Abstract
Objectives
To assess changes in phenotype and pressure sensitivity in patients with suspected opioid-induced-hyperalgesia (OIH) after transitioning to buprenorphine.
Methods
Twenty patients with suspected OIH were enrolled to transition to buprenorphine therapy. Patients completed validated self-report measures at baseline and at 1, 4, 8 weeks, and 6 months after initiation of buprenorphine along with quantitative sensory testing including measures of pressure pain threshold, pain tolerance and Pain 50 (a pain intensity rating).
Results
20 patients were enrolled, 17 were treated with buprenorphine and 11 completed all assessment points. We found that after transitioning to buprenorphine, patients on higher opioid doses (≥100mg oral morphine equivalents) had significant improvements for some measures including decreased pain severity and fibromyalgia survey scores, fewer neuropathic pain features, less catastrophizing, fewer depressive symptoms, and improved functioning 1-week after transitioning to buprenorphine with an eventual return back to baseline. Although not statistically significant, patients on high dose opioids (≥100mg OME) also showed a trend of decreased pressure sensitivity 1-week after transitioning to buprenorphine with a gradual return back to baseline.
Conclusions
Our study is the first to look at pressure pain sensitivity in patients who were taking opioids and transitioned to buprenorphine. These results suggest that the patients most likely to benefit from buprenorphine therapy are those on higher doses. In addition, the eventual return back to baseline on measures of pain phenotype and pressure sensitivity suggests that buprenorphine may over time result in a return of the hyperalgesic effects of a full mu agonist.
Keywords: Opioid-Induced Hyperalgesia, Buprenorphine, Pressure Sensitivity, Phenotypic Changes, Mu Agonists Withdrawal
INTRODUCTION
As many as 90% of the patients who present to pain centers for treatment are already taking opioids (1), yet few studies support a favorable risk: benefit ratio for their long-term use in patients with chronic nonmalignant pain (2–4). Our group previously demonstrated that patients on opioids with persistently high pain scores reported a phenotype consistent with having a more centralized pain state (fibromyalgia-like presentation), which suggests the potential presence of opioid-induced hyperalgesia (OIH)(5). OIH is defined in animal studies as a decrease in pain threshold from baseline after single or repeated administration of opioids (6, 7). Clinically, OIH is characterized by: (i) an increase in pain intensity over time, (ii) the spreading of pain to other locations beyond the initial painful site, and (iii) an increase in pain sensation to external stimuli (8).
The concerns of opioid abuse, diversion and accidental overdose, as well as the potential for OIH, along with the limited efficacy of long-term opioid management were also expressed in the recent CDC Guideline for Prescribing Opioids for Chronic Pain (9). This has spawned an interest in the use of buprenorphine in patients with pain and opioid dependence. Several promising studies have been performed in this area (10–14), but these have targeted changes in pain scores rather than looking at changes in pain phenotype and using quantitative sensory testing. In a previous study we found that patients with suspected OIH had increased pressure pain sensitivity when oral morphine equivalent was greater than 100mg/day (15). The primary objective of this prospective pilot study was to assess changes in phenotype and pressure pain sensitivity in patients with suspected OIH after transitioning to buprenorphine. We hypothesized that these patients would show an improvement in characteristics associated with centralized pain, as well as improvements in pressure pain sensitivity.
METHODS
The study was approved by the Institutional Review Board at the University of Michigan Medical School (Ann Arbor, MI). Written informed consent was obtained from all participants.
Study Setting and Participants
Twenty long-term opioid using patients treated at the Back & Pain Center (Department of Anesthesiology, Division of Pain Medicine, Ann Arbor, MI) were enrolled. All patients were transitioning off full mu agonist opioids to buprenorphine in order to specifically treat suspected OIH. Patients were evaluated by one of two physicians with expertise in managing addiction and OIH (HM or DB). Participants were paid a nominal amount for participating.
