Approximately 20 years after identification of mutations in genes associated with breast cancer (BRCA-1,2), the number of women having BRCA-1,2 tests doubled after the famous artist Angelina Jolie who was a BRCA-1 carrier underwent bilateral prophylactic mastectomy (1). The number of women having prophylactic bilateral mastectomy based on a positive test is also increasing. These results emphasize the role of a well-known person in creating awareness.
Breast-conserving surgery has been a standard in breast cancer surgery for nearly thirty years, and currently lack of ink staining on the specimen is considered as a negative surgical margin. However, the surgical treatment of women diagnosed with breast cancer and carry BRCA-1,2 is not yet standard. In this group of patients, the treatment of choice is bilateral subcutaneous mastectomy and salpingo-oophorectomy over the age of 40 years, while at a younger age, in patients who desire to give birth and breastfeed; the decision to choose such a treatment is usually difficult.
Currently, it is accepted that the diagnosis and treatment of breast cancer should be individualized, and planning should be made according to the patient’s and the tumor’s clinical and genetic characteristics. Similarly, the decision for surgical treatment should be based on patient’ age and tumor characteristics in BRCA 1,2 carriers. This article focuses on an actual young, nulliparous patient who was diagnosed with breast cancer.
Case Presentation
Our patient AK is 33 years old, has a mass in the upper outer quadrant of the right breast. She is nulliparous, age at first menstruation is 9 years. On physical examination, both breasts are dense; there is a 15 mm nodular mass on her right breast at 9 o’clock position, with no palpable axillary node. On mammography an asymmetrical density, and on ultrasonography a lobulated, hypovascular mass was observed on her right breast, which was considered as degenerated fibroadenoma (Figure 1, 2). On MRI, the lesion on the upper outer quadrant of the right breast showed cystic degeneration and Type II curve (Figure 3). The tru-cut biopsy was invasive ductal carcinoma, with triple-negative molecular subtype. Pedigree history showed that her mother’s grandmother and mother’s aunt had breast, her grandmother and mother had ovarian cancer. Her genetic testing for BRCA 1 and 2 mutations was positive. In addition, she had clinical stage I breast cancer.
Figure 1.
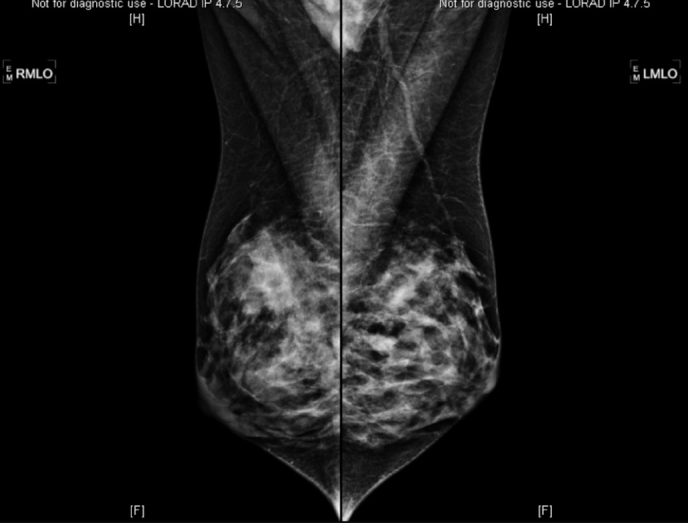
The pre-operative mammogram of the patient: an asymmetrical image on the upper external quadrant of the right breast on MLO graph
Figure 2.

A lobular, hypovascular mass suggesting degenerative fibroadenoma in the right breast at 9 o’clock on the pre-operative ultrasonography of the patient
Figure 3.
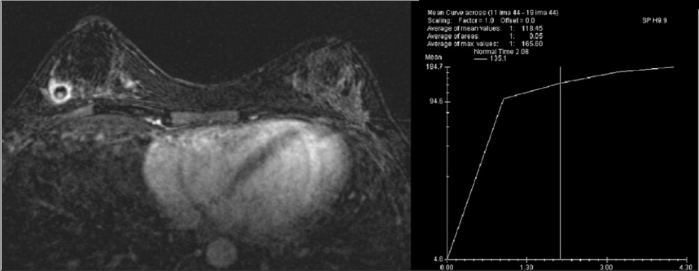
A mass with cystic degeneration and a Type II curve on the upper external quadrant of the right breast on the pre-operative MRI of the patient
Question
If this patient diagnosed with right breast cancer, and she did not have BRCA mutation, which type of surgery would be suggested?
