Abstract
Cigarette smoke (CS) increases the risk of chronic obstructive pulmonary disease (COPD) by causing inflammation, emphysema, and reduced lung function. Additionally, CS can induce autophagy which contributes to COPD. Arachidonic acid-derived epoxyeicosatrienoic acids (EETs) have promising anti-inflammatory properties that may protect the heart and liver by regulating autophagy. For this reason, the effect of decreased soluble epoxide hydrolase (sEH, Ephx2)-mediated EET hydrolysis on inflammation, emphysema, lung function, and autophagy was here studied in CS-induced COPD in vivo. Adult male wild-type (WT) C57BL/6J and Ephx2−/− mice were exposed to air or CS for 12 weeks, and lung inflammatory responses, air space enlargement (emphysema), lung function, and autophagy were assessed. Lungs of Ephx2−/− mice had a less pronounced inflammatory response and less autophagy with mild distal airspace enlargement accompanied by restored lung function and steady weight gain. These findings support the idea that Ephx2 may hold promise as a therapeutic target for COPD induced by CS, and it may be protective property by inhibiting autophagy.
KEY WORDS: Ephx2, epoxyeicosatrienoic acids, inflammation, autophagy, cigarette smoke
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is an inflammatory disease characterized by emphysema, persistent airflow limitations, and reduced lung function [31]. It is the third leading cause of death worldwide and it represents an important public health challenge [44]. Cigarette smoking (CS) is the main risk factor for developing COPD and airway inflammation, which contributes to airway remodeling and pulmonary emphysema [42].
Chronic exposure to CS leads to lung inflammation and increased levels of macrophages [37], neutrophils [8, 16], and dendritic cells (DCs) [40]. An uncontrolled and prolonged inflammatory response may destroy lung tissue and promote remodeling [5, 36]. Elimination of inflammation is a key treatment target for COPD.
Epoxyeicosatrienoic acids (EETs), arachidonic acid-derived epoxides, are important regulators of inflammation and vascular homeostasis [6]. Manipulating them may be a suitably anti-inflammatory pharmacological strategy. Notably, arachidonic acid is metabolized by CYP epoxygenase enzymes, CYP2C and CYP2J subfamilies, to biologically active EETs [46]. Then EETs are hydrolyzed by soluble epoxide hydrolase (sEH, Ephx2) to dihydroxyeicosatrienoic acid (DHETs), which have less biological function [46]. EETs are found in numerous organs such as the lung, kidney, heart, liver, and brain [12, 47]. They have anti-inflammatory effects on human bronchi [23]. A sEH inhibitor has been found to attenuate CS-induced inflammation in mouse models as well [32]. Nording and colleagues showed TNF-α mRNA expression to be significantly decreased in animals treated with a sEH inhibitor and in Ephx2−/− animals in response to sub-chronic tobacco smoke (TS) exposure [30]. Previous studies have suggested that EETs disrupt NF-κB signaling to exert anti-inflammatory effects [9, 29]. However, the phenotypic influence of Ephx2 disruption on inflammation in response to chronic CS is unclear.
Autophagy is a dynamic process involving cytoplasmic organelle and protein turnover via a lysosome-associated degradation pathway. Material is engulfed by autophagosomes and then fuses with lysosomes to be degraded by lysosomal hydrolases. Starvation, oxidative stress, cytokines, and xenobiotics can induce autophagy, suggesting it is important for maintaining cellular homeostasis and adapting to adverse environments [13, 17, 18]. Autophagy contributes to lung disease, exerting effects on fundamental cellular processes such as inflammation, apoptosis, redox balance, and proliferation [21, 26, 27]. COPD patients have more autophagy in epithelial cells than in healthy individuals [25–27] and previous studies have suggested that autophagy contributes to inflammation and emphysema in COPD [1, 3, 4]. López-Vicario and Samokhvalov reported that EETs modulate autophagic response and inhibit inflammation in fatty livers of obese subjects and improved starved cardiac cell viability and recovery [19, 35]. However, the effect of EETs or decreased soluble epoxide hydrolase (sEH, Ephx2)-mediated EET hydrolysis on autophagy in CS-induced COPD is less well understood. For this reason, we here investigated whether Ephx2 deficiency could modulate inflammation and autophagy in COPD and influences emphysema and lung function using Ephx2 (sEH) knockout (Ephx2−/−) and wild-type (WT) mice and a mouse model of CS-induced COPD.
MATERIALS AND METHODS
Mice
Ephx2−/− mice were a gift from the Yi Zhu Laboratory (Tian Jin Medical University, Tian Jing, China). Mice were backcrossed with C57BL/6J mice for five generations prior to use to produce heterozygous Ephx2+/− offspring. Ephx2+/− offspring was intercrossed to generate Ephx2+/+ and Ephx2−/− mice. All animals were housed in a temperature- and humidity-controlled room and kept on a 12:12-h light/dark cycle. Clean food and water were given ad libitum. Tail snips were obtained for DNA extraction to identify murine genotype with PCR. Primers were as follows: F1: 5′-TGG CAC GAC CCT AAT CTT AGG TTC-3′; R1: 5′-TGC ACG CTG GCA TTT TAA CAC CAG-3′; R2: 5′-CCA ATG ACA AGA CGC TGG GCG-3′ [39]. Primer F1/R1 predicts a 338-base pair (bp) amplicon and indicates the Ephx2+/+, primer F1/R2 predicts a 295-bp product and it indicates Ephx2−/− [39]. Primers were designed by TIANGEN Biotech (Beijing) Co., Ltd and genotypic analysis was examined on 3% agarose gel (Lonza Rockland, Inc., Rockland, ME, USA). All animal studies were approved by the Animal Care and Use Committee of Capital Medical University.
Animal CS Exposure
WT and Ephx2−/− mice (10 to 12 weeks old, ∼18–20 g) were randomly divided into two groups (N = 10). WT controls and KO controls were exposed to filtered air. WT-CS and KO-CS groups were whole-body exposed to CS from ten cigarettes (11 mg tar, 0.8 mg nicotine/cigarette; Daqianmen, China) in a sealed 50-L metal exposure chamber. Mice were exposed to 10 cigarettes for 60 min per exposure, once daily for 12 weeks. During exposure, smoke was maintained between 80 and 100 ppm at 18% oxygen. Animal weight was measured once every 2 weeks.
Preparation of BALF and Cell Counts
After 12 weeks CS exposure, mice were sacrificed and bronchoalveolar lavage fluid (BALF) was obtained by cannulating the trachea and lavaging it three times with 0.5 ml of 0.9% sodium chloride. BALF cells were centrifuged with PBS at 1000×g for 10 min at 4 °C. Supernatants were collected and stored at −80 °C to measure inflammatory factors. Pelleted BALF cells were resuspended in 1 ml PBS, and erythrocytes, neutrophils, and monocytes were quantified with a LH 750 (Beckman Coulter, Miami, FL, USA).
Cytokine Analysis
TNF-α and IL-1β in BALF were measured with ELISA using mouse TNF-α and IL-1β ELISA MAX™ Deluxe (BioLegend, San Diego, CA, USA) according to manufacturer’s instructions. Each sample was assayed in triplicate.
Lung Histology and Quantification of Emphysema
After mice were sacrificed, their tracheas and lungs were removed and inflated with 4% paraformaldehyde at a pressure of 25 cm H2O. Tissues were embedded in paraffin, and 5-μm-thick sections were stained with hematoxylin and eosin (H&E). Alveolar size was quantified using the mean linear intercept (Lm) of the airspace which is a measurement of airspace enlargement (emphysema). Lm was measured in 10 randomly selected fields of tissue sections observed at a magnification of ×200.