See Table 1 for inclusion and exclusion criteria. Before treatment, patients underwent blood testing for renal and liver function and urine drug testing utilizing both an enzyme-linked screening immunoassay and gas chromatography/mass spectroscopy.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria |
| Between ages of 18–65 |
| Speak English |
| Willing to cooperate with all study procedures |
|
|
| Exclusion Criteria |
| BMI > 40 |
| Medical conditions capable of causing patient’s symptoms and/or make it unsafe for them to participate |
| Untreated active addiction to illicit substance |
| History of consistent alcohol consumption: |
| exceeding 7 drinks/week for females |
| exceeding 14 drinks/week for males |
| Severe psychiatric illness |
| Prior history of allergies or intolerance to buprenorphine |
Pain Phenotyping
Demographics and current medications were recorded. The average daily dose of opioids was obtained and converted to oral morphine equivalents (OME) (15–17). Patients were phenotyped using validated self-report measures, including pain severity and interference (Brief Pain Inventory [BPI]) (18), neuropathic pain descriptors (PainDETECT [PDQ]) (19), depressive and anxiety symptoms (Hospital Anxiety and Depression Scale [HADS]) (20), pain catastrophizing (Catastrophizing subscale of the Coping Strategies Questionnaire) (21), sleep disturbance (PROMIS Sleep Disturbance ) (22, 23). fatigue (PROMIS Fatigue ) (22, 23), physical function (PROMIS Physical Function) (22, 23), 2011 Fibromyalgia Survey Criteria(24). As outlined in our prior studies (25, 26), our group proposes higher fibromyalgia survey scores represent pain that is more “centralized” in nature (e.g. altered central nervous system pain processing).
Quantitative Sensory Testing (QST)
The Multi-modal Automated Sensory Testing (MAST) System was used to assess pressure pain sensitivity. The MAST is a small, portable device designed for research and potential point-of-care applications (27–29). It applies pressure stimuli to the thumbnail bed. The use of this device has been described extensively elsewhere (15). The measures obtained were pain threshold, pain tolerance and Pain50 (pain intensity rating halfway between pain threshold and tolerance).
Follow-Up Assessment
At 1, 4, 8 weeks, and 6 months after the initiation of buprenorphine, participants returned for a medical evaluation and to complete the same questionnaires and experimental pressure pain testing protocol used at baseline.
Statistical Analysis
To examine the longitudinal trajectories of each phenotypic variable from baseline to 6 months, mean scores were plotted for the overall sample and for those with a baseline OME of less than 100mg or OME 100mg or greater. Differences between baseline and 1 week scores were compared using within-samples t-tests for those with OME < 100mg or OME ≥100mg. Longitudinal linear mixed models utilizing full information maximum likelihood (FIML) were conducted to test the overall trajectories of each score. Similarly, mean QST variables including threshold, tolerance, and P50 were plotted over time for the overall sample and for those with baseline OME < 100mg or OME ≥100mg. Differences between baseline and 1 week scores were compared using within-samples t-tests for those with OME < 100mg or OME ≥100mg. All available data were included in the analyses.
RESULTS
See Figure 1 for recruitment. For 20 patients, baseline demographic and OME data are presented in Table 2. Although the doses of buprenorphine for each visit were not recorded for all patients the most common range clinically used was from 2–16mg/day. Follow up and attrition are outlined in Figure 2.
Figure 1.
Patient flow chart to display patients screened, eligible, consented and completed for study.
Table 2.
Baseline Demographic and Oral Morphine Equivalent (OME)
| Mean (SD) | |
|---|---|
| Age | 44.5 (9.15) |
| Female | 13 (65%)a |
| Caucasian | 18 (90%) |
| Married | 14 (70%) |
| College graduate | 7 (35%) |
| OME | 77.5 [67]b |
| OME < 100 | 13 (65%) |
Count and percentage are presented for dichotomous data.
Median and interquartile range [IQR]
Figure 2.
Of the 20 patients consented, 11 patients completed the 6 month follow up.
Pain and Affective Phenotype Trajectory
Means across every time point for each phenotypic scale are presented in Figures 3 and 4. When examining patients with baseline OME < 100mg (n = 13) and those with OME ≥100mg (n = 7) separately, those with OME of ≥100mg experience a greater change from baseline to 1 week than those with OME < 100mg. Within-subjects t-tests confirmed that those with OME of ≥ 100mg had statistically significant improvements from baseline to 1 week for FM survey score (p = 0.020), BPI pain severity (p = 0.012), Pain DETECT (p = 0.032), Catastrophizing (p = 0.007), HADS depression (p = 0.021), and PROMIS Fatigue (p = 0.003). There were no statistically significant differences from baseline to 1 week for those with baseline OME < 100mg. Those with OME < 100mg had significant negative linear trends for BPI pain severity (p = 0.004), BPI pain interference (p = 0.044), Pain Detect (p = 0.002), FM score (p = 0.019), HADS anxiety (p = 0.003), Catastrophizing (p < 0.001) and PROMIS Sleep (p = 0.021). Those with an OME of ≥100 mg did not have any significant linear trends in any variable.
