Abstract
Background
Coinfection with malaria and HIV is common in Sub-Saharan Africa. In the advent of a decline in the global incidence of malaria, it is important to generate updated data on the burden of malaria in people living with HIV (PLWHIV). This study was designed to determine the prevalence of malaria in PLWHIV in Yaounde, Cameroon, as well determine the association between CD4 + T cell count and malaria in the study population.
Methods
In a cross sectional study performed between April 2015 and June 2016, 355 PLWHIV were enrolled and blood samples were collected for analysis. Complete blood count was performed using an automated haematology analyser (Mindray®, BC-2800) and CD4 + T cell count was performed using a flow cytometer (BD FASCount™). Giemsa-stained blood films were examined to detect malaria parasite. The Pearson’s chi-square, student’s T-test, ANOVA, and correlation analysis were all performed as part of the statistical analyses.
Results
The prevalence of malaria observed in the study was 7.3 % (95 % CI: 4.8–10.6). No significant association was observed between the prevalence of malaria and age or gender. The prevalence of malaria was higher in participants who were not sleeping in insecticide treated bed nets, ITNs (p < 0.001); and in participants who were not on cotrimoxazole prophylaxis (p = 0.002). The prevalence of malaria (p < 0.001) and malaria parasite density (p = 0.005) were observed to be progressively higher in participants with CD4 + T cell count below 200cells/μl. Furthermore, the mean CD4 + T cell count was observed to be lower in participants coinfected with malaria compared to non-coinfected participants (323.5 vs 517.7) (p < 0.001). In this study, a negative correlation was observed between malaria parasite density and CD4 + T cell count (p = 0.019).
Conclusions
A low prevalence of malaria was observed in the study population. Some of the factors accounting for the low prevalence of malaria in this study population may include the health seeking habit of PLWHIV, the use of cotrimoxazole based chemoprophylaxis, and their cautious use of ITNs.
Keywords: Malaria, People living with HIV, Prevalence, Coinfection, CD4+ T cell count, Cotrimoxazole, ITNs, Cameroon
Background
Although the number of cases and death attributed to malaria have witnessed a decline recently, the disease is still responsible for a significant morbidity and mortality especially in sub-Saharan Africa (SSA) and in children below 5 years [1]. In 2015, there were 214 million cases of malaria worldwide, down from the 262 million cases reported in 2000, and within the same period, the number of deaths had decreased by 48 % [1]. Malaria is caused by parasitic protozoan of the genus Plasmodium. There are five species of Plasmodium which cause disease in humans namely; Plasmodium ovale, P. vivax, P. malariae, P. knowlesi and P. falciparum, with the latter being the most virulent accounting for the majority of cases and deaths attributed to malaria. As in most parts of SSA, P. falciparum is the predominant Plasmodium spp. in Cameroon, accounting for almost 100 % of all malaria-related cases [2].
SSA is also the region most affected by the HIV pandemic. In 2014, there were 25.8 million people living with HIV in SSA [3], accounting for approximately 70 % of the global total. Cameroon has one of the highest prevalence of HIV in West and Central Africa. In Cameroon, there were about 600,000 people living with HIV in 2013 [4]. HIV in Cameroon affects typically the poor and less privileged [5]. Because HIV is generally common among the youths, it therefore exerts a negative impact on the country’s economy (by weakening the major workforce of the country). The burden of HIV in Cameroon is also felt in the number of children who are orphaned by the disease [4, 6].
Malaria and HIV are both common in SSA because all the factors which favour transmission are present including poverty. Due to their overlapping distribution, coinfection with malaria and HIV are therefore bound to be common in the area. Coinfection with malaria and HIV is thought to have a synergistic effect, with studies reporting that repeated infection with malaria leads to a more rapid decline in CD4 + T cells overtime, meanwhile malaria coinfection with HIV results in more episodes of symptomatic malaria [7], and more episodes of severe or complicated malaria including death in both children and adults [8–12]. The risk of severe anaemia is also higher in HIV patients coinfected with malaria compared to HIV patients without malaria [13, 14].
Although the prevalence of coinfection between malaria and HIV had earlier been reported in some parts of Cameroon [12, 15], there is the need for continuous monitoring and epidemiologic enquiry to accommodate the current distribution of malaria which does not seem to be influenced only by the geographical setting but also changes overtime with variations in climatic conditions. This study was therefore designed to determine the prevalence of malaria in people living with HIV (PLWHIV) in Yaounde, Cameroon, and also to determine the association between the CD4 + T cell count and malaria. This will generate updated baseline data for clinico-epidemiologic purposes which will improve upon the management and control of both diseases.