Lung Function
Lung function was assessed with a ventilator for small animals (flexiVent™; SCIREQ, Montreal, QC, Canada). After 12 weeks of daily exposure to air or CS, mice were anesthetized with thiopental (250 mg/kg, ip, Sigma-Aldrich, St. Louis, MO, USA) and tracheostomized. Then, a 20G angiocatheter (BD Insyte, Sandy, UT, USA) was inserted into the trachea and a catheter was used to connect the angiocatheter and the ventilator. The tidal volume of the ventilator was set at 10 ml/kg, and respiratory rate was 120 breaths/min with a positive end-expiratory pressure of 3 cm H2O. Lung function was expressed as Newtonian resistance (Rn), respiratory system resistance (Rrs), respiratory system compliance (Crs), and respiratory system elasticity (Ers).
Immunohistochemistry
Lungs were removed and fixed in 4% paraformaldehyde overnight and then embedded in paraffin to obtain three consecutive 5-μm thick sections. Sections were de-paraffinized in xylene and rehydrated through graded alcohol, followed by rinsing in PBS. Sections were placed in EDTA-antigen retrieval buffer and then exposed to 3% H2O2 for 10 min to block endogenous peroxidase activity at room temperature. Samples were blocked with sheep serum for 15 min and incubated in LC3B, Beclin 1, and NFκB primary antibodies (Cell Signaling, Beverly, MA, USA) diluted in blocking sera (1:200) at 4 °C overnight. After incubation, slides were washed three times and incubated with biotinylated secondary antibodies (Cell Signaling, Beverly, MA, USA). A hen enzyme reaction was performed using peroxidase substrate and sections were counterstained with hematoxylin and dehydrated through graded alcohol, mounted with neutral gum and observed under an inverted phase contrast microscope (LeicaDMI3000 B; Leica, Solms, Germany) at ×400 magnification. The immunostaining intensity assessment was performed using Image-Pro Plus 6.0 software. Mean integrated optical density (IOD) was used to express the antigen spot color intensity. The nuclear NF-κB staining was performed by counting staining nucleus. Each group contained three sections from different mice.
Electron Microscopy
Lung tissues were fixed in 2.5% glutaraldehyde for 2 h and washed three times in PBS for 10 min at room temperature. Subsequently, tissues were post-fixed in 2% osmium tetroxide and washed three times in double-distilled H2O. Then tissue was dehydrated in a series of graded ethanol followed by embedding in agar 100 resin. Seventy nanometer sections were cut and post stained with uranyl acetate and lead citrate. Tissues were photographed with a FEI Morgagni 268D transmission electron microscope (FEI, Eindhoven, Netherlands) at 80 kV. Images were acquired using an 11 megapixel Morada charge-coupled device camera (Morada; Olympus). At least three different lungs per group at ×100,000 magnification were used to assess autophagosomes.
Western Blot
Lung tissue was homogenized in ice-cold RIPA lysate buffer (Applygen Technologies Inc., Beijing, China) according to the manufacturer’s instructions. This was followed by centrifugation at 15,000×g for 15 min at 4 °C. Nuclear protein was extracted with extraction reagents (Applygen Technologies Inc.) and protein was quantified with the BCA method (Applygen Technologies Inc.). Samples (20 μg protein/lane) were separated using 10% SDS-PAGE and then transferred onto PVDF membranes. Membranes were blocked with 5% nonfat milk for 2 h at room temperature and then washed three times in TBST and incubated overnight with rabbit polyclonal antibody against Beclin 1, NFκB (1:1000 dilution, Cell Signaling Technology), β-actin (1:2000 dilution, Cell Signaling Technology), and Lamin B1 (Abcam, Cambridge, MA, USA) at 4 °C overnight. After three washes, membranes were incubated with goat antibody linked to horseradish peroxidase (Cell Signaling, Beverly, MA, USA) for 1 h, and antibody-antigen reactivity was measured with Western blot (Clinx Science Instruments Co., Ltd, China). Band density was quantified with ImageJ software.
STATISTICS
Data were expressed as means ± SD. Statistical analysis was performed with SPSS 17.0 (SPSS Inc., Chicago, IL, USA). Differences between two groups were assessed with a Student’s t test. Post hoc pairwise multiple comparisons were performed using one-way ANOVA followed by a Bonferroni correction (significance was set at P < 0.05).
RESULTS
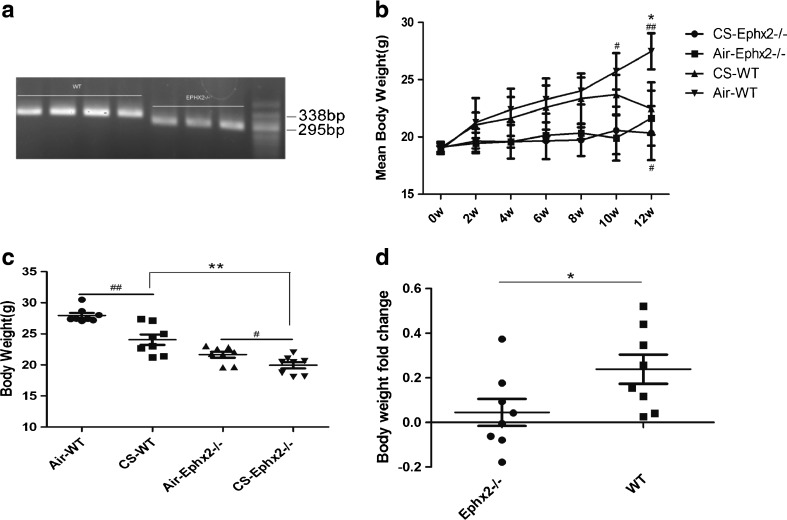
Ephx2−/− Mice Have Fewer Weight Changes After CS Exposure
WT and KO mouse weight was significantly reduced after 12 weeks of cigarette smoke exposure compared to those exposed to air (Fig. 1b). KO mice gained weight more slowly than the WT group in both exposure groups (Fig. 1c). After 12 weeks of cigarette smoke exposure, smoking KO animals weighed less than those in the WT group (Fig. 1b). However, after 12 weeks of treatment, fold-change difference between KO-Con and KO-CS groups was less than that between WT-Con and WT-CS groups (Fig. 1d). It may be that the stable weight observed in Ephx2−/− mice is protective against cigarette smoke exposure.
Fig. 1.
Weight of WT and KO mice changes after exposure to cigarette smoke. a Representative genotype analysis of WT and Ephx2−/− mice. WT type mice produced a gene 338 bp in size and Ephx2−/− mice produced a gene product 295 bp in size. b–d WT mice (n = 20) and Ephx2−/− mice (n = 20) were exposed to air (air-WT, n = 10; air-Ephx2−/−, n = 10) or CS (CS-WT, n = 10; CS-Ephx2−/−, n = 10) for 12 weeks and weight was measured once every 2 weeks. b Weight gain over time. WT weight increased more than in the KO group. c After 12 weeks of treatment, mean weight of mice in the CS-WT group was lower than in the air-WT group and the mean weight of mice in the CS-Ephx2−/− group was lower than that of mice in the air-Ephx2−/−group. d After 12 weeks of treatment, the Ephx2−/− group weight fold-change was less than that of the WT group. Results are expressed as means ± SD. # P < 0.05, significant differences between CS-exposed group and its corresponding air-exposed group; ## P < 0.01, significant differences between CS-exposed group and its corresponding air-exposed group; * P < 0.05, significant differences between CS-exposed WT mice and CS-exposed Ephx2−/− mice, ** P < 0.01, significant differences between CS-exposed WT mice and CS-exposed Ephx2−/− mice.
