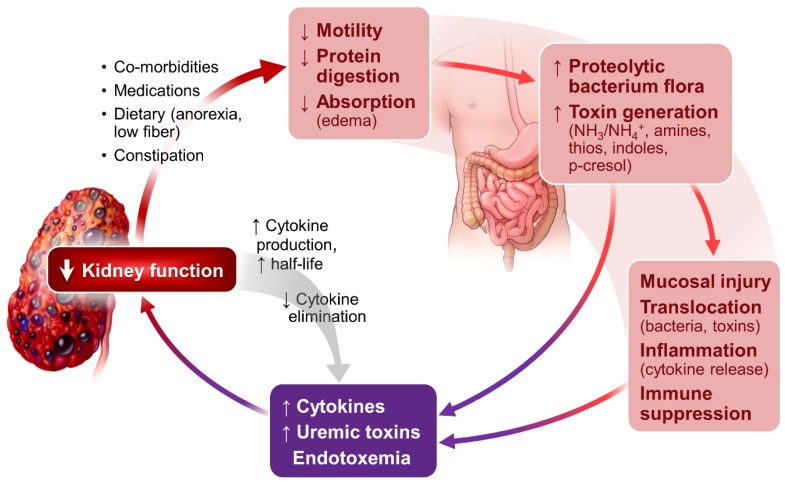
Figure 2.
Kidney-intestinal axis: Gastrointestinal-related inflammation and uremic toxin generation in CKD and ESRD. With progressive decline in kidney function, cytokine production and half-life increases while cytokine elimination decreases. CKD patients frequently have comorbidities (diabetes, hypertension, cardiovascular diseases, anemia and hyperphosphatemia) and are on multiple medications including diuretics (often with fluids restriction), iron preparations, phosphate binders and more that can slow bowel transit and cause constipation. With imposed dietary restrictions for CKD and ESRD, they tend to be on a diet low in fiber that can affect gut motility. Slow intestinal transit plus bowel mucosa edema (occurs often when patients with worsening kidney dysfunction and cardiovascular abnormalities) could alter protein digestion and bowel flora. Proteolytic bacteria floras are preferentially selected over the saccarolytic bacteria. The predominant proteolytic bacteria ferment luminal proteins and generate toxic metabolites and ammonia. The toxic metabolites would disrupt intestinal mucosal barriers causing increasing bacteria and toxin translocation. The systemic exposure and accumulation of these toxins and bacteria causes a low-grade but persistent endotoxemia. Adequate gut flora is known to enhance bowel integrity and promote immunoregulatory function. Disruption of normal flora could compromise gut immune function and, in the extreme, create a situation of “immunoparalysis”. The consequence of these effects is systemic cytokine activation, accumulation of uremic toxins and endotoxemia (purple rectangle).