Abstract
Background:
Hepatocellular carcinoma (HCC) is a major cause of cancer-related mortality worldwide and the incidence is increasing as a result of growing hepatitis B and C virus infections. Primary clear cell carcinoma of the liver (PCCCL) is a rare subgroup of primary HCC, which has low metastatic potential and infrequently reported in literature. Retroperitoneal and intrahepatic metastasis of PCCCL has not been reported previously.
Case Summary:
Here, we present a 55-year-old male with retroperitoneal and intrahepatic metastasis of PCCCL who is managed with surgical method and transcatheter arterial chemoembolization (TACE) at our institution. When the patient is followed up in 16 months after surgery and TACE, he is alive without any extrahepatic metastasis and abnomal liver function.
Conclusion:
We concluded that surgical resection of retroperitoneal metastasis and TACE of the intrahepatic tumors provided an appropriate strategy for the patient with unresectable PCCCL accompanied with extra-hepatic metastasis.
Keywords: clear cell carcinoma, hepatocellular carcinoma, intrahepatic metastasis, retroperitoneal metastasis, transcatheter arterial chemoembolization
1. Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third leading cause of cancer-related deaths worldwide. About 80% cases are reported from Asian countries, accounted for by the high prevalence of Hepatitis B and C infections in this region.[1] Extrahepatic metastasis of HCC at the time of initial diagnosis, even if the primary lesion is locally advanced, is however a rare phenomena.[2] Primary clear cell carcinoma of the liver (PCCCL) is a rare type of HCC, pathologically characterized by diffuse clear cells of the tumor, showing a clear cytoplasm that does not stain with hematoxylin-eosin.[3] Histologically, the tumor cells are moderately differentiated with low metastatic potential and diagnosis is usually made by correlation of histopathology, tumor markers, and immunohistochemistry. Treatment and prognosis of PCCCL with distal organ metastasis is infrequently reported in literature. We present an interesting case of PCCCL associated with retroperitoneal and intrahepatic metastasis in a hepatitis B virus (HBV)-related cirrhotic patient with surgical resection and transcatheter arterial chemoembolization (TACE) management. To the best of our knowledge, this is the first report of such a case in the worldwide.
2. Case presentation
This study was approved by the Institutional Ethic Committee of West China Hospital, Sichuan University. Written informed consent was obtained from this patient. The patient was a 55-year-old male who presented with a 1-month history of persistent right upper quadrant abdominal pain referred to the right shoulder, associated with episodes of chills and fever along with 5 kg weight loss and anorexia. There were no significant medical co-morbidities, other than positive Hep B status, or medication history and there was a 30 pack year history of smoking with moderate alcohol intake. On examination, the patient was hemodynamically stable with no evidence of jaundice and had some tenderness in the right upper quadrant.
Investigations revealed a white blood cell count of 11,730/mm3 with necrophilia (87%). Liver function tests (LFTs) were normal other than direct bilirubin, 9.8 μmol/L (normal range, <8.8 μmol/L); tumor markers showed elevated alpha-fetoprotein (AFP) 175.5 ng/mL (normal range, <8 ng/mL) and carbohydrate antigen 19–9(CA19–9) 30.44U/mL (normal range, <22U/mL). Carcinoembryonic antigen (CEA) and carbohydrate antigen-125 (CA-125) were within normal range. Serum hepatitis B surface antigen (HBsAg), e antibody (HBeAb), and core antibody (HBcAb) tests were positive, whereas serum hepatitis C antibody (HCVAb) was negative. Chest x-ray was unremarkable.
Abdominal CT showed a large, high-density retroperitoneal mass measuring 5.2 × 4.9 cm with complete capsule formation, which had no clear demarcation with the duodenum and the head of the pancreas. There was increased enhancement in the arterial and portal phase of the scan (Fig. 1A). Abdominal MRI revealed that the mass had a well-defined low-intensity T1-weighted image (Fig. 1B). Furthermore, there were many low-density nobes varying sizes throughout the liver and multiple enlarged lymph nodes in the hepatogastric ligaments and para-aortic region.
Figure 1.
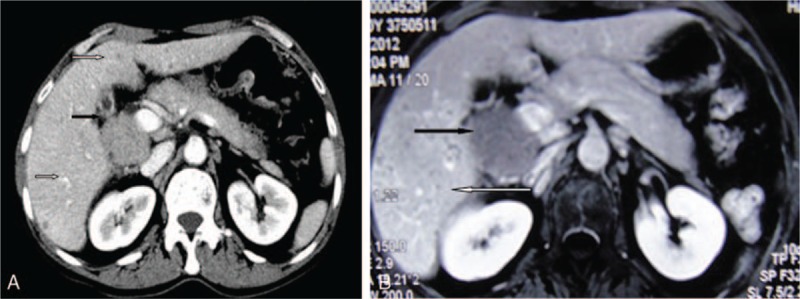
(A) Abdominal contrast CT scan showed the retroperitoneal mass (black arrow) and the multiple intrahepatic lesions (white arrow). (B) Axial T1-weighted MRI scan showing the retroperitoneal mass with low-intensity image (black arrow) and multiple intrahepatic lesions (white arrow). CT = computed tomography, MRI = magnetic resonance imaging.
