Fig. 2.
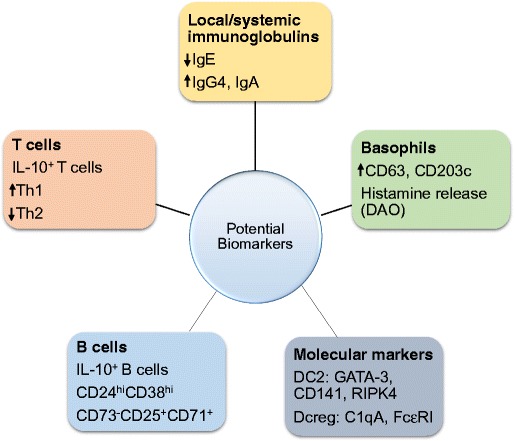
Biomarkers associated with allergen response and AIT. Biomarkers for various cell types may exhibit clinical benefit for allergen immunotherapy. The conventional T cell response to allergen mediating a CD4+ T cell response has been widely evaluated. The increase of CD4+ T cells in response to allergen elicits a Th2 cytokine storm such as IL-4, IL-5, and IL-13 causing an allergic response or asthma. On the other hand, Tregs have a protective role in allergy as they modulate immune tolerance to allergen and control the allergic reaction during allergen immunotherapy. AIT deviates the immune response towards Tregs increasing the IL-10 and TGF-ß production with a decrease in IgE, whereas the elevated IgG4 as well as IgA is mediated by B cells. The increase in Treg subsets Foxp3+ and Tr1 are also induced by AIT may be important biomarkers post-immunotherapy. The immune response can become resistant to immune deviation to Tregs/Th1 subsets; CD4+T cells (CD27-) expressing CRTH2 also produce a Th2 response. The CD27- (Th2) subset have been found to be decreased in AIT treated subjects, whereas the protective CD27+ (Th2) subset was elevated. Additionally, IL10+ Bregs can induce protective IgG4 response and inhibit the antigen-specific CD4+ T cell proliferation during AIT. Furthermore, the DC markers in response to immunotherapy have an increased DCreg (C1QA and FcεRIIIA) and decreased DC2 (GATA-3, CD141, and RIPK4) response. A novel biomarker for basophils has also been established intracellular expression of fluorochrome-labeled diamine oxidase, which was increased in SAR patients but reduced during SCIT and SLIT. The reduction in histamine, CD63, and CD203c by basophils was also associated with reduced symptoms.
