Abstract
Numerous laboratory studies involving both animal and human models indicate that weight loss induces changes in leptin, ghrelin and insulin sensitivity, which work to promote weight regain. It is unclear, however, whether these biological changes serve as a biomarker for predicting weight regain in free-living humans in which biological, behavioral and environmental factors are likely at play. We identified 12 studies published between January 1995 and December 2011 that reported changes in leptin, ghrelin or insulin during intentional weight loss with a follow-up period to assess regain. Two of the nine studies examining leptin suggested that larger decreases were associated with greater regain, three studies found the opposite (smaller decreases were associated with greater regain), whereas four studies found no significant relationship; none of the studies supported the hypothesis that increases in ghrelin during weight loss were associated with regain. One study suggested that improvements in insulin resistance were associated with weight gain, but five subsequent studies reported no association. Changes in leptin, ghrelin or insulin sensitivity, taken alone, are not sufficient to predict weight regain following weight loss in free-living humans. In future studies, it is important to include a combination of physiological, behavioral and environmental variables in order to identify subgroups at greatest risk of weight regain.
Keywords: weight loss, weight regain, appetite hormones, review, free-living humans
INTRODUCTION
Sixty-eight percent of men and women in the United States are classified as overweight (body mass index ≥25 kgm−2) or obese (body mass index ≥30 kgm−2).1 By promoting dyslipidemia, insulin resistance and systemic inflammation, excess adiposity increases risk for poorer health outcomes including cardiovascular disease or type 2 diabetes.2,3 Moderate, but clinically significant weight losses of ~5–10% have been shown to reduce disease risk.4,5 Although weight loss is achievable through a variety of programs (self-guided, commercial, behavioral or medically supervised), weight regain is common.6–9
Weight loss-induced adaptations in several humoral factors have been identified and substantial laboratory-based evidence supports that such adaptations promote weight regain. In rodent models of diet-induced obesity, weight loss triggers biological and metabolic adaptations that contribute to overfeeding and subsequent weight regain.10–12 In humans, fasting concentrations of adiposity signals leptin and insulin, which are elevated with excessive adiposity, are substantially reduced during caloric restriction and subsequent weight loss.13–26 Importantly, these reductions are disproportionately low relative to observed fat mass at a stabilized weight,12,24,27–29 which is likely interpreted by the central nervous system as a considerable energy depletion that must be corrected.30 Indeed, maintenance of a reduced body weight has been related to leptin-reversible neural activity in part of the brain responsible for energy homeostasis,31 and leptin administration in weight-reduced subjects improves satiety.32 In addition, caloric restriction and weight loss induce significant increases in the concentration of ghrelin,33–35 a potent orexigenic hormone.36,37 Elevations in ghrelin concentration, either endogenous38 or exogenous,39 are associated with feelings of hunger and increased food intake.
Given the substantial evidence that biological adaptations occur with weight loss in a manner that promotes overfeeding and weight regain in tightly controlled laboratory studies, it is important to determine whether any of the commonly measured biomarkers (leptin, insulin or ghrelin) are predictive of weight regain in free-living humans, in which non-homeostatic behavioral and environmental factors are also at play. Such a biomarker could have significant value in determining individual risk of weight regain in a clinical setting and in subsequently tailoring treatment programs to improve weight maintenance outcomes in previously overweight or obese individuals. Furthermore, determining a predictive biomarker could advance pharmacological prevention of weight regain. Therefore, the aim of the present review was to determine whether weight loss-induced changes in leptin, insulin or ghrelin have been demonstrated to predict human weight regain in the prior literature.
MATERIALS AND METHODS
Search strategies
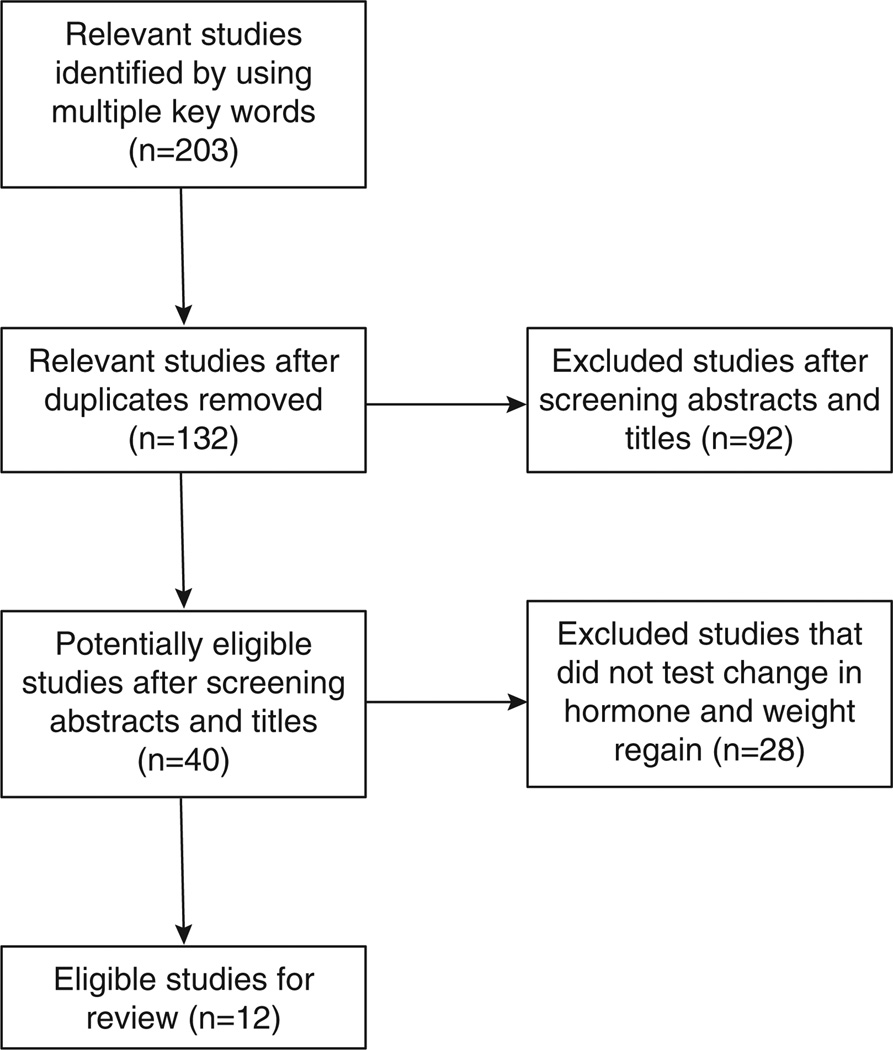
A systematic search was conducted through the PubMed electronic database. The database was searched for human studies from January 1990 to January 2012. The inclusion criteria were that studies (i) reported intentional weight loss with a follow-up period to assess weight regain, (ii) were published in English or with an English abstract, (iii) reported original research on the relationships between weight loss-induced changes in leptin, ghrelin and indices of insulin sensitivity (glucose clamp, fasting insulin, and so on) and weight regain or weight maintenance. Multiple keywords and word combinations were used in searches, including weight, regain, maintenance, leptin, ghrelin, insulin, insulin sensitivity, predict, future and weight change. The references of articles were also screened for potentially relevant studies. The study selection process is shown in Figure 1.