A provisional diagnosis of pancreatic head or duodenal tumor with liver metastasis was made. The patient underwent an exploratory laparotomy and was found to have a gray–white, smoothly encapsulated retroperitoneal solid mass with a necrotic part in the center adherent to the duodenum and right colon with palpable lymph nodes in the lesser omentum. The liver had many low-density mostly about 2 to 3 mm, the largest about 2.6 cm in size. Given the extent of disease, a decision to perform cytoreductive surgery was made, since wide range hepatectomy was not possible. Intraoperative frozen histopathological examination indicated that the tumor in liver was HCC, but the reoperitoneal mass was of unclear origin and pancreatic endocrine tumor could not be excluded. Therefore, the retroperitoneal mass was completely excised and TACE were completed for the liver tumors. There were no intra- or postoperative complications and the patient was discharged 5 days after surgery. Interestingly, the final histopathology of the retroperitoneal mass was extra-hepatic metastasis of PCCCL. Hematoxylin and eosin (H&E) showed that an HCC with clear cell variant in the liver and retroperitoneal mass (Fig. 2A and B). The retroperitoneal mass had approximately 60% clear cells. Immunohistochemical staining of cells from the retroperitoneal mass showed that the tumor cells were positive for Hep1(Fig. 2C), epithelial membrane antigen (EMA), and Ki67 (about 40%), but negative for AFP, chromogranin A(CgA), Syn, CD56, Inhibin, renal cell carcinoma antigen (RCC) and melanoma antigen recognized by T cells 1(MART-1). These results supported a diagnosis of PCCCL with retroperitoneal and intrahepatic metastasis. Since TACE is safe and effective therapy for intrahepatic multiple tumors in advanced stage. On 16 months follow-up, the patient was asymptomatic with normal LFTs and no extrahepatic metastasis.
Figure 2.
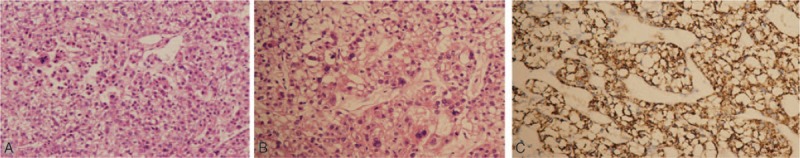
(A) Cells of liver tumor with clear cytoplasm visible on a background of cirrhosis (HE, ×150). (B) Cells from retroperitoneal tumor, mainly diffuse clear cells (60%) with a clear cytoplasm that did not stain with hematoxylin and eosin (HE, ×300). (C) Immunohistochemistry of the retroperitoneal tumor positive for Hep1 confirmed the tumor as hepatocellular carcinoma (×300). HE = hematoxylin-eosin.
3. Discussion
PCCCL is a rare entity accounting for 7.5% to 12.5% of all liver cancer cases and is infrequently reported in literature. [4] Liver cirrhosis is known to be an important risk factor for HCC and is strongly associated with PCCCL and focal PCCCL compared to non-PCCCL liver cancers.[5] It is accepted that cytoplasmic accumulation of lipid plays a major role in the development of the clear cytoplasm in PCCCL. PCCCL cells also have significantly fewer cytoplasmic organelles than non-PCCCL cells. In this case, we used the diagnostic criteria from pathologists in China to diagnose PCCCL, which has a cut off of >50% clear cells.[6] In the present case, the proportion of clear cells was approximately 60%.
PCCCL poses a diagnostic dilemma without the aid of the immunohistochemical staining. If only small tissue sections are available, an accurate diagnosis may not be possible histologically and in ambiguous cases it may be difficult to distinguish PCCCL from metastatic clear cell carcinomas originating in the adrenals, kidneys, ovaries, lung, and other organs. Cytokeratin profiling, and evidence of immunoreactivity for AFP and EMA, is probably a helpful criterion in making the differential diagnosis even in clear cell carcinomas of the liver. In our case, the diagnosis of PCCCL was further supported by raised serum AFP levels, and immunohistochemistry revealed Hep1 positivity, although EMA and AFP were negative.