Methods
Study area
This study was performed in Yaounde. Yaounde (3°52′N 11°31′E) with an average elevation of 750 m, is the capital of Cameroon. With a population of roughly 2.5million, Yaounde is second only to Douala as the largest city in Cameroon [16]. Yaoundé is a very diverse city with people from different works of life and is home to most of the administrative structures in the country. The climate of Yaounde is tropical with 2 rainy (March to June, September to November) and 2 dry seasons (December to February, July–August). The temperature here averages 23.7 °C, and Yaounde receives an average annual rainfall of 1643 mm [17]. Malaria transmission in Yaounde is holoendemic and seasonal with Anopheles gambiae as the main vector [18]. According to hospital records, peak malaria transmission occurs at the beginning of the rainy seasons. The prevalence of malaria in the general population of Yaounde is estimated at 35 % [19].
Study design and setting
This was a cross-sectional study performed between April 2015 and June 2016, involving PLWHIV. Participants were recruited at the Yaounde Military Hospital (YMH). The YMH is one of the main treatment facility for HIV/AIDS patients in Yaounde receiving close to a thousand HIV/AIDS patients every month, coming from all over Yaounde and it’s environ.
Sample size estimation
Using the following formula for sample size calculation [20];
Z = 1.96
p = prevalence of malaria among PLWHIV = 29.4 % [12].
e = error rate = 0.05
It was estimated that we will require a sample of at least 319 PLHIV.
Sampling technique
A convenient sampling technique was used, where PLHIV were consecutively recruited into the study as they came for consultation or to collect their ARV drugs.
Study population
PLWHIV were recruited at the HIV treatment center of the Yaounde Military Hospital. The study population consisted of HIV/AIDS patients on treatment and newly diagnosed cases (treatment-naïve). To be included in the study, participants were to be male or female of all ages. Participants were not to be on any antimalarial medication one week prior to the study. Participants were also required to provide a written informed consent, which was duly explained to them in English, French or the local Pidgin English. For minors and those who could not sign the informed consent, their parents, guardians, or next of kin did on their behalf.
Sample collection
Once participants gave their informed consent, their blood samples were collected. About 4 ml of blood was collected into EDTA anticoagulated test tubes following aseptic techniques, to perform the complete blood count (CBC) and CD4 + T cell count. Thick and thin blood films were also prepared for malaria microscopy.
Performance of CBC and CD4+ T cell counts
The CBC was performed using the Mindray® automatic haematology analyser (BC-2800, Shenzhen Mindray Bio-Medical Electronics Co., Ltd, Shenzhen, P.R., China).
CD4 + T cell counts were determined using a flow cytometer, BD FASCount™.
Detection of malaria parasites
Thick and thin blood films were prepared and stained with 10 % Giemsa and examined using methods previously described [21]. Blood films were read by two expert microscopists who were blinded from the results of the other. In case of any discrepancy with the results obtained by the two microscopists, a third was brought in and the results he gave was considered as final. The thick films were screened for at least 200 fields using the 100X (oil immersion) objective. If asexual parasites were observed, the density was then determined by counting the number of parasites against 500 leucocytes. The slides were only declared negative after counting to 2500WBC. The parasite density was obtained by dividing the number of parasites by 500 and multiplying the result by the actual white blood cell count of the patient obtained from the CBC results [22].
Statistical analysis
Data collected were entered into an Excel spreadsheet and analysed using the Stata® version 12.1 software (StataCorp LP, Texas, USA). The statistical tests performed included the Pearson’s Chi-square for comparison of proportions, the Student’s T-test and ANOVA for the comparison of group means, and correlation analysis to determine the association between parasite density and CD4 + T cell count. Statistical significance was set at p < 0.05.
Results
Four hundred and seven PLWHIV were approached, 355 of them meet the inclusion criteria and were therefore enrolled PLWHIV successfully took part into the study. Among them were 236 (66.5 %) females and 119 (33.5 %) males (Table 1). The ages of the participants ranged between 5 and 72 (mean ± SD = 35.29 ± 12.26). The mean duration of HIV was 3.0 ± 3.3 years. A majority (46.2 %) of the participants had a CD4+ T cell count above 500cells/μl. A bulk (78.9 %) of the participants reported to have been using insecticide treated bed nets (ITNs). Among the participants, 280 (78.9 %) were on antiretroviral therapy (ART) at enrollment, and 234 (65.9 %) were on prophylaxis with cotrimoxazole (Table 1).
Table 1.
