.23356. [DOI] [PubMed] [Google Scholar]
- 6.Takaishi S, Okumura T, Tu S, Wang SS, Shibata W, Vigneshwaran R, Gordon SA, Shimada Y, Wang TC. Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells. 2009;27:1006–1020. doi: 10.1002/stem.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keith B, Simon MC. Hypoxia-inducible factors, stem cells, and cancer. Cell. 2007;129:465–472. doi: 10.1016/j.cell.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panchision DM. The role of oxygen in regulating neural stem cells in development and disease. J Cell Physiol. 2009;220:562–568. doi: 10.1002/jcp.21812. [DOI] [PubMed] [Google Scholar]
- 9.Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;3:721–732. doi: 10.1038/nrc1187. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Li Z, Zhang H, Jin H, Sun L, Dong H, Xu M, Zhao P, Zhang B, Wang J, et al. HIF-1α and HIF-2α correlate with migration and invasion in gastric cancer. Cancer Biol Ther. 2010;10:376–382. doi: 10.4161/cbt.10.4.12441. [DOI] [PubMed] [Google Scholar]
- 11.Blenner JL. The therapeutic functions of companion animals in infertility. Holist Nurs Pract. 1991;5:6–10. doi: 10.1097/00004650-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Krishnamachary B, BergDixon S, Kelly B, Agani F, Feldser D, Ferreira G, Iyer N, LaRusch J, Pak B, Taghavi P, Semenza GL. Regulation of colon carcinoma cell invasion by hypoxia-inducible factor 1. Cancer Res. 2003;63:1138–1143. [PubMed] [Google Scholar]
- 13.Sumiyoshi Y, Kakeji Y, Egashira A, Mizokami K, Orita H, Maehara Y. Overexpression of hypoxia-inducible factor 1alpha and p53 is a marker for an unfavorable prognosis in gastric cancer. Clin Cancer Res. 2006;12:5112–5117. doi: 10.1158/1078-0432.CCR-05-2382. [DOI] [PubMed] [Google Scholar]
- 14.Urano N, Fujiwara Y, Doki Y, Tsujie M, Yamamoto H, Miyata H, Takiguchi S, Yasuda T, Yano M, Monden M. Overexpression of hypoxia-inducible factor-1 alpha in gastric adenocarcinoma. Gastric Cancer. 2006;9:44–49. doi: 10.1007/s10120-005-0356-1. [DOI] [PubMed] [Google Scholar]
- 15.Rohwer N, Lobitz S, Daskalow K, Jöns T, Vieth M, Schlag PM, Kemmner W, Wiedenmann B, Cramer T, Höcker M. HIF-1alpha determines the metastatic potential of gastric cancer cells. Br J Cancer. 2009;100:772–781. doi: 10.1038/sj.bjc.6604919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krishnamachary B, Penet MF, Nimmagadda S, Mironchik Y, Raman V, Solaiyappan M, Semenza GL, Pomper MG, Bhujwalla ZM. Hypoxia regulates CD44 and its variant isoforms through HIF-1α in triple negative breast cancer. PLoS One. 2012;7:e44078. doi: 10.1371/journal.pone.0044078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hashimoto K, Aoyagi K, Isobe T, Kouhuji K, Shirouzu K. Expression of CD133 in the cytoplasm is associated with cancer progression and poor prognosis in gastric cancer. Gastric Cancer. 2014;17:97–106. doi: 10.1007/s10120-013-0255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alain Ravauda, Hervé Wallerand. Molecular pathways in metastatic renal cell carcinoma: The evolving role of mammalian target of rapamycin inhibitors. European Urology. 2009;8:793–798. doi: 10.1016/j.eursup.2009.08.001. [DOI] [Google Scholar]
- 19.Li GG, Li L, Li C, Ye LY, Li XW, Liu DR, Bao Q, Zheng YX, Xiang DP, Chen L, Chen J. Influence of up-regulation of Notch ligand DLL4 on biological behaviors of human gastric cancer cells. World J Gastroenterol. 2013;19:4486–4494. doi: 10.3748/wjg.v19.i28.4486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 21.Xu D, Zhang B, Liang G, Ping J, Kou H, Li X, Xiong J, Hu D, Chen L, Magdalou J, Wang H. Caffeine-induced activated glucocorticoid metabolism in the hippocampus causes hypothalamic-pituitary-adrenal axis inhibition in fetal rats. PLoS One. 2012;7:e44497. doi: 10.1371/journal.pone.0044497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Torre LA, Bray F, Siegel RL, Ferlay J, LortetTieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 23.Hartgrink HH, Jansen EP, van Grieken NC, van de Velde CJ. Gastric cancer. Lancet. 