Figure 1.
Study inclusion. This flow chart illustrates the process including relevant studies for the current review.
Data synthesis
The studies’ diversity in sample, design, data analysis, variables and follow-up time-frame (3 months–4 years after weight loss) precluded meta-analysis. The data are summarized descriptively and synthesized in Tables 1–3. The tables are organized by author group and publication year from earliest to most recent, and then alphabetically. They include descriptions of the sample populations if available (age and body mass index upon entry to study and gender stratification) and descriptions of the intervention (approach to weight loss and durations of weight loss/maintenance phases). Initial weight loss is described referring to weight change during the initial weight loss phase compared with baseline. Follow-up weight loss is also described referring to weight change during the maintenance phase compared with baseline. If quantitative data for follow-up weights were not provided, the tables provide descriptive information on weight change patterns stratified by successful maintenance or quartiles. Finally, tables provide determinations (‘yes’, ‘no’ or ‘not tested’) on the basis of study outcomes of whether decreases in leptin, increases in ghrelin or increases in insulin sensitivity during weight loss were related to weight regain. Within the reviewed studies, we also determined whether low leptin, high ghrelin or high insulin sensitivity at baseline or post-weight loss were associated with weight regain. These data are also available on the provided tables.
Table 1.
Studies of leptin changes during weight loss and weight regain
| Author group and year of publication (citation) |
Sample description | Intervention | Initial weight loss and follow- up status |
Do decreases in leptin predict regain | Does low baseline leptin predict regain |
Does low end point leptin predict regain |
|---|---|---|---|---|---|---|
| Wing et al.45 | Subjects 52 Women Age (years) 41.6 ± 8.0 BMI (kg/m2) 31.1 ± 3.7 |
Approach Behavioral intervention with restricted diet (1000–1500 kcal per day) Weight loss-phase 4 months Maintenance phase 6 months |
Initial − 8.1 ± 3.6 kg Follow-up − 7.2 ± 6.3 kg |
No Declines in fasting leptin during weight loss not associated with weight regain (r = 0.19, P>0.05). (Analysis controlled for change in body weight during weight loss) |
No Baseline leptin was not associated with weight regain (P>0.05) |
NT |
| Torgerson et al.42 | Subjects 69 (65% Women) Age (years) M: 44.0 ± 11.9 W: 44.1 ± 11.2 BMI (kg/m2) M: 39.1 ± 4.5 W: 37.8 ± 3.3 |
Approach Very low-calorie diet (450 kcal per day) Weight-loss phase 16 weeks Maintenance phase 32 weeks |
Initial M: − 20.3 ± 6.7% W: − 15.6 ± 6.9% Follow-up M: − 14.4 ± 7.5% W: − 11.8 ± 8.4% |
No Smaller declines in leptin were associated with weight regain (T-ratio = 6.56, P<0.001) |
No High baseline leptin associated with weight regain (T-ratio = 4.70, P<0.001) |
NT |
| Mavri et al.44 | Subjects 30 Women Age (years) 40 BMI (kg/m2) 30.6 ± 5.0 |
Approach Hypocaloric diet (800–1200 kcal per day Weight–loss phase 3 months Maintenance phase 5 months |
Initial − 16 ± 6% body weight Follow-up 12 regaineda, 18 maintainedb |
No Declines in fasting leptin during weight loss larger (− 60%, P<0.01) in those who subsequently maintained weight loss compared with those who regained (− 22%, P = 0.07) |
Yes Lower baseline leptin found in those who subsequently regained compared with those who maintained weight loss (P = 0.04) |
NT |
| Vogels and Westerterp- Plantenga46 |
Subjects 103 Age (years) 48 ± 9.5 BMI (kg/m2) 31.1 ± 3.7 |
Approach Very low-calorie diet (500 kcal per day) Weight-loss phase 6 weeks Maintenance phase 22.5 months |
Initial − 7.2 ± 3.1 kg Follow-up 90 regainedc, 13 maintainedd |
No Declines in fasting leptin during weight loss similar between regainers (− 68%) and maintainers (− 57%) (not tested statistically) |
No Baseline leptin not different between maintainers and regainers (P>0.05) |
NT |
| Crujeiras et al.43 | Subjects 104 (47% Women) Age (years) 35 ± 6 BMI (kg/m2) 31.1 ± 2.9 |
Approach Hypocaloric diet (30% kcal restriction) Weight-loss phase 8 weeks Maintenance phase 6 months |
Initial − 5.0 ± 2.2% body weight Follow-up − 5.68% body weight |
No Smaller declines in leptin during weight loss associated with weight regain (r = 0.30, P = 0.005; OR = 0.141, P = 0.001) (Analysis controlled for change in body weight during weight loss) |
No High baseline leptin associated with weight regain (r = 0.25, P = 0.021) |
NO High post-weight loss leptin associated with weight regain (r = 0.26, P = 0.014) |
| Erez et al.40 | Subjects 272 (14% Women) Age (years) 51.2 ± 6.4 BMI (kg/m2) 30.9 ± 3.6 |
Approach Restricted low-fat or Mediterranean diets (1500–1800 kcal per day) or non-restricted low carbohydrate Weight-loss phase 6 months Maintenance phase 18 months |
Initial − 6.1 ± 5.4% body weight Follow-up − 4.7 ± 5.7% body weight |
Yes Larger declines in fasting leptin during weight loss predicts weight regain (β = − 0.131, P = 0.013) (analysis controlled for change in body weight during weight loss) |
NT | NT |
| Soni et al.41 | Subjects 200 Women Age (years) 57.1 ± 2.9 years BMI (kg/m2) 30.3 ± 3.7 |
Approach Lifestyle intervention with restricted low-fat diet (1300–1500 kcal per day) Weight-loss phase 18 months Maintenance phase 12 months |
Initial − 10.5 lbs (range: + 18 to − 77.5 lbs) Follow-upe 1st (n = 47): + 9.2 to 22 lbs 2nd (n = 47): + 4.7 to 9.2 lbs 3rd (n = 46): + 0.0 to 4.7 lbs 4th (n = 48): − 0.0 to 30 lbs |
Yes Larger declines in fasting leptin during weight loss associated with weight regain (P = 0.008) Change in fasting leptin during weight loss not associated with weight regain when limiting analysis to subjects losing >l0 lbs DNS |
No Baseline leptin not associated with weight regain (DNS) |
NT |
| Sumithran et al.47 | Subjects 34 (69% Women) Age (years) 56.0 ± 10.6 BMI (kg/m2) 34.7 ± 3.7 |
Approach Very low-calorie diet (500–550 kcal per day Weight-loss phase 8 weeks Maintenance phase 12 months |
Initial − 13.5 ± 0.5 kg Follow-up − 7.9 ± 1.1 kg |
No Declines in fasting leptin during weight loss not associated with weight regain (DNS) |
NT | NO Post-weight loss leptin not associated with weight regain (DNS) |
| Wang et al.48 | Subjects 96 Women Age (years) 29–49 BMI (kg/m2) Maintainers 34.5 ± 4.8 Regainers 33.3 ± 4.3 |
Approach Low-calorie diet (790 kcal per day) Weight-loss phase 8 weeks Maintenance phase 6 months |
Initial Maintainers − 11.2 kg Regainers − 9.5 kg Follow-up Maintainers − 14.5 Regainers − 5.6 kg |
No Declines in fasting leptin during weight loss was not predictive of weight regain (odd ratio exp(B) = 0.55, P = 0.60)f (Analysis controlled for change in weight) |
No Baseline leptin not associated with weight regain (odd ratio exp(B) = 0.56, P = 0.70)f |
NO Post-weight loss leptin not associated with weight regain (odd ratio exp(B) = 0.56, P = 0.95)f |
Abbreviations: BMI, body mass index; β, linear regression beta coefficient; DNS, data not shown; NT, not tested; OR, odds ratio; r, Pearson correlation coefficient. These studies are provided in chronological order, followed by alphabetical order.