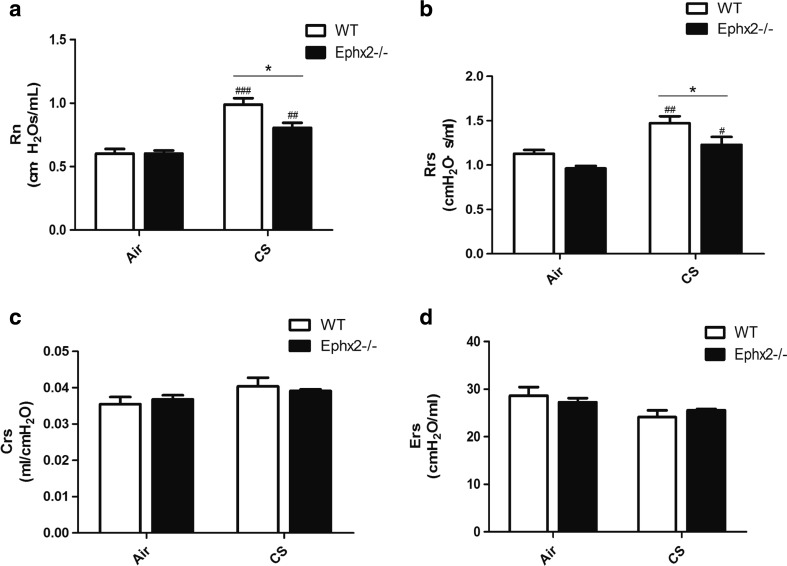
Ephx2−/− Mice Have Less Airway Resistance in Response to CS Exposure
Rn and Rrs of lung function were significantly increased after CS exposure in both WT and Ephx2−/− groups (Fig. 2a, b). Also, Rn and Rrs indices in CS-Ephx2−/− mice were lower than those of CS-WT mice (Fig. 2a, b). These data suggest that lungs of Ephx2−/− mice are less susceptible to CS-induced airway resistance. However, Crs and Ers did not differ in the air-exposed and CS-exposed groups (Fig. 2c, d), perhaps due to insufficient CS exposure time to cause change in Crs and Ers.
Fig. 2.
Ephx2−/− mice have less airway resistance in response to CS exposure. a Rn; b Rrs; c Crs; and d Ers were measured in air- and CS-exposed WT and Ephx2−/− mice, as described. a, b Rn and Rrs increased after 12 weeks of CS exposure in both groups. Rn and Rrs were significantly lower in CS-exposed Ephx2−/− mice. c, d Crs and Ers did not differ between groups with CS exposure. Data are means ± SD (n = 3–4 mice/group). # P < 0.05, significant difference from corresponding air-exposed mice; ## P < 0.01, significant difference from corresponding air-exposed mice; ### P < 0.001, significant difference from corresponding air-exposed mice. * P < 0.05, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/− mice.
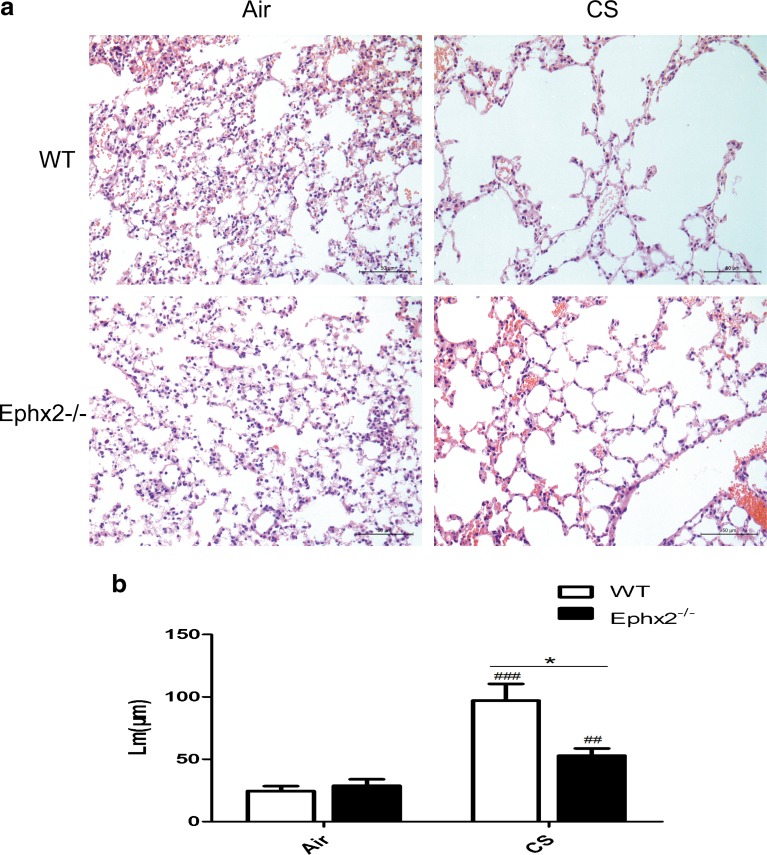
Ephx2−/− Mice Show Attenuated Emphysema in Response to CS
Pulmonary emphysema is a clinical phenotype of COPD, characterized by irreversible enlargement of airspaces distal to the terminal bronchiole and irreversible loss of alveolar structures [41]. Lm was measured to quantify emphysema and CS-exposed WT and CS-exposed Ephx2−/− mice had greater alveolar size compared with corresponding air-exposed mice. Lm of CS-exposed Ephx2−/− mice was significantly lower compared with CS-exposed WT mice (Fig. 3), indicating a partial protection against pulmonary emphysema.
Fig. 3.
There is less air space enlargement in Ephx2−/− mice in response to CS. a Representative H&E stained lung sections exposed to air and CS in WT and Ephx2−/− mice. b Lm was calculated. Original magnification, ×100. Results are expressed as means ± SD (n = 3 mice/group). ## P < 0.01, significant difference from corresponding air-exposed mice; ### P < 0.001, significant difference from corresponding air-exposed mice. * P < 0.05, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/−mice.