Lumpectomy + sentinel lymph node biopsy (SLNB)
Mastectomy + SLNB
Subcutaneous mastectomy + silicone prosthesis reconstruction + SLNB
Answer
In a patient with right-sided breast cancer and no genetic carrier status, the ideal surgical treatment to be offered is lumpectomy-SLNB, if the breast tumor ratio is appropriate. If the patient previously received radiation therapy to the chest wall, or radiation therapy is contraindicated due to collagen disease (lupus erythematosus, dermatomyositis, etc.), or if she prefers mastectomy, or if radiotherapy is necessary after subcutaneous mastectomy + reconstruction, then classic mastectomy + SLNB can be performed. If the patient prefers mastectomy and radiation therapy is not required, subcutaneous mastectomy + silicone prosthesis reconstruction+ SLNB may be suggested as a third alternative.
Question
If this patient diagnosed with right breast cancer had BRCA mutation, which type of surgery would be suggested?
Right lumpectomy + SLNB
Right mastectomy + SLNB
Right subcutaneous mastectomy + SLNB; Left prophylactic mastectomy + SLNB
In a recent prospective analysis (EMBRACE study), 978 BRCA-1 and 909 BRCA-2 mutation carriers were evaluated and the risk until 70 years of age in BRCA-1 carriers was reported as 60% (44–75%) for breast cancer, 59% for ovarian cancer (%43–76), 83% for another breast cancer (69–94%) (2). The risk in BRCA-2 carriers is 55% (% 41–70) for breast cancer, 16.5% (7.5–34%) for ovarian cancer, and 62%% (44–79.5%) for contraletaral breast cancer (2–3).
Breast conserving surgery and radiotherapy are being implemented as a standard treatment for a long time in early-stage and selected breast cancer patients with a similar survival rate to mastectomy (3, 4). Nevertheless, several aspects should be considered in the decision making process for surgical treatment in BRCA carriers with breast cancer: 1. Local recurrence within the same breast, risk of contra-lateral breast cancer, 2. The effect of prophylactic mastectomy on survival, 3. The factors that increase or decrease the risk of breast cancer on the same or the opposite breast. Most of the studies regarding these questions are retrospective studies with controversial results (5–14).
Answers
If this patient diagnosed with right breast cancer had BRCA mutation, which type of surgery would be suggested?
1. Right lumpectomy + SLNB
Local recurrence in BRCA mutation carriers with breast cancer undergoing breast-conserving surgery (BCS)
In a meta-analysis, twenty-three studies were found to be eligible for evaluation. In 10 of these, local recurrence rates following breast conserving surgery (BCS) in patients with and without the mutation were evaluated (15). The local recurrence rate was 17% in BRCA mutation carriers, while this rate was 11% in patients without BRCA mutation and this difference was not statistically significant (p=0.07). Whether the patient has or does not have BRCA-1 or 2 mutation does not affect the patients’ local recurrence rate (p=0.2). This result shows that local treatment with radiotherapy is equally effective in patients with mutation carriers. With longer follow-up, local recurrence rate increases in mutation carriers; this can be explained by detection of true local recurrence in these patients.
Overall survival in BRCA mutation carriers with breast cancer undergoing breast-conserving surgery (BCS)
Survival rates of breast cancer patients with or without mutation undergoing BCS were identified to be similar in studies regarding overall survival and breast cancer related survival rates (10, 15).
In one of the studies on breast cancer-specific survival rate, there was no difference in terms of survival in 5-year follow-up. On the other hand, another study reported higher mortality rates in mutation carriers at 116 months of follow-up (15, 16).