Regainers = regained >40% of lost weight.
Maintainers = regained none.
Regainers = regained >10% of their weight.
Maintainers = regained none or <10% of their weight.
Quartiles of weight change.
Estimate from Volcano plot.
Table 3.
Studies of insulin sensitivity changes during weight loss and regain
| Author group and year of publication (citation) |
Sample description | Intervention | Initial weight loss and follow-up status |
Do increases in insulin sensitivity predict regain |
Does baseline insulin sensitivity predict regain |
Does end point insulin sensitivity predict regain |
|---|---|---|---|---|---|---|
| Yost et al.51 | Subjects 10 Women Age (years) 36 ± 2 BMI (kg/m2) 34.9 ± 1.1 |
Approach Low-calorie liquid diet (900 kcal per day) Weight-loss phase 3 months+ 3 months isocaloric maintenance Maintenance phase 18 months |
Initial − 11.4 ± 2.2 kg Follow-up 1.1 kg |
Yes Increases in insulin sensitivity during weight loss associated with weight regain (r2=0.78, P = 0.013) |
NT | NT |
| Wing Study 152 |
Subjects 125 subjects Age (years) 38.7 ± 5.0 BMI (kg/m2) 30.9 ± 2.2 |
Approach Behavioral weight loss program with kcal restriction (1000–1500 kcal per day) Weight-loss phase 6 months Maintenance phase 24 months |
Initial Study 1: − 9.8 ± 5.5 kg Follow-up Study 1: − 2 kg |
No Change in insulin sensitivity during weight loss not associated with weight regain (r = 0.00 for fasting insulin, r = − 0.08 for post glucose-load insulin) |
No Baseline insulin sensitivity not associated with weight regain (r = 0.08 for fasting insulin, r = − 0.01 for post glucose- load insulin) |
No Post-weight loss insulin sensitivity not associated with weight regain (r = 0.01 for fasting insulin, r = − 0.08 for post glucose- load insulin) |
| Wing Study 252 |
Subjects 33 T2D subjects Age (years) 55.8 ± 9.2 BMI (kg/m2) 36.5 ± 4.8 |
Approach Behavior modification plus very low-calorie diet (400–500 kcal per day) or balanced low-calorie diet (1000–1200 kcal per day) Weight-loss phase 6 months Maintenance phase 18 months |
Initial − 18 kg Follow-up − 8 kg |
No Change in insulin sensitivity during weight loss not associated with weight regain (r = 0.20) |
No Baseline insulin sensitivity not associated with weight regain (r = − 0.05) |
No Post-weight loss insulin sensitivity not associated with weight regain (r = 0.17) |
| Crujeiras et al.43 | Subjects 104 (47% Women) Age (years) 35 ± 6 BMI (kg/m2) 31.1 ± 2.9 |
Approach Hypocaloric diet (30% kcal restriction) Weight-loss phase 8 weeks Maintenance phase 6 months |
Initial − 5.0 ± 2.2% body weight Follow-up − 5.68% body weight 49 subjects regained at least 10% of lost weight 55 subjects maintained |
No Change in fasting insulin during weight loss not associated with weight regain (OR = 0.541, P = 0.153) |
No Baseline insulin not associated with weight regain (r = 0.013) |
No Post-weight loss insulin not associated with weight regain (r = 0.047) |
| Soni et al.41 | Subjects 200 Women Age (years) 57.1 ± 2.9 BMI (kg/m2) 30.3 ± 3.7 |
Approach Lifestyle intervention with restricted low-fat diet (1300–1500 kcal per day) Weight-loss phase 18 months Maintenance phase 12 months |
Initial − 10.5 lbs (range: + 18 to − 77.5 lbs) Follow-upa 1st (n = 47): + 9.2 to 22 lbs 2nd (n = 47): + 4.7 to 9.2 lbs 3rd (n = 46): + 0.0 to 4.7 lbs 4th (n = 48): − 0.0 to –30 lbs |
No Change in fasting insulin during weight loss not associated with weight regain (P = 0.30) |
No Baseline insulin not associated with weight regain (DNS) |
NT |
| Sumithran et al.47 |
Subjects 34 (69% Women) Age (years) 56.0 ± 10.6 BMI (kg/m2) 34.7 ± 3.7 |
Approach Very low-calorie diet (500–550 kcal per day) Weight-loss phase 8 weeks Maintenance phase 12 months |
Initial − 13.5 ± 0.5 kg Follow-up − 7.9 ± 1.1 kg |
No Change in fasting insulin not associated with weight regain (DNS) |
NT | No Post-weight loss insulin not associated with weight regain (DNS) |
Abbreviations: BMI, body mass index; DNS, data not show; NT, not tested; OR, odds ratio; r, Pearson correlation coefficient; T2D, type 2 diabetes. These studies are provided in chronological order, followed by alphabetical order.