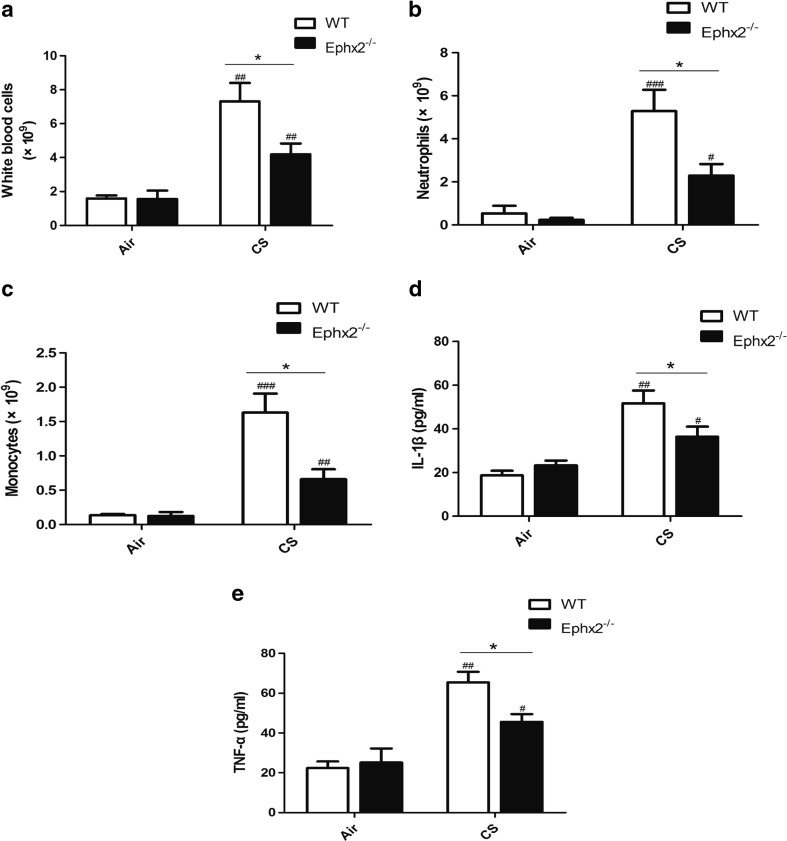
Ephx2−/− Mice Have Less Inflammation in Response to CS
Inflammatory factors, IL-1β, and TNF-α were measured in BALF and these factors were greater after 12 weeks of CS exposure both in WT and Ephx2−/− mice compared with air-exposed mice (Fig. 4a–c). CS-exposed Ephx2−/− mice had less inflammatory cell influx compared with CS-exposed WT mice and CS-exposed WT, and Ephx2−/− mice had more TNF-α and IL-1β in BALF than the air-exposed WT and Ephx2−/− mice (Fig. 4d, e). CS-exposed Ephx2−/− mice had less TNF-α and IL-1β compared with CS-exposed WT mice (Fig. 4d, e). Thus, inflammation is aggravated after 12 weeks of CS exposure and Ephx2−/− mice are protected against this to a degree.
Fig. 4.
Ephx2−/− mice had reduced inflammation in response to CS. After 12 weeks of exposure to air or CS, BALF were obtained and inflammatory cells and TNF-α and IL-1β were quantified. a–c CS-exposed WT mice and CS-exposed Ephx2−/− mice had more leukocytes, neutrophils, and monocytes in BALF than air-exposed mice. CS-exposed Ephx2−/− mice had significantly fewer inflammatory cells in BALF. d, e TNF-α and IL-1β were increased in CS-exposed WT and CS-exposed Ephx2−/− mice than with air-exposed WT and air-exposed Ephx2−/− mice. CS-exposed Ephx2−/− mice had significantly lower TNF-α and IL-1β than CS-exposed WT mice. Results are expressed as means ± SD (n = 4 mice/group). # P < 0.05, significant difference from corresponding air-exposed mice; ## P < 0.01, significant difference from corresponding air-exposed mice; ### P < 0.001, significant difference from corresponding air-exposed mice; * P < 0.05, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/− mice.
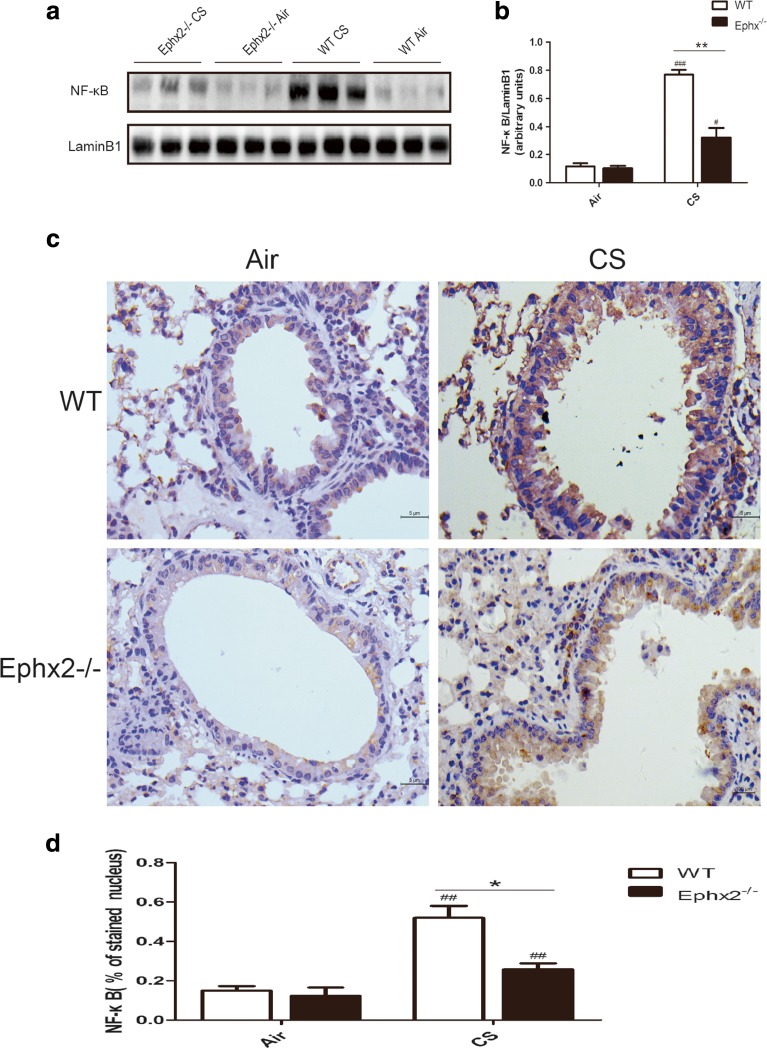
Ephx2−/− Mice Have Reduced NF-κB Expression in Response to CS
NF-κB was measured and was observed to be greater in CS-exposed WT mice and CS-exposed Ephx2−/− mice compared to air-exposed mice (Fig. 5a, b). Ephx2−/− mice had reduced NF-κB expression compared to WT mice in response to CS (Fig. 5a, b). Immunohistochemical data were consistent with blot data (Fig. 5c, d) and blot and immunohistochemistry results were consistent with findings of greater inflammatory factors and cells in BALF (Fig. 4). Thus, Ephx2 deficiency may increase resistance to inflammation via the NF-κB pathway.
Fig. 5.
Nuclear factor NF-κB is expressed in the lungs in response to CS. NF-κB expression was measured after 12 weeks of exposure to air or CS. a Western blot for NF-κB expression in lung tissue. b Relative intensity of NF-κB calculated by densitometry. Results represent means ± SD from at least three independent experiments. c NF-κB expression in lung alveolar/airway epithelial cells from each group via immunohistochemistry (n = 3 mice/group). Inverted phase contrast microscopy revealing dark brown staining representing NF-κB expression (×400). d Graph is IntDen of NF-κB. # P < 0.05, significant difference from corresponding air-exposed mice; ## P < 0.01, significant difference from corresponding air-exposed mice; ### P < 0.001, significant difference from corresponding air-exposed mice; * P < 0.05, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/− mice; ** P < 0.01, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/− mice.