Factors that increase the risk of local recurrence in BRCA mutation carriers diagnosed with breast cancer undergoing BCS
Factors increasing local/regional recurrence in the same breast or contra-lateral breast cancer should be taken into account in the decision making process for surgical treatment of mutation carriers with breast cancer, and it should be decided if these risk factors mandate a more radical surgical treatment. It was reported that adjuvant chemotherapy, the use of tamoxifen and bilateral salpingo-oopherectomy (BSO) reduced local recurrence rate following BCS (15). Age, surgical margins, axillary involvement, tumor stage, grade, and estrogen receptor positivity were not shown to be associated with local recurrence.
Adjuvant chemotherapy and BSO reduces local recurrence by 50% in the same breast: BRCA1/2-associated breast cancer is more sensitive to chemotherapy, in addition, the observed reduction in risk in carrier patients with breast cancer and BSO is similar to the risk reduction by BSO in carriers without breast cancer (17). Consequently, in carriers with breast cancer, aggressive surgery (mastectomy, mastectomy + contra-lateral prophylactic mastectomy) may be more appropriate if BSO is not performed.
2. Right mastectomy and sentinel lymph node biopsy
Local recurrence after mastectomy for breast cancer in BRCA mutation carriers
There is only one study comparing local recurrence in BRCA mutation carriers with breast cancer after mastectomy and breast conserving surgery (16, 17). This study reported quite high local recurrence rates after 15 years in BCS (23.5% and 5.5%), however, breast cancer specific (92.8% and 93.5%) and overall survival rates (89.8% and 93.8%) were similar.
Local recurrences were mostly in the form of new primary in mutation carriers and as true recurrences after mastectomy. The difference in survival between BCS and mastectomy is related to the more frequent true recurrences, which have a worse prognosis, in mutation carriers following BCS (18, 19).
3. Right subcutaneous mastectomy + SLNB; Left prophylactic mastectomy + SLNB
Contra-lateral breast cancer risk in BRCA mutation carriers
In a meta-analysis published last year and included 14 studies, it was identified that contra-lateral prophylactic mastectomy in BRCA carriers and/or patients with family history of breast cancer reduces the risk of metachronous breast cancer, but it did not affect overall or disease-specific survival rates (20).
Another meta-analysis evaluated the risk of cancer in the opposite breast in breast cancer patients with and without BRCA mutation (15). This risk was 24% in BRCA carriers, and 7% in patients without the mutation, in other words, the risk was 3.5 times higher in mutation carriers.
Contra-lateral breast cancer risk in BRCA-1 and BRCA-2 mutation carriers
Studies on the risk of contra-lateral breast cancer in breast cancer patients reported contra-lateral breast cancer rate as 21% for BRCA-1 carriers, and as 15% in BRCA-2 carriers (15). Carriers of BRCA 1 have been identified to display more aggressive molecular subtypes (triple negative and basal like) than BRCA-2 carriers. Additionally, it was reported that tamoxifen or prophylactic BSO had more protective effect in BRCA-2 mutation carriers, and BRCA-1 carriers show more estrogen receptor negativity.
Risk factors for contra-lateral breast cancer in BRCA mutation carriers
Bilateral salpingo-oopherectomy (BSO), older age at diagnosis (>50), tamoxifen and adjuvant chemotherapy were found to be important factors in reducing the risk of cancer in the contra-lateral breast in BRCA mutation carriers (15). Adjuvant tamoxifen and BSO are known to decrease the risk of cancer in the contra-lateral breast by 50%. Continuing treatment with aromatase enzyme inhibitors following BSO will further reduce the risk of contra-lateral breast cancer. Contra-lateral breast cancer risk is decreased in relation to more advanced age on diagnosis. As a result, mastectomy to the breast with cancer and prophylactic mastectomy for the other breast may be preferred in women without BSO or tamoxifen.
Overall and disease-specific survival rates after mastectomy – contra-lateral prophylactic mastectomy for breast cancer in BRCA mutation carriers
In studies comparing BRCA carriers undergoing mastectomy to the cancer-bearing breast and prophylactic mastectomy to the opposite side with mastectomy alone, it has been shown that contra-lateral prophylactic mastectomy did not increase survival (10–16).