Quartiles of weight change.
RESULTS
Characteristics of the included studies
Twelve articles met the inclusion criteria, ranging in date published from 1995 to 2011. Nine articles assessed the relationship between changes in leptin and weight regain. Four studies assessed the relationship between changes in ghrelin and weight regain. Six studies assessed the relationship between changes in indices of insulin sensitivity and weight regain (seven experiments in total; Wing52 discussed two interventions in one publication).
Do reductions in leptin during weight loss predict weight regain?
The nine articles examining relationships between changes in leptin during weight loss and weight regain are summarized in Table 1. Overall, the results are mixed. Only two of nine studies supported the hypothesis that decreases in leptin predict weight regain in free-living humans. Erez et al.40 found that weight regain was greatest in individuals with larger decreases in leptin during weight loss, supporting the hypothesis that decreases in leptin may be a determinant of weight regain. Soni et al.41 provided mixed support of their hypothesis. Decreases in leptin during the weight-loss phase were associated with weight regain during the maintenance phase; however, this association was lost when analyses were limited to participants who lost ≥10 lbs during the initial weight-loss phase.41 Three studies reported opposite results, such that a smaller decline in leptin during weight loss was associated with a larger weight regain.42–44 In the largest and most recent of these studies,43 the authors found that smaller decreases in leptin were significantly related to regain among men and women who had lost on average 5% of their weight during a low-calorie diet.43 Finally, four additional studies reported no association between leptin reductions during weight loss and subsequent weight change.45–48
A number of these studies also examined the association between baseline and/or post-weight loss leptin and weight regain; these findings are also mixed (Table 1). One study found that low baseline leptin levels were associated with weight regain.44 However, two studies demonstrated opposing findings, such that relatively higher baseline leptin concentrations were associated with greater weight regain.42,43 Four additional studies found no association between baseline leptin and subsequent weight change.41,45,46,48 The relationship of post-weight loss leptin with weight change was less frequently assessed. Two studies reported no correlation with subsequent weight change,47,48 whereas another found that higher end point leptin was associated with greater weight regain.43
Do increases in ghrelin during weight loss predict weight regain?
Four studies have directly tested relationship between ghrelin and weight regain.40,43,49,50 None of the available studies support hypothesis that higher levels of ghrelin predict weight regain (Table 2). Three studies found no association between weight loss-induced increases in ghrelin and weight regain,41,47,49 whereas one study by Crujeiras et al.43 found that decreases in ghrelin during weight loss increased the risk of regain. However, it should be noted that in the study by Crujeiras et al.,43 post-weight loss increases in ghrelin were small (12 pg ml−1) and statistically nonsignificant (P=0.461) and the average weight loss was relatively small (average 4.8 kg lost, regaining 10% of lost weight), suggesting that this finding should be interpreted with caution. Lower levels of ghrelin at baseline were found to be associated with greater weight regain in two studies,43,49 whereas no association between baseline ghrelin and weight change was noted in the third.41 Two studies found that lower post-weight loss ghrelin after weight loss was associated with weight regain.43,49 A third study found no relationship between post-weight loss ghrelin and weight regain.47 Taken together, almost no studies found that higher ghrelin measured at any time point during weight loss predicted more difficulty with weight loss maintenance.
Table 2.
Studies of ghrelin changes during weight loss and regain
| Author group and year of publication (citation) |
Sample description | Intervention | Initial weight loss and follow-up status |
Do increases in ghrelin predict regain | Does high baseline ghrelin predict regain |
Does high end point ghrelin predict regain |
|---|---|---|---|---|---|---|
| Garcia et al.49 | Subjects 48 Mexican women Age (years) 43.6 ± 7.9 BMI (kg/m2) 37.7 ± 7.9 |
Approach Behavioral intervention with calorie restriction (− 500 kcal per day) + Orlistat Weight-loss phase 6 months Maintenance phase 6 months |
Initial − 3.3 BMI units Follow-up − 3.8 BMI units |
No Weight loss-induced increases in fasting ghrelin return to baseline values with sustained weight loss maintenance (not statistically tested) |
NT | No Low post-weight loss ghrelin associated with weight regain (r = − 0.46, P<0.01) |
| Crujeiras et al.43 | Subjects 104 (47% Women) Age (years) 35 ± 6 BMI (kg/m2) 31.1 ± 2.9 |
Approach Hypocaloric diet (30% kcal restriction) Weight-loss phase 8 weeks Maintenance phase 6 months |
Initial − 5.0 ± 2.2% body weight Follow-up − 5.68% body weight |
No Decreases in fasting ghrelin during weight loss associated with weight regain (OR = 3.109, P = 0.008) |
No Low baseline ghrelin associated with weight regain (r = − 0.25, P = 0.012) |
No Low end point ghrelin associated with weight regain (r = − 0.26, P = 0.007) |
| Soni et al.41 | Subjects 200 Women Age (years) 57.1 ± 2.9 BMI (kg/m2) 30.3 ± 3.7 |
Approach Lifestyle intervention with low-fat diet (1300– 1500 kcal per day) Weight-loss phase 18 months Maintenance phase 12 months |
Initial − 10.5 lbs (range: + 18 to − 77.5 lbs) Follow-upa 1st (n = 47): + 9.2 to 22 lbs 2nd (n = 47): + 4.7 to 9.2 lbs 3rd (n = 46): + 0.0 to 4.7 lbs 4th (n = 48): − 0.0 to 30 lbs |
No Change in fasting ghrelin during weight loss not associated with weight regain (P = 0.10) |
No Baseline ghrelin not associated with weight regain (DNS) |
NT |
| Sumithran et al.47 | Subjects 34 (69% Women) Age (years) 56.0 ± 10.6 BMI (kg/m2) 34.7 ± 3.7 |
Approach Very low-calorie diet (500–550 kcal per day) Weight-loss phase 8 weeks Maintenance phase 12 months |
Initial − 13.5 ± 0.5 kg Follow-up − 7.9 ± 1.1 kg |
No Change in fasting ghrelin during weight loss not associated with weight regain (DNS) |
NT | No Post-weight loss ghrelin not associated with weight regain (DNS) |
Abbreviations: BMI, body mass index; DNS, data not shown; NT, not tested; OR, odds ratio; r, Pearson correlation coefficient. These studies are provided in chronological order, followed by alphabetical order.
Quartiles of weight change.
Do improvements in insulin sensitivity during weight loss predict weight regain?