Generally, PCCCL tumors display a low-grade malignancy, are encapsulated, and surgical resection is the most promising therapeutic treatment. The overall prognosis of PCCCL is still unclear as there are some reports suggesting that the outcome of patients with PCCCL is better than those with other types of HCC[7] and there are other data indicating that the prognosis of these patients is similar to its common type counterparts and may be even worse.[8,9] To date, there is no consensus on the treatment strategy for extrahepatic and intrahepatic metastasis of the PCCCL. The role of postoperative adjuvant chemotherapy in PCCCL is also controversial. We reviewed literature about retroperitoneal and intrahepatic metastatic PCCCL, only Kobayashi et al[10] reported 1 patient with retroperitoneal metastasis and intrahepatic recurrence of HCC. However, our case was different from that report, because the retroperitoneal metastasis of HCC happened after the liver resection and the exact subtype of pathological was not known. Similary, that patient was given the TACE for intrahepatic recurrent tumors and he was alive in his first year after surgery without any extrahepatic metastasis. For our case, on 16 months follow-up, the patient was also without extrahepatic metastasis and LFTs was normal.
However, some limitations of this report should be recognized. First, this is just a case report which restricted the promotion for our treatment method; therefore, a bigger patient population is needed in further research; Second, the long-term follow-up should be given to the patient for confirming this therapeutic effect; Third, some factors influence the outcome of the management, such as the preoperative serum AFP level, HBV infection and tumor size and proportion of clear cells. However, this report is just a case, so we cannot analyze the above factors.
In conclusion, we report a unique case of retroperitoneal and intrahepatic metastasis of PCCCL. In clinical practice, although there is presently no consensus on the optimum treatment strategy in this condition, therapeutic approaches to control intrahepatic tumors are important in improving patient survival. Our experience suggests that surgical resection of extrahepatic metastases and TACE for hepatic tumors provided an appropriate strategy for the patient with unresectable PCCCL accompanied with extra-hepatic metastasis and can be considered by other hepatopancreatobiliary teams.
Footnotes
Abbreviations: AFP = alpha-fetoprotein, CA-125 = carbohydrate antigen-125, CA19–9 = carbohydrate antigen 19–9, CEA = carcinoembryonic antigen, CgA = chromogranin A, EMA = epithelial membrane antigen, HBV = hepatitis B virus, HCC = hepatocellular carcinoma, LFTs = liver function tests, MART-1 = melanoma antigen recognized by T cells 1, PCCCL = primary clear cell carcinoma of the liver, RCC = renal cell carcinoma, TACE = transcatheter arterial chemoembolization.
Authorship: XL designed the research; JX and DH collected research data and wrote the manuscript; WH and XL revised the manuscript. XL reviewed the literature. All authors read and approved the final manuscript.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Han KH, Kudo M, Ye SL, et al. Asian consensus workshop report: expert consensus guideline for the management of intermediate and advanced hepatocellular carcinoma in Asia. Oncology 2011;81suppl 1:158–64. [DOI] [PubMed] [Google Scholar]
- [2].Lee HS. Management of patients with hepatocellular carcinoma and extrahepatic metastasis. Dig Dis 2011;29:333–8. [DOI] [PubMed] [Google Scholar]
- [3].Orsatti G, Arnold MM, Paronetto F. DNA image cytometric analysis of primary clear cell carcinoma of the liver. Arch Pathol Lab Med 1994;118:1226–9. [PubMed] [Google Scholar]
- [4].Takahashi A, Saito H, Kanno Y, et al. Case of clear-cell hepatocellular carcinoma that developed in the normal liver of a middle-aged woman. World J Gastroenterol 2008;14:129–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Emile JF, Lemoine A, Azoulay D, et al. Histological, genomic and clinical heterogeneity of clear cell hepatocellular carcinoma. Histopathology 2001;38:225–31. [DOI] [PubMed] [Google Scholar]
- [6].Cong WM, Zhang SH. Introduction of the rare types of HCC. Chin J Pathol 2002;31:457–60. [Google Scholar]
- [7].Wu PC, Lai CL, Lam KC, et al. Clear cell carcinoma of liver. An ultrastructural study. Cancer 1983;52:504–7. [DOI] [PubMed] [Google Scholar]
- [8].Shah S, Gupta S, Shet T, et al. Metastatic clear cell variant of hepatocellular carcinoma with an occult hepatic primary. Hepatobiliary Pancreat Dis Int 2005;4:306–7. [PubMed] [Google Scholar]
- [9].Adamek HE, Spiethoff A, Kaufmann V, et al. Primary clear cell carcinoma of noncirrhotic liver: immunohistochemical discrimination of hepatocellular and cholangiocellular origin. Dig Dis Sci 1998;43:33–8. [DOI] [PubMed] [Google Scholar]
- [10].Kobayashi S, Ueno M, Ohkawa S, et al. Retroperitoneal metastasis of hepatocellular carcinoma—a case report. Gan To Kagaku Ryoho 2011;38:465–8. [PubMed] [Google Scholar]