Bilateral mastectomy prevents breast cancer development in the contralateral breast to a large extent in BRCA-1,2 carriers (20). However, bilateral mastectomy was not identified to alter survival in another meta-analysis (15). Heemskerk-Gerritsen et al. (21) investigated the contribution of prophylactic mastectomy on survival, in patients with breast cancer who underwent prophylactic contralateral mastectomy in the Netherlands. The median follow-up of the patients was 11.4 years, and the risk of contralateral breast cancer was significantly lower in patients with prophylactic mastectomy. The mortality rate was 9.6% in the group with contralateral mastectomy, while it was 21.6% in the group without this procedure. The mortality rate was higher especially in patients under the age of 40, those not receiving chemotherapy, primary cancer with triple negative molecular subtype, and histological grade 3. However, in this study, patients who underwent mastectomy received more systemic therapy; and this difference can be explained by the fact that BRCA mutation carriers are more sensitive to chemotherapy (22, 23). Therefore, the survival benefit of prophylactic mastectomy to the contralateral breast remains unanswered, requiring prospective randomized studies in this regard.
Psychosocial and emotional effects of prophylactic mastectomy
An important and unique aspect of prophylactic mastectomy is psychosocial and emotional consequences related to such a procedure. Some studies showed that psychosocial effects and quality of life were similar in patients with and without prophylactic mastectomy (24–26), whereas other studies indicate that it has a negative impact on body image and sexuality (24–26). Therefore, when choosing the most appropriate surgical treatment for breast cancer in mutation carriers, psychosocial aspects should also be taken into consideration.
Available data do not allow us to create clinical guidelines for the surgical treatment of unilateral breast cancer in BRCA mutation carriers. Therefore, each patient should be assessed individually by clinical, pathological, and psychosocial features. For that reason, discussing details with the patient before making a final decision for surgery, and asking for psychologic and genetic consultations will be quite helpful in the mutual selection of treatment. This discussion should include new evidence on the reliability of BCS in providing oncologic safety, the 3.5-fold increased risk of contra-lateral breast cancer, the psychosocial consequences of prophylactic mastectomy, and the presence of proven factors that alter local recurrence and contra-lateral breast cancer risks.
In conclusion, our patient who was 33 years of age at diagnosis underwent lumpectomy+ SLNB based on her age, nulli-parity and her own choice. Stage I [pT1c (12 mm) N0 M0], triple negative, Ki-67 85% breast cancer was identified. Chemotherapy with adriamycin and taxanes, radiotherapy and tamoxifen were used as adjuvant therapy. Her physical examination and radiographic examinations are normal at postoperative 3 years (Figures 4–6). The patient was suggested to undergo bilateral subcutaneous mastectomy + reconstruction at age 40.
Figure 4.
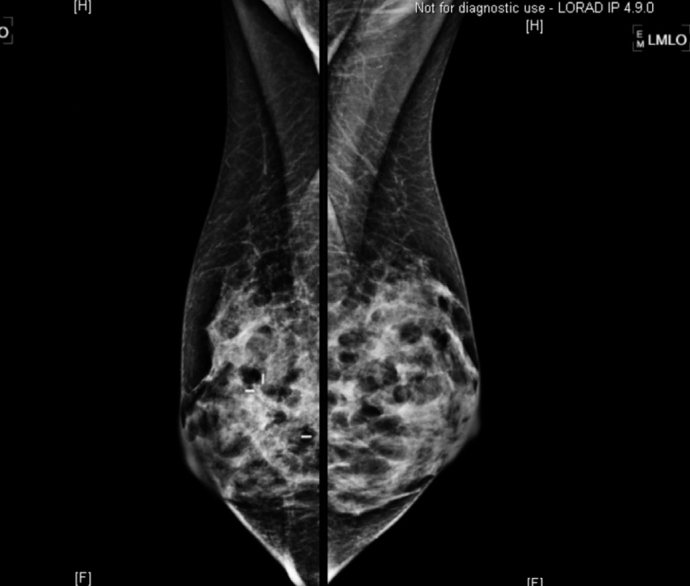
Normal appearance of the right breast on the post-operative mammogram of the patient at the postoperative third year
Figure 5.