As with both leptin and ghrelin, improvements in insulin sensitivity via weight loss do not seem to predict weight regain (Table 3). The earliest published study51 found that improvements in insulin sensitivity with weight loss predicted weight regain. However, results from five subsequent experiments do not confirm these results.41,43,47,52 For example, Wing52 reported that changes in insulin sensitivity did not predict weight regain in two separate experiments carried out in non-diabetic and type 2 diabetic subjects, respectively, following behavioral weight loss treatment that consisted of 6 months of weight loss and relatively long (2+ years) follow-up period to assess weight regain.52 Neither baseline41,43 nor end point43,47,52 measures of insulin sensitivity predicted weight regain.
DISCUSSION
This systematic review identified studies that assessed changes in leptin, ghrelin and insulin sensitivity during weight loss, and tested the relationship between such changes and weight regain. Strong evidence assert that biological adaptations of these factors to weight loss increase the propensity for weight regain.47,53–56 Yet, in reviewing clinical weight loss trials that assessed pre-post changes in leptin, ghrelin, and insulin sensitivity and weight regain, neither decreases in leptin or insulin sensitivity nor increases in ghrelin consistently predicted subsequent weight regain. Further, little evidence within the reviewed studies support pre- or post-weight loss leptin, ghrelin or insulin sensitivity as predictors of regain. These findings suggest that, despite the important roles that leptin, ghrelin and insulin seem to exert in energy homeostasis, their changes during weight loss, taken alone, are not sufficient predictors of weight regain in free-living humans.
Although leptin, ghrelin or insulin are typically measured and assessed throughout the literature as though they may singularly be predictive of weight regain, this is an unlikely scenario. Circulating hormones represent just one facet of a highly complex, systemic response that involves interactions between the central nervous system, the gut, adipose tissue, muscle tissue and the liver.30 Sex differences are also likely important, as the strongest evidence for leptin reduction as a predictor of weight regain was shown in a study consisting mainly of men,40 whereas women were more strongly represented in the majority of studies with nonsignificant results. Furthermore, the magnitude of change in leptin with weight loss differs by sex,57,58 as does hypothalamic sensitivity to leptin.59,60 Genetic variability also may alter such changes in and interactions between leptin, ghrelin or insulin, influencing the predictive ability of these biomarkers regarding weight regain.30,61
In addition, non-biological inputs can also influence the degree of weight maintenance or regain. An obesogenic environment is characteristic of many modern nations, marked by fast food promotion, high availability of sugar-sweetened beverages, large serving sizes paired with decreased opportunities for active transportation and recreation,62 in addition to other emerging factors that may have a role in obesity or weight regain.63–65 Such environmental pressures may overshadow biological or genetic control of body weight.66 In this case, teaching individuals how to successfully navigate food cravings or an obesogenic environment is necessary. Successful prevention of weight regain has been related to behaviors such as strictly adhering to a low-calorie, low-fat diet, performing high levels of physical activity (~2800 kcal energy expenditure per week), frequent self-weighing and breakfast consumption.67 Psychological variables, such as disinhibition, or self-reported loss of control over eating, have also been shown to predict weight regain.68 In addition, continued clinical contact has also been demonstrated to help prevent weight regain.69
Future directions
On the basis of our findings that weight loss adaptations in leptin, ghrelin and insulin alone do not appear to reliably predict weight regain in free-living individuals, it is clear that a multifactorial approach is necessary in order to adequately make such a prediction.
One aspect of a multifactorial approach may be assessing possible predictors in the postprandial, as well as the fasted, state. In each study reviewed, only the relationship between fasting values of leptin and ghrelin were assessed. These, and other biological factors, are extremely sensitive to acute caloric restriction and intake.70,71 In addition, obesity seems to not only affect fasting levels but also postprandial changes in both appetite hormones, which are thought to reinforce the obese state.72,73 Thus, researchers may want to examine whether the dynamic response of such factors to fasting and feeding provides a more reliable means of predicting weight regain. However, the addition of postprandial assessments does not address the issue that each hormone is but one factor contributing to a complex response.
Sumithran et al.47 suggested that the ability of hormonal adaptations to weight loss to promote weight regain may be a conglomerate effect, rather than resting on the change in one single hormone or peptide.47 In addition to the commonly assessed leptin, ghrelin or insulin, other important factors such as peptide YY, cholecystokinin, amylin and glucagon-like peptide-1 have significant impacts on appetite52 and should be considered in assessing conglomerate effects. Assessment of blood glucose homeostasis may also be pertinent, as hypoglycemia following an oral glucose tolerance test has been strongly correlated with weight regain.74
As several behaviors and environmental issues have been associated with weight change, it is imperative that a multifactorial approach includes biological and non-biological components. Typically, behavioral researchers have focused on behavioral variables, whereas physiological researchers have examined energy expenditure or hormonal changes. Each is explaining only a small proportion of the variance in weight regain. In order to better understand weight loss maintenance and regain, it is important that future studies assess a broad array of demographic characteristics, such as sex57 or genetics,75 behaviors, such as diet composition76 and physical activity77 and environmental factors66,69 as potential predictors, in addition to biological factors known to undergo adaptations to weight loss. Elucidating key biomarkers that can predict an individual’s risk based on biology, behavior and environment would be valuable in determining the most effective course of treatment, be it behavioral intervention for diet or exercise, pharmacological or surgical intervention.
Strengths and limitations
Using a thorough literature search, the present study included weight loss trials specifically designed to assess the relationships between weight loss-induced changes in leptin, ghrelin and insulin sensitivity and subsequent weight regain, making it the first comprehensive review of data addressing this question. However, it is important to note that the studies included in this review varied in demographic characteristics, approaches used to produce weight loss, the magnitude of weight loss and change in hormones, duration of follow-up and statistical methods used to analyze the relationship between hormonal changes and weight regain. In particular, the study conducted by Erez et al.40 was perhaps the most well designed to test the hypothesis that changes in leptin with weight predict weight regain in free-living individuals. In this study, multivariate regression models were adjusted for age, sex and other biomarkers that were potential confounders for weight loss.
Summary
Within a comprehensive review of relevant literature, we found no consistent relationship between individual changes in leptin, ghrelin and insulin sensitivity during weight loss and subsequent weight regain in free-living humans. Thus, changes in these hormones in and of themselves are not sufficient to predict weight regain. We further discuss a variety of suggestions aimed to strengthen future research in this area by addressing important limitations highlighted by the present review. Most important is utilizing a multidisciplinary approach that necessitates collaboration among researchers specializing in physiological, behavioral and environmental contributions to weight regain in order to more effectively predict outcomes regarding weight loss maintenance.
ACKNOWLEDGEMENTS
KS was supported by a T32 Training Fellowship (Training in Behavioral and Preventive Medicine; T32 HL076134).