Figure 3.
Line graphs show average values for 4 of the 10 outcome variables from baseline to 6 month follow-up for the whole group, and for those on OME < 100 mg or OME ≥ 100 mg. Stars (*) denote statistical significance of at least p < 0.05 for change in outcome from baseline to 1 week follow-up. For patients taking 100mg or more OME, there were statistically significant decreases in FM survey score, catastrophizing, pain severity and depression (all ps < 0.05 or less) from baseline to 1 week follow-up.
Figure 4.
Line graphs show average values for 6 of the 10 outcome variables from baseline to 6 month follow-up for the whole group, and for those on OME < 100 mg or OME ≥ 100 mg. Stars (*) denote statistical significance of at least p < 0.05 for change in outcome from baseline to 1 week follow-up. For patients taking 100mg or more OME, there were statistically significant decreases in pain interference, neuropathic pain, and fatigue (all ps < 0.05 or less) from baseline to 1 week follow-up.
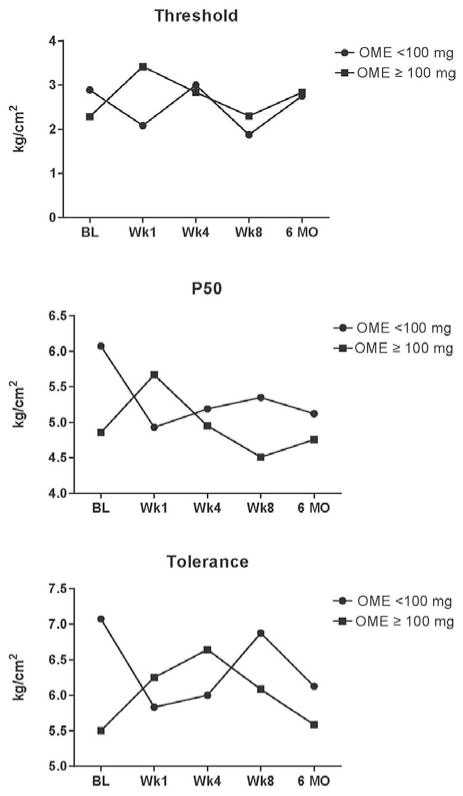
Quantitative Sensory Testing (QST) Trajectory
Plots of means across each time point for QST measures tolerance, threshold, and P50 are presented in Figure 5. Those with baseline OME < 100mg have initial decreases in tolerance, threshold, and P50. Those with baseline OME of ≥100mg have initial increases in tolerance, threshold, and P50. However, none of the baseline to 1-week differences for either group were statistically significant. There were no significant linear trends for any QST variable for those with OME < 100mg or those with OME ≥100mg.
Figure 5.
Line graphs show average values of threshold, P50, and tolerance at baseline to 6 month follow-up for those on OME < 100 mg or OME ≥ 100 mg.
DISCUSSION
We observed that patients on higher doses of opioids (≥100mg OME) had significant improvements for various measures of pain phenotyping associated with centralized pain after transitioning to buprenorphine. Our study is the first to look at pressure pain sensitivity in patients suspected of OIH being transitioned to buprenorphine. Although we were unable to detect a significant difference in pressure pain sensitivity, we did find a trend showing that patients on higher doses of opioids had improved pressure pain sensitivity at week 1. These results suggest that the patients with suspected OIH who are most likely to benefit from buprenorphine therapy are those on higher OME doses. Further, the eventual return back to baseline for measures of pain, mood and function, as well as pressure pain sensitivity suggests that buprenorphine may over time result in a return to the hyperalgesic effects of a full mu agonist.
Buprenorphine has been used as an effective agent for detoxification of patients on high dose opioids (17). However, what is not known is that once patients have been detoxified from the high dose opioids whether there is a role for continuation of buprenorphine long term. Based on our results it seems that long-term use of buprenorphine results in a gradual return to baseline hyperalgesia. It has been shown in animals that buprenorphine can induce hyperalgesia, which helps account for our findings (30).