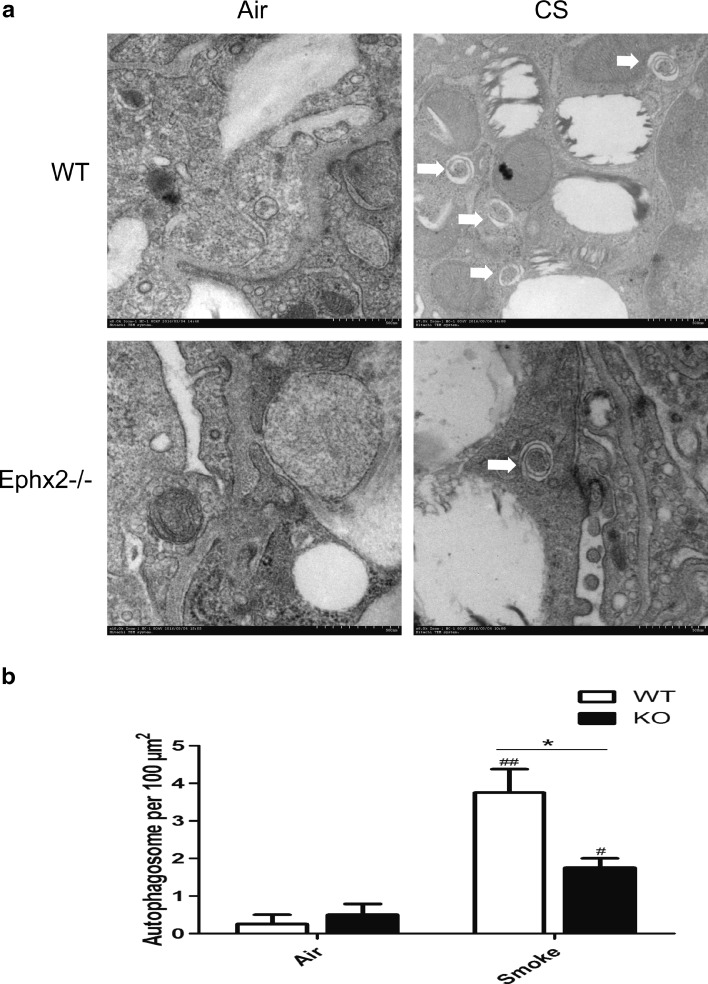
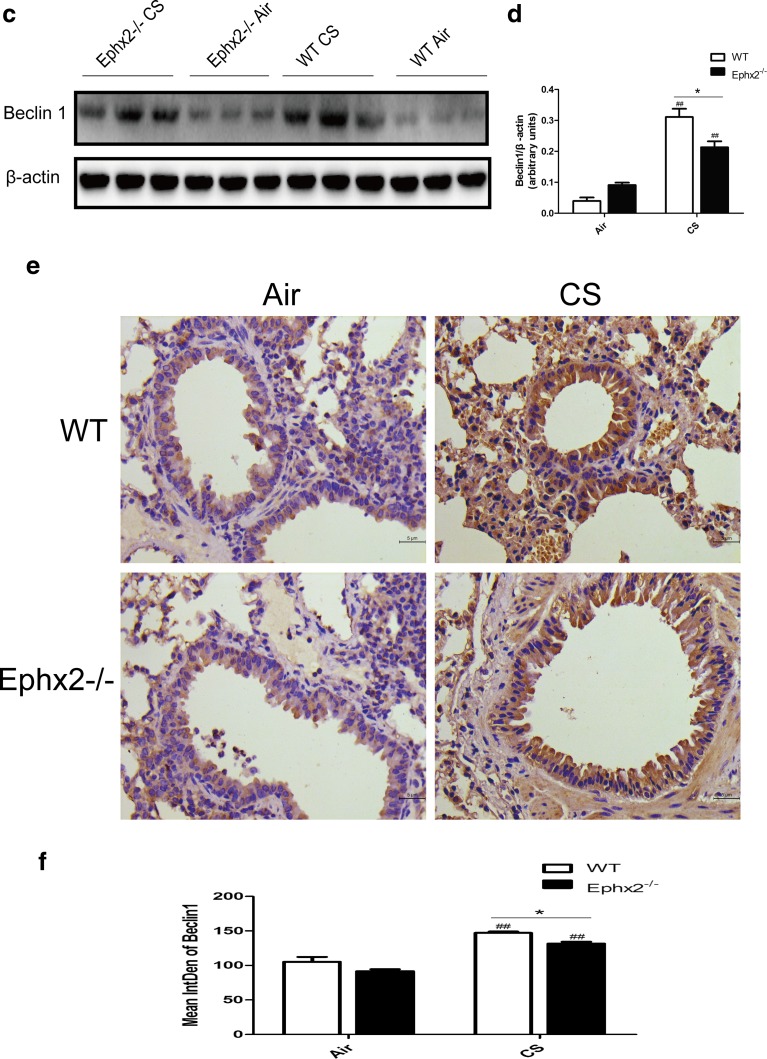
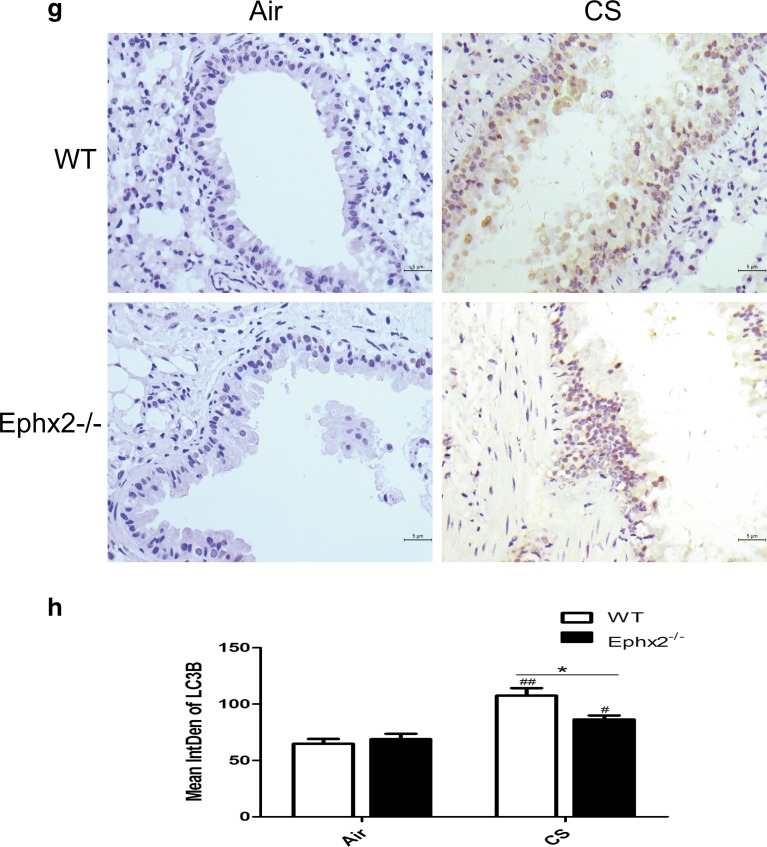
Ephx2−/− Mice Have Reduced Autophagy in Response to CS
Autophagy contributes to COPD [3] and may interact with EETs [19, 35]. For this reason, autophagy was measured in each mouse group (Fig. 6a). Data show that autophagosomes increased in CS-exposed WT and CS-exposed Ephx2−/− mice compared to air-exposed animals. CS-exposed Ephx2−/− mice had fewer autophagosomes than CS-exposed WT mice (Fig. 6a, b). In this way, CS can induce autophagy in a COPD mouse model and Ephx2−/− mice may be less susceptible to autophagy. Data also show that Beclin 1 and LC3B (Fig. 6c, e, g) were significantly higher in CS-exposed WT and CS-exposed Ephx2−/− mice than in air-exposed mice and that CS-exposed Ephx2−/− mice had less Beclin 1 and LC3B expression compared to CS-exposed WT.
