Figure 4. Diagnosing neuropathic pain, a.
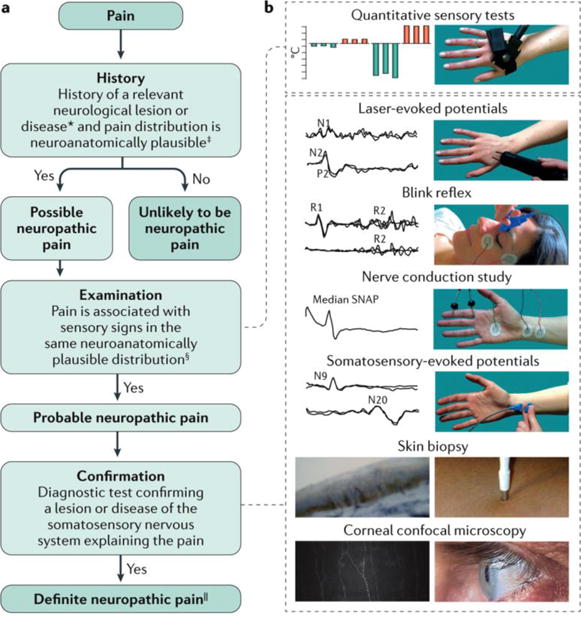
The flowchart summarizes the clinical steps in diagnosing neuropathic pain, which involves taking the patient history, examining the patient and following up with confirmatory tests. If the answer is ‘no’ after examination, the patient might still have probable neuropathic pain. In such cases, confirmation tests could be performed if sensory abnormalities are not found; for example, in some hereditary conditions, sensory abnormalities are not found at the moment of examination. *History of a neurological lesion or disease relevant to the occurrence of neuropathic pain. ‡The patient's pain distribution reflects the suspected lesion or disease. §Signs of sensory loss are generally required. However, touch-evoked or thermal allodynia might be the only finding at bedside examination. ||‘Definite’ neuropathic pain refers to a pain that is compatible with the features of neuropathic pain and confirmatory tests are consistent with the location and nature of the lesion or disease, although this may not imply any causality. b | The confirmatory tests for neuropathic pain include quantitative sensory testing (in which the patient provides a subjective report on a precise and reproducible stimulus), blink reflex testing (whereby the trigeminal afferent system is investigated by recording the R1 and R2 reflex responses recorded from the orbicularis oculi muscle) and nerve conduction study (which assesses non-nociceptive fibre function of the peripheral nerves). Somatosensory-evoked potentials (N9 is generated by the brachial plexus and N20 by the somatosensory cortex) and laser-evoked potentials (LEPs), both recorded from the scalp, are neurophysiological tools that investigate large and small afferent fibre function. The N1 LEP wave is a lateralized component and generated by the secondary somatosensory cortex, and the negative-positive complex of LEP (N2-P2) is a vertex recorded potential, which is generated by the insular cortex bilaterally and the cingulate cortex204. A skin biopsy enables the quantification of the intraepidermal nerve fibres, which provides a measure of small-fibre loss77. Finally, corneal confocal microscopy assesses corneal innervation, which consists of small nerve fibres. In most patients with neuropathic pain, standard neurophysiological testing, such as blink reflex, nerve conduction study and somatosensory-evoked potentials, is sufficient for showing the damage of the somatosensory system. However, in patients with selective damage of the nociceptive system, a nociceptive-specific tool, such as LEPs, skin biopsy or corneal confocal microscopy, is needed. Typically, tests are performed in the sequence of increasing invasiveness; that is, quantitative sensory testing, blink reflex, nerve conduction study, somatosensory-evoked potentials, LEPs, skin biopsy and corneal confocal microscopy. SNAP, sensory nerve action potential. Adapted with permission from REF 77, Macmillan Publishers Limited. The corneal innervation image in part b (left panel) is reproduced with permission from REF 86, Elsevier.