LIMITATIONS
There are a number of limitations to our study. First, our sample size was small with only 20 participants and there was significant attrition; this is a challenging patient population not only to recruit but also to retain for a study. Also, the lack of a gold standard for clinical OIH diagnosis limits interpretation of these findings. Further, we used self-report questionnaires; however, all were well-validated measures. Finally, we did not control for buprenorphine dose and lower doses could influence return to baseline hyperalgesia. Nonetheless, these preliminary results suggest that it may be best to wean patients off of opioids altogether rather than to continue them on buprenorphine long term. This study excluded patients with a history of addiction, which may benefit from continued buprenorphine therapy regardless of the pain effects. Further, studies using larger cohorts are still needed to replicate our findings.
Acknowledgments
This study was supported by a Michigan Institute for Clinical and Health Research Grant 2UL1TR000433. The authors thank Kevin K Tremper, PhD, MD, Professor and Chairman of the Department of Anesthesiology at the University of Michigan, and Daniel Clauw, MD, Professor of Anesthesiology, Medicine (Rheumatology) and Psychiatry and Director of the Chronic Pain and Fatigue Research Center at the University of Michigan, for guidance and support. Furthermore, we thank the staff at the Back and Pain Center and the other members of the Division of Pain Research.
Footnotes
DISCLOSURES
Dr. Brummett receives research funding from Neuros Medical, Inc. (Willoughby Hills, OH) and is a consultant for Tonix Pharmaceuticals (New York, NY). Dr. Hassett has received research funding from and has been a consultant for Bristol-Myers Squibb (New York, NY) and Pfizer (New York, NY). Dr. Harte has received research funding from Cerephex (Palo Alto, CA), Forest Laboratories (New York, NY), Analgesic Solutions (Natick, MA), Regeneron (Tarrytown, NY), and deCode Genetics (Reykjavik, Iceland). Dr. Harte is co-inventor of the MAST device used in this study. For the remaining authors, there are no conflicts of interest to disclose.
References
- 1.Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2--guidance. Pain Physician. 2012;15(3 Suppl):S67–116. [PubMed] [Google Scholar]
- 2.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350:g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell G, Nielsen S, Bruno R, Lintzeris N, Cohen M, Hall W, et al. The Pain and Opioids IN Treatment study: characteristics of a cohort using opioids to manage chronic non-cancer pain. Pain. 2015;156(2):231–42. doi: 10.1097/01.j.pain.0000460303.63948.8e. [DOI] [PubMed] [Google Scholar]
- 4.Ballantyne JC. What can the POINT study tell us? Pain. 2015;156(2):201–2. doi: 10.1097/01.j.pain.0000460298.33454.9c. [DOI] [PubMed] [Google Scholar]
- 5.Wasserman RA, Brummett CM, Goesling J, Tsodikov A, Hassett AL. Characteristics of chronic pain patients who take opioids and persistently report high pain intensity. Reg Anesth Pain Med. 2014;39(1):13–7. doi: 10.1097/AAP.0000000000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Celerier E, Rivat C, Jun Y, Laulin JP, Larcher A, Reynier P, et al. Long-lasting hyperalgesia induced by fentanyl in rats: preventive effect of ketamine. Anesthesiology. 2000;92(2):465–72. doi: 10.1097/00000542-200002000-00029. [DOI] [PubMed] [Google Scholar]
- 7.Van Elstraete AC, Sitbon P, Trabold F, Mazoit JX, Benhamou D. A single dose of intrathecal morphine in rats induces long-lasting hyperalgesia: the protective effect of prior administration of ketamine. Anesth Analg. 2005;101(6):1750–6. doi: 10.1213/01.ANE.0000184136.08194.9B. [DOI] [PubMed] [Google Scholar]
- 8.Katz NP, Paillard FC, Edwards RR. Review of the Performance of Quantitative Sensory Testing Methods to Detect Hyperalgesia in Chronic Pain Patients on Long-term Opioids. Anesthesiology. 2015;122(3):677–85. doi: 10.1097/ALN.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 9.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 10.Daitch J, Frey ME, Silver D, Mitnick C, Daitch D, Pergolizzi J., Jr Conversion of chronic pain patients from full-opioid agonists to sublingual buprenorphine. Pain Physician. 2012;15(3 Suppl):ES59–66. [PubMed] [Google Scholar]