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 3.Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–846. doi: 10.1038/nature05482. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, Clark JM, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes care. 2007;30:1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Gaal LF, Wauters MA, De Leeuw IH. The beneficial effects of modest weight loss on cardiovascular risk factors. Int J Obes Relat Metab Disord. 1997;21(Suppl 1):S5–S9. [PubMed] [Google Scholar]
- 6.Votruba SB, Blanc S, Schoeller DA. Pattern and cost of weight gain in previously obese women. Am J Physiol Endocrinol Metab. 2002;282:E923–E930. doi: 10.1152/ajpendo.00265.2001. [DOI] [PubMed] [Google Scholar]
- 7.Weiss EC, Galuska DA, Kettel Khan L, Gillespie C, Serdula MK. Weight regain in U.S. adults who experienced substantial weight loss, 1999–2002. Am J Prev Med. 2007;33:34–40. doi: 10.1016/j.amepre.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 8.Field AE, Wing RR, Manson JE, Spiegelman DL, Willett WC. Relationship of a large weight loss to long-term weight change among young and middle-aged US women. Int J Obes Relat Metab Disord. 2001;25:1113–1121. doi: 10.1038/sj.ijo.0801643. [DOI] [PubMed] [Google Scholar]
- 9.Sarlio-Lahteenkorva S, Rissanen A, Kaprio J. A descriptive study of weight loss maintenance: 6 and 15 year follow-up of initially overweight adults. Int J Obes Relat Metab Disord. 2000;24:116–125. doi: 10.1038/sj.ijo.0801094. [DOI] [PubMed] [Google Scholar]
- 10.MacLean PS, Higgins JA, Johnson GC, Fleming-Elder BK, Donahoo WT, Melanson EL, et al. Enhanced metabolic efficiency contributes to weight regain after weight loss in obesity-prone rats. Am J Physiol Regul Integr Comp Physiol. 2004;287:R1306–R1315. doi: 10.1152/ajpregu.00463.2004. [DOI] [PubMed] [Google Scholar]
- 11.MacLean PS, Higgins JA, Johnson GC, Fleming-Elder BK, Peters JC, Hill JO. Metabolic adjustments with the development, treatment, and recurrence of obesity in obesity-prone rats. Am J Physiol Regul Integr Comp Physiol. 2004;287:R288–R297. doi: 10.1152/ajpregu.00010.2004. [DOI] [PubMed] [Google Scholar]
- 12.MacLean PS, Higgins JA, Jackman MR, Johnson GC, Fleming-Elder BK, Wyatt HR, et al. Peripheral metabolic responses to prolonged weight reduction that promote rapid, efficient regain in obesity-prone rats. Am J Physiol Regul Integr Comp Physiol. 2006;290:R1577–R1588. doi: 10.1152/ajpregu.00810.2005. [DOI] [PubMed] [Google Scholar]
- 13.Beck EJ, Tapsell LC, Batterham MJ, Tosh SM, Huang XF. Oat beta-glucan supplementation does not enhance the effectiveness of an energy-restricted diet in overweight women. Br J Nutr. 2010;103:1212–1222. doi: 10.1017/S0007114509992856. [DOI] [PubMed] [Google Scholar]
- 14.Capel F, Klimcakova E, Viguerie N, Roussel B, Vitkova M, Kovacikova M, et al. Macrophages and adipocytes in human obesity: adipose tissue gene expression and insulin sensitivity during calorie restriction and weight stabilization. Diabetes. 2009;58:1558–1567. doi: 10.2337/db09-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Das SK, Gilhooly CH, Golden JK, Pittas AG, Fuss PJ, Cheatham RA, et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am J Clin Nutr. 2007;85:1023–1030. doi: 10.1093/ajcn/85.4.1023. [DOI] [PubMed] [Google Scholar]
- 16.de Luis DA, Sagrado MG, Conde R, Aller R, Izaola O. The effects of two different hypocaloric diets on glucagon-like peptide 1 in obese adults, relation with insulin response after weight loss. J Diab Complications. 2009;23:239–243. doi: 10.1016/j.jdiacomp.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Hayes MR, Miller CK, Ulbrecht JS, Mauger JL, Parker-Klees L, Gutschall MD, et al. A carbohydrate-restricted diet alters gut peptides and adiposity signals in men and women with metabolic syndrome. J Nutr. 2007;137:1944–1950. doi: 10.1093/jn/137.8.1944. [DOI] [PubMed] [Google Scholar]
- 18.Heini AF, Lara-Castro C, Kirk KA, Considine RV, Caro JF, Weinsier RL. Association of leptin and hunger-satiety ratings in obese women. Int J Obes Relat Metab Disord. 1998;22:1084–1087. doi: 10.1038/sj.ijo.0800731. [DOI] [PubMed] [Google Scholar]
- 19.Hietaniemi M, Jokela M, Rantala M, Ukkola O, Vuoristo JT, Ilves M, et al. The effect of a short-term hypocaloric diet on liver gene expression and metabolic risk factors in obese women. Nutr Metab Cardiovasc Dis. 2009;19:177–183. doi: 10.1016/j.numecd.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 20.Keim NL, Stern JS, Havel PJ. Relation between circulating leptin concentrations and appetite during a prolonged, moderate energy deficit in women. Am J Clin Nutr. 1998;68:794–801. doi: 10.1093/ajcn/68.4.794. [DOI] [PubMed] [Google Scholar]
- 21.Lien LF, Haqq AM, Arlotto M, Slentz CA, Muehlbauer MJ, McMahon RL, et al. The STEDMAN project: biophysical, biochemical and metabolic effects of a behavioral weight loss intervention during weight loss, maintenance, and regain. OMICS. 2009;13:21–35. doi: 10.1089/omi.2008.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med. 1995;1:1155–1161. doi: 10.1038/nm1195-1155. [DOI] [PubMed] [Google Scholar]
- 23.Olivan B, Teixeira J, Bose M, Bawa B, Chang T, Summe H, et al. Effect of weight loss by diet or gastric bypass surgery on peptide YY3-36 levels. Ann Surg. 2009;249:948–953. doi: 10.1097/SLA.0b013e3181a6cdb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenbaum M, Nicolson M, Hirsch J, Murphy E, Chu F, Leibel RL. Effects of weight change on plasma leptin concentrations and energy expenditure. J Clin Endocrinol Metab. 1997;82:3647–3654. doi: 10.1210/jcem.82.11.4390. [DOI] [PubMed] [Google Scholar]
- 25.Straznicky NE, Grima MT, Eikelis N, Nestel PJ, Dawood T, Schlaich MP, et al. The effects of weight loss versus weight loss maintenance on sympathetic nervous system activity and metabolic syndrome components. J Clin Endocrinol Metab. 2011;96:E503–E508. doi: 10.1210/jc.2010-2204. [DOI] [PubMed] [Google Scholar]