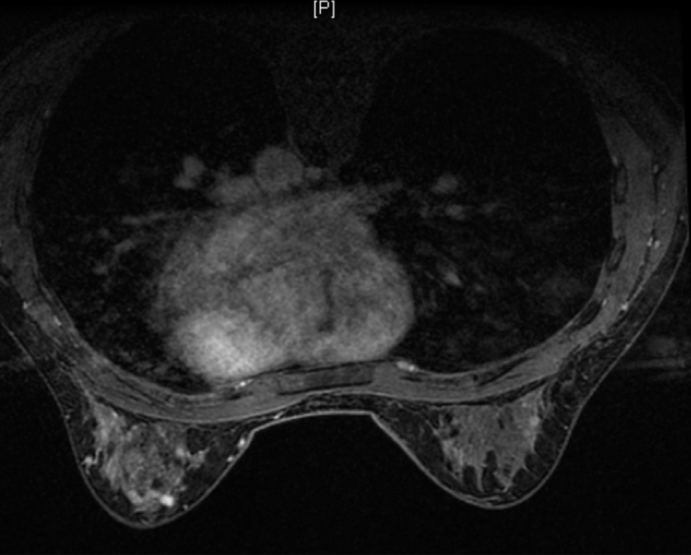
Normal appearance of the right breast on the post-operative MRI of the patient at the postoperative third year
Figure 6.

Appearance at the postoperative third year
References
- 1.Evans DG, Barwell J, Eccles DM, Collins A, Izatt L, Jacobs C, Donaldson A, Brady AF, Cuthbert A, Harrison R, Thomas S, Howell A FH02 Study Group; RGC teams. Miedzybrodzka Z, Murray A. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res. 2014;16:442. doi: 10.1186/s13058-014-0442-6. http://dx.doi.org/10.1186/s13058-014-0442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mavaddat N, Peock S, Frost D, Ellis S, Platte R, Fineberg E, Evans DG, Izatt L, Eeles RA, Adlard J, Davidson R, Eccles D, Cole T, Cook J, Brewer C, Tischkowitz M, Douglas F, Hodgson S, Walker L, Porteous ME, Morrison PJ, Side LE, Kennedy MJ, Houghton C, Donaldson A, Rogers MT, Dorkins H, Miedzybrodzka Z, Gregory H, Eason J, Barwell J, McCann E, Murray A, Antoniou AC, Easton DF EMBRACE. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst. 2013;105:812–822. doi: 10.1093/jnci/djt095. http://dx.doi.org/10.1093/jnci/djt095. [DOI] [PubMed] [Google Scholar]
- 3.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. http://dx.doi.org/10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366:2087–2106. doi: 10.1016/S0140-6736(05)67887-7. http://dx.doi.org/10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 5.Brekelmans CT, Tilanus-Linthorst MM, Seynaeve C, vd Ouweland A, Menke-Pluymers MB, Bartels CC, Kriege M, van Geel AN, Burger CW, Eggermont AM, Meijers-Heijboer H, Klijn JG. Tumour characteristics, survival and prognostic factors of hereditary breast cancer from BRCA2-, BRCA1- and non- BRCA1/2 families as compared to sporadic breast cancer cases. Eur J Cancer. 2007;43:867–876. doi: 10.1016/j.ejca.2006.12.009. http://dx.doi.org/10.1016/j.ejca.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Eccles D, Simmonds P, Goddard J, Coultas M, Hodgson S, Lalloo F, Evans G, Haites N. Familial breast cancer: an investigation into the outcome of treatment for early stage disease. Fam Cancer. 2001;1:65–72. doi: 10.1023/a:1013867917101. http://dx.doi.org/10.1023/A:1013867917101. [DOI] [PubMed] [Google Scholar]
- 7.El-Tamer M, Russo D, Troxel A, Bernardino LP, Mazziotta R, Estabrook A, Ditkoff BA, Schnabel F, Mansukhani M. Survival and recurrence after breast cancer in BRCA1/2 mutation carriers. Ann Surg Oncol. 2004;11:157–164. doi: 10.1245/aso.2004.05.018. http://dx.doi.org/10.1245/ASO.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Etienne CA, Barile M, Gentilini OD, Botteri E, Rotmensz N, Sagona A, Farante G, Galimberti V, Luini A, Veronesi P, Bonanni B. Breast conserving surgery in BRCA1/2 mutation carriers: are we approaching an answer? Ann Surg Oncol. 2009;16:3380–3387. doi: 10.1245/s10434-009-0638-7. http://dx.doi.org/10.1245/s10434-009-0638-7. [DOI] [PubMed] [Google Scholar]
- 9.Haffty BG, Harrold E, Khan AJ, Pathare P, Smith TE, Turner BC, Glazer PM, Ward B, Carter D, Matloff E, Bale AE, Franco MA. Outcome of conservatively managed early-onset breast cancer by BRCA1/2 status. Lancet. 2002;359:1471–1477. doi: 10.1016/S0140-6736(02)08434-9. http://dx.doi.org/10.1016/S0140-6736(02)08434-9. [DOI] [PubMed] [Google Scholar]