- 11.Pade PA, Cardon KE, Hoffman RM, Geppert CM. Prescription opioid abuse, chronic pain, and primary care: a Co-occurring Disorders Clinic in the chronic disease model. J Subst Abuse Treat. 2012;43(4):446–50. doi: 10.1016/j.jsat.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Roux P, Sullivan MA, Cohen J, Fugon L, Jones JD, Vosburg SK, et al. Buprenorphine/naloxone as a promising therapeutic option for opioid abusing patients with chronic pain: reduction of pain, opioid withdrawal symptoms, and abuse liability of oral oxycodone. Pain. 2013;154(8):1442–8. doi: 10.1016/j.pain.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malinoff HL, Barkin RL, Wilson G. Sublingual buprenorphine is effective in the treatment of chronic pain syndrome. Am J Ther. 2005;12(5):379–84. doi: 10.1097/01.mjt.0000160935.62883.ff. [DOI] [PubMed] [Google Scholar]
- 14.Berland DW, Malinoff HL, Weiner MA, Przybylski R. When opioids fail in chronic pain management: the role for buprenorphine and hospitalization. Am J Ther. 2013;20(4):316–21. doi: 10.1097/MJT.0b013e31827ab599. [DOI] [PubMed] [Google Scholar]
- 15.Wasserman RA, Hassett AL, Harte SE, Goesling J, Malinoff HL, Berland DW, et al. Pressure Pain Sensitivity in Patients With Suspected Opioid-Induced Hyperalgesia. Reg Anesth Pain Med. 2015;40(6):687–93. doi: 10.1097/AAP.0000000000000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E. Equianalgesic dose ratios for opioids. a critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22(2):672–87. doi: 10.1016/s0885-3924(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 17.McCaffery M, Pasero C. Pain: Clinical Manual. 2. St. Louis, MO: Mosby, Inc; 1999. Opioid Analgesics. [Google Scholar]
- 18.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38. [PubMed] [Google Scholar]
- 19.Freynhagen R, Baron R, Gockel U, Tolle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22(10):1911–20. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- 20.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17(1):33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 22.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38(6):1113–22. doi: 10.3899/jrheum.100594. [DOI] [PubMed] [Google Scholar]
- 25.Janda AM, As-Sanie S, Rajala B, Tsodikov A, Moser SE, Clauw DJ, et al. Fibromyalgia survey criteria are associated with increased postoperative opioid consumption in women undergoing hysterectomy. Anesthesiology. 2015;122(5):1103–11. doi: 10.1097/ALN.0000000000000637. [DOI] [PubMed] [Google Scholar]
- 26.Brummett CM, Janda AM, Schueller CM, Tsodikov A, Morris M, Williams DA, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119(6):1434–43. doi: 10.1097/ALN.0b013e3182a8eb1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harte SE, Mitra M, Ichesco EA, Halvorson ME, Clauw DJ, Shih AJ, et al. Development and validation of a pressure-type automated quantitative sensory testing system for point-of-care pain assessment. Med Biol Eng Comput. 2013;51(6):633–44. doi: 10.1007/s11517-013-1033-x. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt-Wilcke T, Ichesco E, Hampson JP, Kairys A, Peltier S, Harte S, et al. Resting state connectivity correlates with drug and placebo response in fibromyalgia patients. Neuroimage Clin. 2014;6:252–61. doi: 10.1016/j.nicl.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schrepf A, Bradley CS, O’Donnell M, Luo Y, Harte SE, Kreder K, et al. Toll-like Receptor 4 and comorbid pain in Interstitial Cystitis/Bladder Pain Syndrome: A Multidisciplinary Approach to the Study of Chronic Pelvic Pain research network study. Brain Behav Immun. 2015 doi: 10.1016/j.bbi.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wala EP, Holtman JR., Jr Buprenorphine-induced hyperalgesia in the rat. Eur J Pharmacol. 2011;651(1–3):89–95. doi: 10.1016/j.ejphar.2010.10.083. [DOI] [PubMed] [Google Scholar]