Fig. 6.
Ephx2−/− mice had less autophagy in response to CS-WT and Ephx2−/− mice were exposed to air or CS for 12 weeks and autophagy protein LC3B and Beclin 1 expression was measured. a Autophagosomes under electron microscopy (×100,000); white arrows depict autophagosomes (n = 3 mice/group). b EM images scored autophagosomes. Data are expressed as AVs/100 μm2 (N = 10 images representative of each group). c Western blot of Beclin 1. d Relative intensity of Beclin 1 was calculated by densitometry and values are presented as means ± SD. e–h Representative immunohistochemical images for Beclin 1 (e) and LC3B (g) in mouse lung tissues (n = 3 mice/group). f, h Graph represents IntDen of Beclin 1 and LC3B and values are presented as means ± SD. # P < 0.05, significant difference from corresponding air-exposed mice; ## P < 0.01, significant difference from corresponding air-exposed mice. * P < 0.05, significant difference between CS-exposed WT mice and CS-exposed Ephx2−/− mice.
DISCUSSION
COPD is mainly caused by cigarette smoking, and it is characterized by emphysema, pulmonary inflammation, fibrogenesis, and reduced lung function [31]. Increased autophagy is also observed in lungs of mice exposed to chronic CS [3]. The greatest amount of airway inflammation was observed in mice after 12 weeks of CS exposure, and WT and Ephx2−/− mice both had aggravated emphysema, increased airway resistance, and inflammation and autophagy compared to air-exposed animals, but Ephx2−/− mice had fewer of these symptoms than WT mice and they had reduced autophagy. In this way, Ephx2 deficiency may protect individuals from CS-induced lung disease.
CYP-mediated arachidonic acid metabolism is an important regulator of inflammation and EETs, whose CYP epoxygenase-derived products are proposed to be anti-inflammatory mediators in vascular, liver, and renal diseases [29]. EETs are hydrolyzed by sEH, which is encoded by Ephx2−/− gene [28], to DHETs, which has a less important biological function. Inhibitors targeting sEH-induced increasing endogenous EETs can be antihypertensive and anti-inflammatory as well as protective to the brain, heart, and kidneys [11, 24]. Recently, EETs and sEH inhibitors have been shown to have an anti-inflammatory effect in lung disease. Morin’s group reported that 14, 15-EET has anti-inflammatory effects on human bronchi treated with TNF-α [23]. Ma and colleagues reported that 11, 12-EET and 14, 15-EET can reduce CS extraction-induced release of IL-8 in human bronchial epithelial cells [20]. Podolin’s group demonstrated that a sEH inhibitor reduces CS-induced pulmonary inflammation by inhibiting its initiation and promoting its resolution [32]. Recently, an initial report indicated that inhibition of sEH downregulates the inflammatory response induced by acute or sub-chronic tobacco smoke exposure, which was consistent with data from Ephx2−/− knockout mice [30]. This was the first report to describe chronic CS-induced inflammatory response in an Ephx2−/− knockout mice model. Current data showed that 12 weeks of CS exposure elevated inflammatory cells in BALF of WT and Ephx2−/− mice but that, Ephx2−/− mice had less inflammatory cell influx than WT mice. TNF-α and IL-1β displayed the same trend. NF-κB expression was noted to be elevated in CS-exposed WT and Ephx2−/− mice, and Ephx2−/− mice had less NF-κB than WT mice. Immunohistochemistry and blot data were consistent with these findings.
EETs are reported to inhibit the NF-κB signaling pathway, and subsequently inhibit expression of vascular cell adhesion molecule-1 (VCAM-1), attenuating leukocyte migration [29]. Nording’s group reported that 8, 9-EET/DHET and 14, 15-EET/DHET ratios in plasma were more elevated in Ephx2−/− mice subjected to after acute and sub-chronic CS exposure than in WT mice, suggesting an anti-inflammatory property of Ephx2 deficiency [30]. In this way, Ephx2 deficiency may lead to increased EETs/DHET ratios which may block the NF-κB signaling pathway and protect against chronic CS-induced lung inflammation. The manner by which this occurs is uncertain.
In this way, Ephx2−/− mice are less susceptible to CS-induced emphysema and airway resistance and air space enlargement is greater in WT and Ephx2−/− mice in response to CS exposure but comparatively less in CS-exposed Ephx2−/− mice. Pulmonary emphysema occurs in COPD and is characterized by irreversible enlargement of airspaces distal to the terminal bronchiole and irreversible loss of alveolar structures [41]. Previous reports have suggested that infiltration of neutrophils and macrophages with release of proteolytic enzymes in response to CS contributes to lung tissue destruction in mouse emphysema models [7, 10, 38]. Apoptosis triggered by oxidative stress can also contribute to pathogenesis of CS-induced emphysema [14].
Ephx2−/− mice have reduced inflammation and EETs have a role in an anti-apoptotic CS-induced human bronchial epithelial cell line. In this way, the mechanism of repair of tissue in Ephx2−/− mice with emphysema may depend on EET properties. COPD features elevation of respiratory resistance and reduced compliance [2, 43]. Yang’s group reported that respiratory system resistance indices were elevated after 10 or 12 months of tobacco inhalation [45]. This is consistent with the current observations. After 12 weeks of CS exposure, Rn and Rrs increased in both exposed animal groups even though Ephx2−/− mice had normal Rn and Rrs levels and WT mice did not. This may be partly due to the lower concentrations of fewer inflammatory cells and inflammatory factors. There was no significant difference between the CS-exposed group and the air-exposed group with respect to Crs or Ers likely because 12 weeks is not sufficient for these to change appreciably. Ephx2−/− mice gained less weight than WT but why this is so is unclear.
Ephx2 deficiency inhibits autophagy in a CS-exposed COPD mouse model. Data showed there to be more autophagosomes in lung tissues of CS-exposed WT mice and CS-exposed Ephx2−/− mice than in animals exposed to air, and CS-exposed Ephx2−/− mice had fewer autophagosomes than WT mice. In this way, autophagy was enhanced in a COPD mouse model and Ephx2 deficiency inhibited autophagy. Beclin 1 and LC3B data are consistent with these trends. Chen’s group reported for the first time that increased autophagy is associated with CS-induced COPD [3], and autophagy was induced in the current COPD model. An and colleagues reported that TLR4 exerts a protective role in CS-induced emphysema development by reducing the autophagic pathway [1]. Ji’s group reported that Vam3 decreases CS-induced autophagy and inhibits oxidative stress. Stefan and colleagues proposed that autophagy has an effect on the stress response to CS exposure in vitro and may contribute to the etiology of COPD [34]. Two reports have described EETs and heart and liver protection via autophagy regulation [19, 35]. In this way, Ephx2−/− mice may have protection against CS-induced lung inflammation and this likely takes place through reduced autophagy but EETs and autophagy interactions require elucidation to confirm these assertions. In addition to the protective role of autophagy suppression we proved, autophagy is a double-edge sword and it has a complex cross-talk with apoptosis [33]. Autophagy primarily plays a protective role that may prevent cell death and it has been demonstrated that autophagy plays a critical role in maintaining cellular homeostasis and the adaption to environmental stress (oxidative stress, starvation, hypoxia, etc.) [13–15, 22]. However, it has been proved that both excessive and impaired autophagy can cause cell death in some model systems due to the interaction with apoptosis [33]. Deficiency of LC3B and Beclin 1 inhibits cell death induced by CSE in pulmonary epithelial cells and the airspace enlargement and apoptosis after cigarette smoke exposure are inhibited in LC3B-deficient mice [3, 4, 14]. Further studies are required to elucidate the role of autophagy in COPD. In conclusion, we used mouse model with a deficiency in Ephx2 to explore the effect of this gene on chronic CS-induced COPD. Mice lacking this gene had less lung inflammation and reduced emphysema and airway resistance. Also, the gene may contribute to less autophagy. In this way, this may represent a novel therapeutic target for the treatment of COPD.