- 10.Kirova YM, Savignoni A, Sigal-Zafrani B, de La Rochefordiere A, Salmon RJ, This P, Asselain B, Stoppa-Lyonnet D, Fourquet A. Is the breast-conserving treatment with radiotherapy appropriate in BRCA1/2 mutation carriers? Long-term results and review of the literature. Breast Cancer Res Treat. 2010;120:119–126. doi: 10.1007/s10549-009-0685-6. http://dx.doi.org/10.1007/s10549-009-0685-6. [DOI] [PubMed] [Google Scholar]
- 11.Metcalfe K, Lynch HT, Ghadirian P, Tung N, Kim-Sing C, Olopade OI, Domchek S, Eisen A, Foulkes WD, Rosen B, Vesprini D, Sun P, Narod SA. Risk of ipsilateral breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat. 2011;127:287–296. doi: 10.1007/s10549-010-1336-7. http://dx.doi.org/10.1007/s10549-010-1336-7. [DOI] [PubMed] [Google Scholar]
- 12.Pierce LJ, Phillips KA, Griffith KA, Buys S, Gaffney DK, Moran MS, Haffty BG, Ben-David M, Kaufman B, Garber JE, Merajver SD, Balmaña J, Meirovitz A, Domchek SM. Local therapy in BRCA1 and BRCA2 mutation carriers with operable breast cancer: comparison of breast conservation and mastectomy. Breast Cancer Res Treat. 2010;121:389–398. doi: 10.1007/s10549-010-0894-z. http://dx.doi.org/10.1007/s10549-010-0894-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robson ME, Chappuis PO, Satagopan J, Wong N, Boyd J, Goffin JR, Hudis C, Roberge D, Norton L, Begin LR, Offit K, Foulkes WD. A combined analysis of outcome following breast cancer: differences in survival based on BRCA1/BRCA2 mutation status and administration of adjuvant treatment. Breast Cancer Res. 2004;6:R8–R17 16. doi: 10.1186/bcr658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stoppa-Lyonnet D, Ansquer Y, Dreyfus H, Gautier C, Gauthier-Villars M, Bourstyn E, Clough KB, Magdelénat H, Pouillart P, Vincent-Salomon A, Fourquet A, Asselain B. Familial invasive breast cancers: worse outcome related to BRCA1 mutations. J Clin Oncol. 2001;18:4053–4059. doi: 10.1200/JCO.2000.18.24.4053. [DOI] [PubMed] [Google Scholar]
- 15.Valachis A, Nearchou AD, Lind P. Surgical management of breast cancer in BRCA-mutation carriers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014;144:443–455. doi: 10.1007/s10549-014-2890-1. http://dx.doi.org/10.1007/s10549-014-2890-1. [DOI] [PubMed] [Google Scholar]
- 16.Rennert G, Bisland-Naggan S, Barnett-Griness O, Bar-Joseph N, Zhang S, Rennert HS, Narod SA. Clinical outcomes of breast cancer in carriers of BRCA1 and BRCA2 mutations. N Engl J Med. 2007;357:115–123. doi: 10.1056/NEJMoa070608. http://dx.doi.org/10.1056/NEJMoa070608. [DOI] [PubMed] [Google Scholar]
- 17.Fayanju OM, Stoll CR, Fowler S, Colditz GA, Margenthaler JA. Contralateral prophylactic mastectomy after unilateral breast cancer: a systematic review and meta-analysis. Ann Surg. 2014;260:1000–1010. doi: 10.1097/SLA.0000000000000769. http://dx.doi.org/10.1097/SLA.0000000000000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang E, Buchholz TA, Meric F, Krishnamurthy S, Mirza NQ, Ames FC, Feig BW, Kuerer HM, Ross MI, Singletary SE, McNeese MD, Strom EA, Hunt KK. Classifying local disease recurrences after breast conservation therapy based on location and histology: new primary tumors have more favorable outcomes than true local disease recurrences. Cancer. 2002;95:2059–2067. doi: 10.1002/cncr.10952. http://dx.doi.org/10.1002/cncr.10952. [DOI] [PubMed] [Google Scholar]