2009;374:477–490. doi: 10.1016/S0140-6736(09)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan IB, Ivanova T, Lim KH, Ong CW, Deng N, Lee J, Tan SH, Wu J, Lee MH, Ooi CH, et al. Intrinsic subtypes of gastric cancer, based on gene expression pattern, predict survival and respond differently to chemotherapy. Gastroenterology. 2011;141:476–485. doi: 10.1053/j.gastro.2011.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim B, Bang S, Lee S, Kim S, Jung Y, Lee C, Choi K, Lee SG, Lee K, Lee Y, et al. Expression profiling and subtype-specific expression of stomach cancer. Cancer Res. 2003;63:8248–8255. [PubMed] [Google Scholar]
- 26.Clarke MF, Dick JE, Dirks PB, Eaves CJ, Jamieson CH, Jones DL, Visvader J, Weissman IL, Wahl GM. Cancer stem cells-perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer Res. 2006;66:9339–9344. doi: 10.1158/0008-5472.CAN-06-3126. [DOI] [PubMed] [Google Scholar]
- 27.Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–284. doi: 10.1038/nrc1590. [DOI] [PubMed] [Google Scholar]
- 28.Jang BI, Li Y, Graham DY, Cen P. The Role of CD44 in the Pathogenesis, Diagnosis and Therapy of Gastric Cancer. Gut Liver. 2011;5:397–405. doi: 10.5009/gnl.2011.5.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagano O, Saya H. Mechanism and biological significance of CD44 cleavage. Cancer Sci. 2004;95:930–935. doi: 10.1111/j.1349-7006.2004.tb03179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ponta H, Sherman L, Herrlich PA. CD44: From adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol. 2003;4:33–45. doi: 10.1038/nrm1004. [DOI] [PubMed] [Google Scholar]
- 31.Guo J, Wang B, Fu Z, Wei J, Lu W. Hypoxic Microenvironment Induces EMT and Upgrades Stem-Like Properties of Gastric Cancer Cells. Technol Cancer Res Treat. 2016;15:60–68. doi: 10.1177/1533034614566413. [DOI] [PubMed] [Google Scholar]
- 32.Matsumoto K, Arao T, Tanaka K, Kaneda H, Kudo K, Fujita Y, Tamura D, Aomatsu K, Tamura T, Yamada Y, et al. mTOR signal and hypoxia-inducible factor-1 alpha regulate CD133 expression in cancer cells. Cancer Res. 2009;69:7160–7164. doi: 10.1158/0008-5472.CAN-09-1289. [DOI] [PubMed] [Google Scholar]
- 33.Platet N, Liu SY, Atifi ME, Oliver L, Vallette FM, Berger F, Wion D. Influence of oxygen tension on CD133 phenotype in human glioma cell cultures. Cancer Lett. 2007;258:286–290. doi: 10.1016/j.canlet.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 34.Fujikuni N, Yamamoto H, Tanabe K, Naito Y, Sakamoto N, Tanaka Y, Yanagihara K, Oue N, Yasui W, Ohdan H. Hypoxia-mediated CD24 expression is correlated with gastric cancer aggressiveness by promoting cell migration and invasion. Cancer Sci. 2014;105:1411–1420. doi: 10.1111/cas.12522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu HL, Liu D, Ding GR, Liao PF, Zhang JW. Hypoxia-inducible factor-1α and Wnt/β-catenin signaling pathways promote the invasion of hypoxic gastric cancer cells. Mol Med Rep. 2015;12:3365–3373. doi: 10.3892/mmr.2015.3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazumdar J, O'Brien WT, Johnson RS, LaManna JC, Chavez JC, Klein PS, Simon MC. O2 regulates stem cells through Wnt/β-catenin signalling. Nat Cell Biol. 2010;12:1007–1013. doi: 10.1038/ncb2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braunschweig L, Meyer AK, Wagenführ L, Storch A. Oxygen regulates proliferation of neural stem cells through Wnt/β-catenin signalling. Mol Cell Neurosci. 2015;67:84–92. doi: 10.1016/j.mcn.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 38.Siapati EK, Papadaki M, Kozaou Z, Rouka E, Michali E, Savvidou I, Gogos D, Kyriakou D, Anagnostopoulos NI, Vassilopoulos G. Proliferation and bone marrow engraftment of AML blasts is dependent on β-catenin signalling. Br J Haematol. 2011;152:164–174. doi: 10.1111/j.1365-2141.2010.08471.x. [DOI] [PubMed] [Google Scholar]