ACKNOWLEDGEMENTS
This work was supported by Beijing Municipal Natural Science Foundation (7142046, 7164250) and grant Shou Fa 2011-2002-03 from the Beijing Municipal Health Bureau. We would like to thank professor Yi Zhu who is from Tianjing Medical University for providing us the EPHX2-/- mice. We would like to thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Footnotes
Qi Hou and Bo Xu contributed equally to this work.
REFERENCES
- 1.An CH, Wang XM, Lam HC, Ifedigbo E, Washko GR, Ryter SW, Choi AM. TLR4 deficiency promotes autophagy during cigarette smoke-induced pulmonary emphysema. American Journal of Physiology Lung Cellular and Molecular Physiology. 2012;303(9):L748–757. doi: 10.1152/ajplung.00102.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown RH, Walters DM, Greenberg RS, Mitzner W. A method of endotracheal intubation and pulmonary functional assessment for repeated studies in mice. Journal of Applied Physiology (1985) 1999;87(6):2362–2365. doi: 10.1152/jappl.1999.87.6.2362. [DOI] [PubMed] [Google Scholar]
- 3.Chen ZH, Kim HP, Sciurba FC, Lee SJ, Feghali-Bostwick C, Stolz DB, Dhir R, et al. Egr-1 regulates autophagy in cigarette smoke-induced chronic obstructive pulmonary disease. PLoS One. 2008;3(10) doi: 10.1371/journal.pone.0003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen ZH, Lam HC, Jin Y, Kim HP, Cao J, Lee SJ, Ifedigbo E, Parameswaran H, Ryter SW, Choi AM. Autophagy protein microtubule-associated protein 1 light chain-3B (LC3B) activates extrinsic apoptosis during cigarette smoke-induced emphysema. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(44):18880–18885. doi: 10.1073/pnas.1005574107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowburn AS, Condliffe AM, Farahi N, Summers C, Chilvers ER. Advances in neutrophil biology: clinical implications. Chest. 2008;134(3):606–612. doi: 10.1378/chest.08-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng Y, Theken KN, Lee CR. Cytochrome P450 epoxygenases, soluble epoxide hydrolase, and the regulation of cardiovascular inflammation. Journal of Molecular and Cellular Cardiology. 2010;48(2):331–341. doi: 10.1016/j.yjmcc.2009.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhami R, Gilks B, Xie C, Zay K, Wright JL, Churg A. Acute cigarette smoke-induced connective tissue breakdown is mediated by neutrophils and prevented by alpha1-antitrypsin. American Journal of Respiratory Cell and Molecular Biology. 2000;22(2):244–252. doi: 10.1165/ajrcmb.22.2.3809. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein R, Fraser RS, Ghezzo H, Cosio MG. Alveolar inflammation and its relation to emphysema in smokers. American Journal of Respiratory and Critical Care Medicine. 1995;152(5 Pt 1):1666–1672. doi: 10.1164/ajrccm.152.5.7582312. [DOI] [PubMed] [Google Scholar]
- 9.Fleming I, Michaelis UR, Bredenkotter D, Fisslthaler B, Dehghani F, Brandes RP, Busse R. Endothelium-derived hyperpolarizing factor synthase (Cytochrome P450 2C9) is a functionally significant source of reactive oxygen species in coronary arteries. Circulation Research. 2001;88(1):44–51. doi: 10.1161/01.RES.88.1.44. [DOI] [PubMed] [Google Scholar]
- 10.Hautamaki RD, Kobayashi DK, Senior RM, Shapiro SD. Requirement for macrophage elastase for cigarette smoke-induced emphysema in mice. Science. 1997;277(5334):2002–2004. doi: 10.1126/science.277.5334.2002. [DOI] [PubMed] [Google Scholar]
- 11.Imig JD, Hammock BD. Soluble epoxide hydrolase as a therapeutic target for cardiovascular diseases. Nature Reviews Drug Discovery. 2009;8(10):794–805. doi: 10.1038/nrd2875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaspera R, Totah RA. Epoxyeicosatrienoic acids: formation, metabolism and potential role in tissue physiology and pathophysiology. Expert Opinion on Drug Metabolism & Toxicology. 2009;5(7):757–771. doi: 10.1517/17425250902932923. [DOI] [PubMed] [Google Scholar]
- 13.Kiffin R, Bandyopadhyay U, Cuervo AM. Oxidative stress and autophagy. Antioxidants and Redox Signaling. 2006;8(1–2):152–162. doi: 10.1089/ars.2006.8.152. [DOI] [PubMed] [Google Scholar]
- 14.Kim HP, Wang X, Chen ZH, Lee SJ, Huang MH, Wang Y, Ryter SW, Choi AM. Autophagic proteins regulate cigarette smoke-induced apoptosis: protective role of heme oxygenase-1. Autophagy. 2008;4(7):887–895. doi: 10.4161/auto.6767. [DOI] [PubMed] [Google Scholar]
- 15.Kondo Y, Kanzawa T, Sawaya R, Kondo S. The role of autophagy in cancer development and response to therapy. Nature Reviews Cancer. 2005;5(9):726–734. doi: 10.1038/nrc1692. [DOI] [PubMed] [Google Scholar]
- 16.Lacoste JY, Bousquet J, Chanez P, Van Vyve T, Simony-Lafontaine J, Lequeu N, Vic P, Enander I, Godard P, Michel FB. Eosinophilic and neutrophilic inflammation in asthma, chronic bronchitis, and chronic obstructive pulmonary disease. The Journal of Allergy and Clinical Immunology. 1993;92(4):537–548. doi: 10.1016/0091-6749(93)90078-T. [DOI] [PubMed] [Google Scholar]
- 17.Levine B, Klionsky DJ. Development by self-digestion: molecular mechanisms and biological functions of autophagy. Developmental Cell. 2004;6(4):463–477. doi: 10.1016/S1534-5807(04)00099-1. [DOI] [PubMed] [Google Scholar]
- 18.Levine B, Yuan J. Autophagy in cell death: an innocent convict? Journal of Clinical Investigation. 2005;115(10):2679–2688. doi: 10.1172/JCI26390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez-Vicario C, Alcaraz-Quiles J, Garcia-Alonso V, Rius B, Hwang SH, Titos E, Lopategi A, Hammock BD, Arroyo V, Claria J. Inhibition of soluble epoxide hydrolase modulates inflammation and autophagy in obese adipose tissue and liver: role for omega-3 epoxides. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(2):536–541. doi: 10.1073/pnas.1422590112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma WJ, Sun YH, Jiang JX, Dong XW, Zhou JY, Xie QM. Epoxyeicosatrienoic acids attenuate cigarette smoke extract-induced interleukin-8 production in bronchial epithelial cells. Prostaglandins, Leukotrienes, and Essential Fatty Acids. 2015;94:13–19. doi: 10.1016/j.plefa.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Maiuri MC, Zalckvar E, Kimchi A, Kroemer G. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nature Reviews Molecular Cell Biology. 2007;8(9):741–752. doi: 10.1038/nrm2239. [DOI] [PubMed] [Google Scholar]
- 22.Mizushima N, Levine B, Cuervo AM, Klionsky DJ. Autophagy fights disease through cellular self-digestion. Nature. 2008;451(7182):1069–1075. doi: 10.1038/nature06639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morin C, Sirois M, Echave V, Gomes MM, Rousseau E. EET displays anti-inflammatory effects in TNF-alpha stimulated human bronchi: putative role of CPI-17. American Journal of Respiratory Cell and Molecular Biology. 2008;38(2):192–201. doi: 10.1165/rcmb.2007-0232OC. [DOI] [PubMed] [Google Scholar]