- 19.Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev. 2010;11:CD002748. doi: 10.1002/14651858.CD002748.pub3. http://dx.doi.org/10.1002/14651858.cd002748.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Rhiem K, Schmutzler R. Impact of Prophylactic Mastectomy in BRCA1/2 Mutation Carriers. Breast Care (Basel) 2014;9:385–389. doi: 10.1159/000369592. http://dx.doi.org/10.1159/000369592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heemskerk-Gerritsen BA, Rookus MA, Aalfs CM, Ausems MG, Collée JM, Jansen L, Kets CM, Keymeulen KB, Koppert LB, Meijers-Heijboer HE, Mooij TM, Tollenaar RA, Vasen HF HEBON. Hooning MJ, Seynaeve C. Improved overall survival after contralateral risk-reducing mastectomy in BRCA1/2 mutation carriers with a history of unilateral breast cancer: a prospective analysis. Int J Cancer. 2015;136:668–677. doi: 10.1002/ijc.29032. [DOI] [PubMed] [Google Scholar]
- 22.Fourquet A, Stoppa-Lyonnet D, Kirova YM, Sigal-Zafrani B, Asselain B Institut Curie Breast Cancer Study Group, Institut Curie Breast Ovary Cancer Risk Study Group. Familial breast cancer: clinical response to induction chemotherapy or radiotherapy related to BRCA1/2 mutations status. Am J Clin Oncol. 2009;32:127–131. doi: 10.1097/COC.0b013e31817f9e1c. http://dx.doi.org/10.1097/COC.0b013e31817f9e1c. [DOI] [PubMed] [Google Scholar]
- 23.Kriege M, Seynaeve C, Meijers-Heijboer H, Collee JM, Menke-Pluymers MB, Bartels CC, Tilanus-Linthorst MM, Blom J, Huijskens E, Jager A, van den Ouweland A, van Geel B, Hooning MJ, Brekelmans CT, Klijn JG. Sensitivity to first-line chemotherapy for metastatic breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2009;27:3764–3771. doi: 10.1200/JCO.2008.19.9067. http://dx.doi.org/10.1200/JCO.2008.19.9067. [DOI] [PubMed] [Google Scholar]
- 24.Brandberg Y, Sandelin K, Erikson S, Jurell G, Liljegren A, Lindblom A, Lindén A, von Wachenfeldt A, Wickman M, Arver B. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol. 2008;26:3943–3949. doi: 10.1200/JCO.2007.13.9568. http://dx.doi.org/10.1200/JCO.2007.13.9568. [DOI] [PubMed] [Google Scholar]
- 25.Tercyak KP, Peshkin BN, Brogan BM, DeMarco T, Pennanen MF, Willey SC, Magnant CM, Rogers S, Isaacs C, Schwartz MD. Quality of life after contralateral prophylactic mastectomy in newly diagnosed high-risk breast cancer patients who underwent BRCA1/2 gene testing. J Clin Oncol. 2007;25:285–291. doi: 10.1200/JCO.2006.07.3890. http://dx.doi.org/10.1200/JCO.2006.07.3890. [DOI] [PubMed] [Google Scholar]
- 26.Frost MH, Slezak JM, Tran NV, Williams CI, Johnson JL, Woods JE, Petty PM, Donohue JH, Grant CS, Sloan JA, Sellers TA, Hartmann LC. Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol. 2005;23:7849–7856. doi: 10.1200/JCO.2005.09.233. http://dx.doi.org/10.1200/JCO.2005.09.233. [DOI] [PubMed] [Google Scholar]