- 26.Verdich C, Toubro S, Buemann B, Lysgard Madsen J, Juul Holst J, Astrup A. The role of postprandial releases of insulin and incretin hormones in meal-induced satiety—effect of obesity and weight reduction. In J Obes Relat Metab Disord. 2001;25:1206–1214. doi: 10.1038/sj.ijo.0801655. [DOI] [PubMed] [Google Scholar]
- 27.Jequier E. Leptin signaling, adiposity, and energy balance. Ann N Y Acad Sci. 2002;967:379–388. doi: 10.1111/j.1749-6632.2002.tb04293.x. [DOI] [PubMed] [Google Scholar]
- 28.Levin BE, Keesey RE. Defense of differing body weight set points in diet-induced obese and resistant rats. Am J Physiol. 1998;274(2 Pt 2):R412–R419. doi: 10.1152/ajpregu.1998.274.2.R412. [DOI] [PubMed] [Google Scholar]
- 29.Lofgren P, Andersson I, Adolfsson B, Leijonhufvud BM, Hertel K, Hoffstedt J, et al. Long-term prospective and controlled studies demonstrate adipose tissue hypercellularity and relative leptin deficiency in the postobese state. J Clin Endocrinol Metab. 2005;90:6207–6213. doi: 10.1210/jc.2005-0596. [DOI] [PubMed] [Google Scholar]
- 30.Maclean PS, Bergouignan A, Cornier MA, Jackman MR. Biology’s response to dieting: the impetus for weight regain. Am J Physiol Regul Integr Compar Physiol. 2011;301:R581–R600. doi: 10.1152/ajpregu.00755.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosenbaum M, Sy M, Pavlovich K, Leibel RL, Hirsch J. Leptin reverses weight loss-induced changes in regional neural activity responses to visual food stimuli. J Clin Invest. 2008;118:2583–2591. doi: 10.1172/JCI35055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kissileff HR, Thornton JC, Torres MI, Pavlovich K, Mayer LS, Kalari V, et al. Leptin reverses declines in satiation in weight-reduced obese humans. Am J Clin Nutr. 2012;95:309–317. doi: 10.3945/ajcn.111.012385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–1630. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 34.Hansen TK, Dall R, Hosoda H, Kojima M, Kangawa K, Christiansen JS, et al. Weight loss increases circulating levels of ghrelin in human obesity. Clin Endocrinol. 2002;56:203–206. doi: 10.1046/j.0300-0664.2001.01456.x. [DOI] [PubMed] [Google Scholar]
- 35.Lejeune MP, Hukshorn CJ, Saris WH, Westerterp-Plantenga MS. Effects of very low calorie diet induced body weight loss with or without human pegylated recombinant leptin treatment on changes in ghrelin and adiponectin concentrations. Physiol Behav. 2007;91:274–280. doi: 10.1016/j.physbeh.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 36.Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–660. doi: 10.1038/45230. [DOI] [PubMed] [Google Scholar]
- 37.Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal MS, Suganuma T, et al. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000;141:4255–4261. doi: 10.1210/endo.141.11.7757. [DOI] [PubMed] [Google Scholar]
- 38.Cummings DE, Frayo RS, Marmonier C, Aubert R, Chapelot D. Plasma ghrelin levels and hunger scores in humans initiating meals voluntarily without time- and food-related cues. Am J Physiol Endocrinol Metab. 2004;287:E297–E304. doi: 10.1152/ajpendo.00582.2003. [DOI] [PubMed] [Google Scholar]
- 39.Wren AM, Seal LJ, Cohen MA, Brynes AE, Frost GS, Murphy KG, et al. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab. 2001;86:5992. doi: 10.1210/jcem.86.12.8111. [DOI] [PubMed] [Google Scholar]
- 40.Erez G, Tirosh A, Rudich A, Meiner V, Schwarzfuchs D, Sharon N, et al. Phenotypic and genetic variation in leptin as determinants of weight regain. Int J Obes. 2011;35:785–792. doi: 10.1038/ijo.2010.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soni AC, Conroy MB, Mackey RH, Kuller LH. Ghrelin, leptin, adiponectin, and insulin levels and concurrent and future weight change in overweight, postmenopausal women. Menopause. 2011;18:296–301. doi: 10.1097/gme.0b013e3181f2e611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Torgerson JS, Carlsson B, Stenlof K, Carlsson LM, Bringman E, Sjostrom L. A low serum leptin level at baseline and a large early decline in leptin predict a large 1-year weight reduction in energy-restricted obese humans. J Clin Endocrinol Metab. 1999;84:4197–4203. doi: 10.1210/jcem.84.11.6089. [DOI] [PubMed] [Google Scholar]
- 43.Crujeiras AB, Goyenechea E, Abete I, Lage M, Carreira MC, Martinez JA, et al. Weight regain after a diet-induced loss is predicted by higher baseline leptin and lower ghrelin plasma levels. J Clin Endocrinol Metab. 2010;95:5037–5044. doi: 10.1210/jc.2009-2566. [DOI] [PubMed] [Google Scholar]
- 44.Mavri A, Stegnar M, Sabovic M. Do baseline serum leptin levels predict weight regain after dieting in obese women? Diab Obes Metab. 2001;3:293–296. doi: 10.1046/j.1463-1326.2001.00134.x. [DOI] [PubMed] [Google Scholar]
- 45.Wing RR, Sinha MK, Considine RV, Lang W, Caro JF. Relationship between weight loss maintenance and changes in serum leptin levels. Horm Metab Res. 1996;28:698–703. doi: 10.1055/s-2007-979881. [DOI] [PubMed] [Google Scholar]
- 46.Vogels N, Westerterp-Plantenga MS. Successful long-term weight maintenance: a 2-year follow-up. Obesity. 2007;15:1258–1266. doi: 10.1038/oby.2007.147. [DOI] [PubMed] [Google Scholar]
- 47.Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–1604. doi: 10.1056/NEJMoa1105816. [DOI] [PubMed] [Google Scholar]
- 48.Wang P, Holst C, Andersen MR, Astrup A, Bouwman FG, van Otterdijk S, et al. Blood profile of proteins and steroid hormones predicts weight change after weight loss with interactions of dietary protein level and glycemic index. PLoS ONE. 2011;6:2. doi: 10.1371/journal.pone.0016773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garcia JM, Iyer D, Poston WS, Marcelli M, Reeves R, Foreyt J, et al. Rise of plasma ghrelin with weight loss is not sustained during weight maintenance. Obesity. 2006;14:1716–1723. doi: 10.1038/oby.2006.197. [DOI] [PubMed] [Google Scholar]