- 24.Morisseau C, Hammock BD. Impact of soluble epoxide hydrolase and epoxyeicosanoids on human health. Annual Review of Pharmacology and Toxicology. 2013;53:37–58. doi: 10.1146/annurev-pharmtox-011112-140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morse D, Rosas IO. Tobacco smoke-induced lung fibrosis and emphysema. Annual Review of Physiology. 2014;76:493–513. doi: 10.1146/annurev-physiol-021113-170411. [DOI] [PubMed] [Google Scholar]
- 26.Nakahira K, Choi AM. Autophagy: a potential therapeutic target in lung diseases. American Journal of Physiology - Lung Cellular and Molecular Physiology. 2013;305(2):L93–107. doi: 10.1152/ajplung.00072.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakahira K, Cloonan SM, Mizumura K, Choi AM, Ryter SW. Autophagy: a crucial moderator of redox balance, inflammation, and apoptosis in lung disease. Antioxidants and Redox Signaling. 2014;20(3):474–494. doi: 10.1089/ars.2013.5373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newman JW, Morisseau C, Hammock BD. Epoxide hydrolases: their roles and interactions with lipid metabolism. Progress in Lipid Research. 2005;44(1):1–51. doi: 10.1016/j.plipres.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Node K, Huo Y, Ruan X, Yang B, Spiecker M, Ley K, Zeldin DC, Liao JK. Anti-inflammatory properties of cytochrome P450 epoxygenase-derived eicosanoids. Science. 1999;285(5431):1276–1279. doi: 10.1126/science.285.5431.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nording ML, Yang J, Hoang L, Zamora V, Uyeminami D, Espiritu I, Pinkerton KE, Hammock BD, Luria A. Bioactive lipid profiling reveals drug target engagement of a soluble epoxide hydrolase inhibitor in a murine model of tobacco smoke exposure. Journal of Meteorology. 2015 doi: 10.7243/2059-0008-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. American Journal of Respiratory and Critical Care Medicine. 2001;163(5):1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 32.Podolin PL, Bolognese BJ, Foley JF, Long E, 3rd, Peck B, Umbrecht S, Zhang X, et al. In vitro and in vivo characterization of a novel soluble epoxide hydrolase inhibitor. Prostaglandins & Other Lipid Mediators. 2013;104–105:25–31. doi: 10.1016/j.prostaglandins.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Ravikumar B, Sarkar S, Davies JE, Futter M, Garcia-Arencibia M, Green-Thompson ZW, Jimenez-Sanchez M, et al. Regulation of mammalian autophagy in physiology and pathophysiology. Physiological Reviews. 2010;90(4):1383–1435. doi: 10.1152/physrev.00030.2009. [DOI] [PubMed] [Google Scholar]
- 34.Ryter SW, Chen ZH, Kim HP, Choi AM. Autophagy in chronic obstructive pulmonary disease: homeostatic or pathogenic mechanism? Autophagy. 2009;5(2):235–237. doi: 10.4161/auto.5.2.7495. [DOI] [PubMed] [Google Scholar]
- 35.Samokhvalov V, Alsaleh N, El-Sikhry HE, Jamieson KL, Chen CB, Lopaschuk DG, Carter C, et al. Epoxyeicosatrienoic acids protect cardiac cells during starvation by modulating an autophagic response. Cell Death & Disease. 2013;4 doi: 10.1038/cddis.2013.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scrivo R, Vasile M, Bartosiewicz I, Valesini G. Inflammation as “common soil” of the multifactorial diseases. Autoimmunity Reviews. 2011;10(7):369–374. doi: 10.1016/j.autrev.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Shapiro SD. The macrophage in chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1999;160(5 Pt 2):S29–32. doi: 10.1164/ajrccm.160.supplement_1.9. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro SD, Goldstein NM, Houghton AM, Kobayashi DK, Kelley D, Belaaouaj A. Neutrophil elastase contributes to cigarette smoke-induced emphysema in mice. The American Journal of Pathology. 2003;163(6):2329–2335. doi: 10.1016/S0002-9440(10)63589-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sinal CJ, Miyata M, Tohkin M, Nagata K, Bend JR, Gonzalez FJ. Targeted disruption of soluble epoxide hydrolase reveals a role in blood pressure regulation. Journal of Biological Chemistry. 2000;275(51):40504–40510. doi: 10.1074/jbc.M008106200. [DOI] [PubMed] [Google Scholar]
- 40.Soler P, Moreau A, Basset F, Hance AJ. Cigarette smoking-induced changes in the number and differentiated state of pulmonary dendritic cells/Langerhans cells. American Review of Respiratory Disease. 1989;139(5):1112–1117. doi: 10.1164/ajrccm/139.5.1112. [DOI] [PubMed] [Google Scholar]
- 41.Surolia R, Karki S, Kim H, Yu Z, Kulkarni T, Mirov SB, Carter AB, et al. Heme oxygenase-1-mediated autophagy protects against pulmonary endothelial cell death and development of emphysema in cadmium-treated mice. American Journal of Physiology - Lung Cellular and Molecular Physiology. 2015;309(3):L280–292. doi: 10.1152/ajplung.00097.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tuder RM, Yun JH. It takes two to tango: cigarette smoke partners with viruses to promote emphysema. Journal of Clinical Investigation. 2008;118(8):2689–2693. doi: 10.1172/JCI36536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wright JL, Sun JP, Vedal S. A longitudinal analysis of pulmonary function in rats during a 12 month cigarette smoke exposure. European Respiratory Journal. 1997;10(5):1115–1119. doi: 10.1183/09031936.97.10051115. [DOI] [PubMed] [Google Scholar]
- 44.Xu F, Yin X, Zhang M, Shen H, Lu L, Xu Y. Prevalence of physician-diagnosed COPD and its association with smoking among urban and rural residents in regional mainland China. Chest. 2005;128(4):2818–2823. doi: 10.1378/chest.128.4.2818. [DOI] [PubMed] [Google Scholar]
- 45.Yang W, Ni H, Wang H, Gu H. NLRP3 inflammasome is essential for the development of chronic obstructive pulmonary disease. International Journal of Clinical and Experimental Pathology. 2015;8(10):13209–13216. [PMC free article] [PubMed] [Google Scholar]
- 46.Zeldin DC. Epoxygenase pathways of arachidonic acid metabolism. Journal of Biological Chemistry. 2001;276(39):36059–36062. doi: 10.1074/jbc.R100030200. [DOI] [PubMed] [Google Scholar]
- 47.Zeldin DC, Plitman JD, Kobayashi J, Miller RF, Snapper JR, Falck JR, Szarek JL, Philpot RM, Capdevila JH. The rabbit pulmonary cytochrome P450 arachidonic acid metabolic pathway: characterization and significance. Journal of Clinical Investigation. 1995;95(5):2150–2160. doi: 10.1172/JCI117904. [DOI] [PMC free article] [PubMed] [Google Scholar]