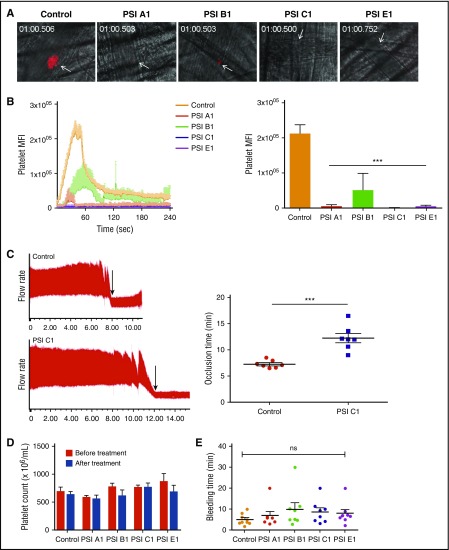
Figure 7.
Anti-β3 PSI mAbs inhibited thrombus formation in in vivo murine thrombosis models without significantly affecting tail bleeding time and platelet counts. C57 mice were injected anti-PSI mAbs before injury. Thrombus formation was monitored and recorded using a computerized digital camera. (A) Representative images showing that thrombosis was induced by a laser injury to the cremaster arterioles. In untreated mice (Control), thrombi reached their maximal size ∼40 seconds after injury. (B) IV injection with anti-PSI mAbs (5 μg in 100 μL saline) 30 minutes before injury significantly inhibited thrombus formation and growth (mean ± SEM; ***P < .001; n = 3 each). (C) FeCl3 injury in a carotid artery thrombosis model. PSI C1 (5 μg in 100 μL saline) pretreatment inhibited carotid artery thrombus formation. Left panel: representative tracing of carotid artery flow after FeCl3 injury. Arrows indicate the time of vessel occlusion. Right panel: statistical analysis of vessel occlusion time (mean ± SEM; **P < .01; n = 7). (D) Anti-PSI mAbs did not induce a significant platelet clearance. Mice were injected with saline or anti-PSI mAbs or anti-native β3 mAbs (5 μg in 100 μL saline). Platelet count was checked 40 minutes after injection (mean ± SEM; NS; n = 3). This result is different from other anti-β3 polyclonal or monoclonal antibody (eg, JAN D1. 9D2 or M1; supplemental Figure S7)–induced platelet clearance.46 (E) Anti-PSI mAbs did not significantly increase tail bleeding time. Mice were injected with anti-PSI mAbs (5 μg in 100 μL saline). Forty minutes after treatment, the bleeding times of each group were compared (mean ± SEM; NS; n = 8-9).