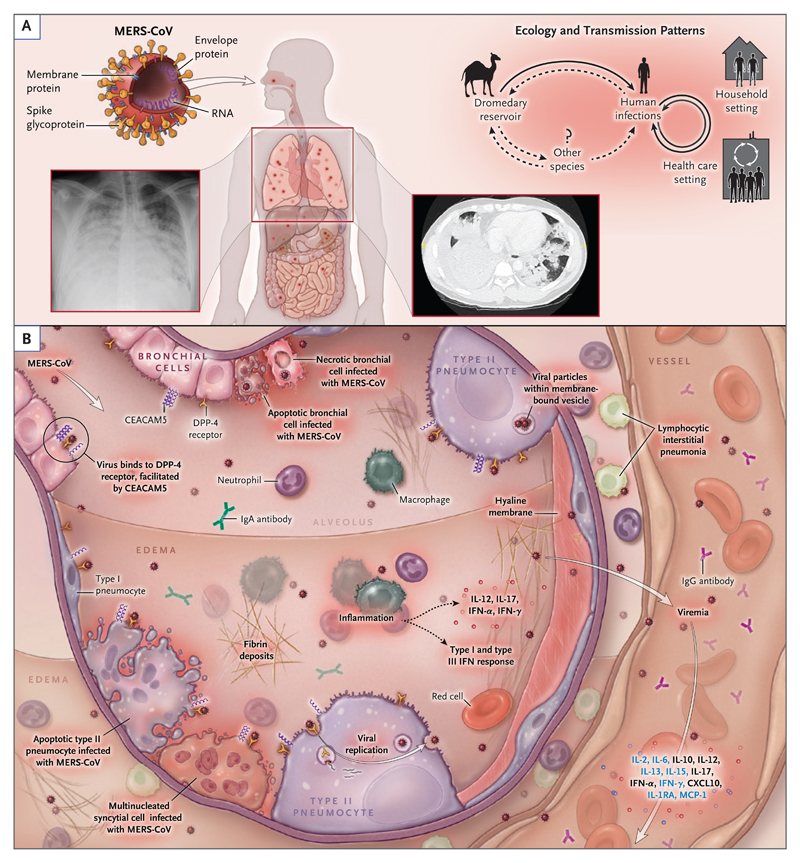
Figure 3. Transmission Patterns and Pathogenesis of the Middle East Respiratory Syndrome Coronavirus.
Panel A shows the structure, ecologic features, and transmission patterns of the Middle East respiratory syndrome (MERS) coronavirus (MERS-CoV). The virion surface is covered with the spike glycoprotein, a 149 kDa glycoprotein that extends outward to create a crownlike appearance. The spike glycoprotein is critical for binding the host-cell receptor, dipeptidyl peptidase 4 (DPP-4), to initiate infection. Dromedary camels are infected with the virus and are believed to be the most likely source of animal-to-human transmission. Human-to-human transmission in household and health care settings has also occurred. Panel B shows the current understanding of key events in MERS pathogenesis, which is based on limited observations in patients and data from animal and cell-culture model systems. After intratracheal inoculation of MERS-CoV in nonhuman primates, the virus infects bronchial epithelial cells through DPP-4 before spreading to lung parenchymal cells, including type I and type II alveolar pneumocytes and endothelial cells. Viral entry is facilitated by another cell-surface protein, carcinoembryonic antigen–related cell-adhesion molecule 5 (CEACAM5), which is also expressed in lung tissue. Inflammatory signaling molecules that are released by infected cells, alveolar macrophages, and neutrophils recruited to infected tissue have been detected in infected patients (black text) and animal models (blue text). A host antiviral type I and type III interferon response occurs, with systemic release of proinflammatory cytokines and chemokines.3,4 The virus may spread into the circulation, possibly from lung parenchyma or through infected endothelial cells. In humans, a high viral copy number has been detected in the lower respiratory tract, including tracheal aspirates and bronchoalveolar lavage specimens, as well as in peripheral blood. In advanced disease, diffuse alveolar damage is seen, with extensive hemorrhagic edema and hyaline membrane deposition. CXCL10 denotes C-X-C motif chemokine 10, IL interleukin, IL-1RA IL-1 receptor antagonist, IFN interferon, and MCP monocyte chemotactic protein.