- 50.Goodpaster BH, Kelley DE, Wing RR, Meier A, Thaete FL. Effects of weight loss on regional fat distribution and insulin sensitivity in obesity. Diabetes. 1999;48:839–847. doi: 10.2337/diabetes.48.4.839. [DOI] [PubMed] [Google Scholar]
- 51.Yost TJ, Jensen DR, Eckel RH. Weight regain following sustained weight reduction is predicted by relative insulin sensitivity. Obes Res. 1995;3:583–587. doi: 10.1002/j.1550-8528.1995.tb00193.x. [DOI] [PubMed] [Google Scholar]
- 52.Wing RR. Insulin sensitivity as a predictor of weight regain. Obes Res. 1997;5:24–29. doi: 10.1002/j.1550-8528.1997.tb00279.x. [DOI] [PubMed] [Google Scholar]
- 53.Rosenbaum M, Goldsmith R, Bloomfield D, Magnano A, Weimer L, Heymsfield S, et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J Clin Invest. 2005;115:3579–3586. doi: 10.1172/JCI25977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cummings DE, Schwartz MW. Genetics and pathophysiology of human obesity. Ann Rev Med. 2003;54:453–471. doi: 10.1146/annurev.med.54.101601.152403. [DOI] [PubMed] [Google Scholar]
- 55.Ahima RS, Antwi DA. Brain regulation of appetite and satiety. Endocrinol Metab Clin North Am. 2008;37:811–823. doi: 10.1016/j.ecl.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 57.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 58.Nicklas BJ, Katzel LI, Ryan AS, Dennis KE, Goldberg AP. Gender differences in the response of plasma leptin concentrations to weight loss in obese older individuals. Obes Res. 1997;5:62–68. doi: 10.1002/j.1550-8528.1997.tb00284.x. [DOI] [PubMed] [Google Scholar]
- 59.Clegg DJ, Brown LM, Woods SC, Benoit SC. Gonadal hormones determine sensitivity to central leptin and insulin. Diabetes. 2006;55:978–987. doi: 10.2337/diabetes.55.04.06.db05-1339. [DOI] [PubMed] [Google Scholar]
- 60.Woods SC, Gotoh K, Clegg DJ. Gender differences in the control of energy homeostasis. Exp Biol Med (Maywood) 2003;228:1175–1180. doi: 10.1177/153537020322801012. [DOI] [PubMed] [Google Scholar]
- 61.Larsen LH, Angquist L, Vimaleswaran KS, Hager J, Viguerie N, Loos RJ, et al. Analyses of single nucleotide polymorphisms in selected nutrient-sensitive genes in weight-regain prevention: the DIOGENES study. Am J Clin Nutr. 2012;95:1254–1260. doi: 10.3945/ajcn.111.016543. [DOI] [PubMed] [Google Scholar]
- 62.Swinburn B, Egger G. The runaway weight gain train: too many accelerators, not enough brakes. BMJ. 2004;329:736–739. doi: 10.1136/bmj.329.7468.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McAllister EJ, Dhurandhar NV, Keith SW, Aronne LJ, Barger J, Baskin M, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49:868–913. doi: 10.1080/10408390903372599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hersoug LG, Sjodin A, Astrup A. A proposed potential role for increasing atmospheric CO2 as a promoter of weight gain and obesity. Nutr Diab. 2012;2:e31. doi: 10.1038/nutd.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tremblay A, Pelletier C, Doucet E, Imbeault P. Thermogenesis and weight loss in obese individuals: a primary association with organochlorine pollution. Int J Obes Relat Metab Disord. 2004;28:936–939. doi: 10.1038/sj.ijo.0802527. [DOI] [PubMed] [Google Scholar]
- 66.Muller MJ, Bosy-Westphal A, Heymsfield SB. Is there evidence for a set point that regulates human body weight? F1000 Med Rep. 2010;2:59. doi: 10.3410/M2-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S–225SS. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 68.Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, et al. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008;76:1015–1021. doi: 10.1037/a0014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev. 2012;13:509–517. doi: 10.1111/j.1467-789X.2011.00972.x. [DOI] [PubMed] [Google Scholar]
- 70.Wadden TA, Considine RV, Foster GD, Anderson DA, Sarwer DB, Caro JS. Short- and long-term changes in serum leptin dieting obese women: effects of caloric restriction and weight loss. J Clin Endocrinol Metab. 1998;83:214–218. doi: 10.1210/jcem.83.1.4494. [DOI] [PubMed] [Google Scholar]
- 71.Cummings DE, Shannon MH. Roles for ghrelin in the regulation of appetite and body weight. Arch Surg. 2003;138:389–396. doi: 10.1001/archsurg.138.4.389. [DOI] [PubMed] [Google Scholar]
- 72.Romon M, Lebel P, Fruchart JC, Dallongeville J. Postprandial leptin response to carbohydrate and fat meals in obese women. J Am Coll Nutr. 2003;22:247–251. doi: 10.1080/07315724.2003.10719300. [DOI] [PubMed] [Google Scholar]
- 73.le Roux CW, Patterson M, Vincent RP, Hunt C, Ghatei MA, Bloom SR. Postprandial plasma ghrelin is suppressed proportional to meal calorie content in normal-weight but not obese subjects. J Clin Endocrinol Metab. 2005;90:1068–1071. doi: 10.1210/jc.2004-1216. [DOI] [PubMed] [Google Scholar]
- 74.Boule NG, Chaput JP, Doucet E, Richard D, Despres JP, Bouchard C, et al. Glucose homeostasis predicts weight gain: prospective and clinical evidence. Diab Metab Res Rev. 2008;24:123–129. doi: 10.1002/dmrr.768. [DOI] [PubMed] [Google Scholar]
- 75.Farooqi IS. Genetic, molecular and physiological insights into human obesity. Eur J Clin Invest. 2011;41:451–455. doi: 10.1111/j.1365-2362.2010.02468.x. [DOI] [PubMed] [Google Scholar]
- 76.Sloth B, Due A, Larsen TM, Holst JJ, Heding A, Astrup A. The effect of a high-MUFA, low-glycaemic index diet and a low-fat diet on appetite and glucose metabolism during a 6-month weight maintenance period. Br J Nutr. 2009;101:1846–1858. doi: 10.1017/S0007114508137710. [DOI] [PubMed] [Google Scholar]
- 77.MacLean PS, Higgins JA, Wyatt HR, Melanson EL, Johnson GC, Jackman MR, et al. Regular exercise attenuates the metabolic drive to regain weight after long-term weight loss. Am J Physiol Regul Integr Comp Physiol. 2009;297:R793–R802. doi: 10.1152/ajpregu.00192.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]