Clinical and demographic characteristics of the study population
| Parameter | n (%) | |
|---|---|---|
| Age | <20 | 26 (7.3) |
| 20–39 | 208 (58.6) | |
| 40–59 | 107 (30.1) | |
| ≥60 | 14 (3.9) | |
| Total | 355 | |
| Gender | F | 236 (66.5) |
| M | 119 (33.5) | |
| Total | 355 | |
| On HAART | Yes | 201 (56.6) |
| No | 154 (43.4) | |
| Total | 355 | |
| Sleeping under ITN | Yes | 280 (78.9) |
| No | 75 (21.1) | |
| Total | 355 | |
| Mean (±SD) duration of HIV | HAART | 4.4 ± 2.5 |
| Naïve | 1.2 ± 3.4 | |
| Total | 3.0 ± 3.3 | |
| CD4+ T cell counts | <200 | 40 (11.3) |
| 200–499 | 151 (42.5) | |
| ≥500 | 164 (46.2) | |
| Total | 355 | |
| On prophylaxis with cotrimoxazole | Yes | 234 (65.9) |
| No | 121 (34.1) | |
| Total | 355 | |
Twenty six (26) of the 355 PLWHIV were infected with malaria parasite giving a prevalence of 7.3 % (95 % CI: 4.8–10.6). The prevalence of malaria was higher in individuals between 40 and 59years of age (Table 2). However no significant difference was observed between the prevalence of malaria and age (p = 0.960). The prevalence of malaria was higher in males compared to females (Table 2). Like the age, no significant association was observed between prevalence of malaria and gender in this study (p = 0.388). The prevalence of malaria was significantly higher in participants that were not sleeping under ITNs compared to those who were (p <0.001). The prevalence of malaria was also significantly higher in participants who were not on prophylaxis with cotrimoxazole (p = 0.002) (Table 2).
Table 2.
The distribution of malaria parasitaemia with respect to age, gender, HIV treatment status, CD4+ T cell counts, use of ITNs and cotrimoxazole prophylaxis
| Parameter | n (%) | Malaria positive n (%) | χ 2 | p-value | |
|---|---|---|---|---|---|
| Age | <20 | 26 | 2 (7.7) | 0.3 | 0.960 |
| 20–39 | 208 | 14 (6.7) | |||
| 40–59 | 107 | 9 (8.4) | |||
| ≥60 | 14 | 1 (7.1) | |||
| Total | 355 | 26 (7.3) | |||
| Gender | F | 236 | 15 (6.4) | 0.324 | 0.388* |
| M | 119 | 11 (9.2) | |||
| Total | 355 | 26 | |||
| On HAART | Yes | 201 | 13 (6.5) | 0.479 | 0.540* |
| No | 154 | 13 (8.4) | |||
| Total | 355 | 26 | |||
| Sleeping under ITN | Yes | 280 | 8 (2.9) | 39.0 | <0.001 |
| No | 75 | 18 (24.0) | |||
| Total | 355 | 26 | |||
| CD4+ T cell counts | <200 | 40 | 11 (27.5) | 28.5 | <0.001 |
| 200–499 | 151 | 10 (6.6) | |||
| ≥500 | 164 | 5 (3.1) | |||
| Total | 355 | 26 | |||
| On prophylaxis with cotrimoxazole | Yes | 234 | 10 (4.1) | 9.7 | 0.002 |
| No | 121 | 16 (13.2) | |||
| Total | 355 | 26 | |||
The CD4 + T cell count of the participants ranged between 38 and 1600 cells/μl (mean ± SD = 503.5 ± 276.2). The prevalence of malaria parasitaemia was higher in participants with CD4 + T cell count below 200 cells/μl and lowest in participants with counts above 500cells/μl (Table 2). A significant association was observed between prevalence of malaria and CD4 + T cell count (p < 0.001). Furthermore, the mean CD4 + T cell count was lower in patients coinfected with malaria parasites compared to non-coinfected participants (323.5 vs 517.7). The difference in the CD4+ T cell counts between malaria coinfected patients and non-coinfected patients was observed to be significant statistically (p < 0.001).
The geometric mean parasite density (GMPD) observed was 1219.7 parasites/μl. The GMPD was progressively higher in CD4 + T cell count below 200 cells/μl (Fig. 1). A Comparison between GMPD and the CD4 + T cell count category revealed a significant association (p = 0.005). Furthermore a negative correlation was observed between CD4 + T cell count and GMPD (r = −0.465, p = 0.019) (Fig. 2).
Fig. 1.
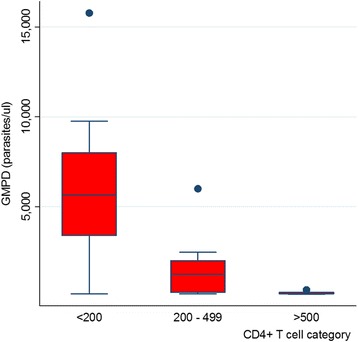
Distribution of the GMPD according to the different categories of CD4 + T cell count shows a progressively higher GMPD in patients with CD4 + T cell count below 200cells/μl (p = 0.005)
Fig. 2.
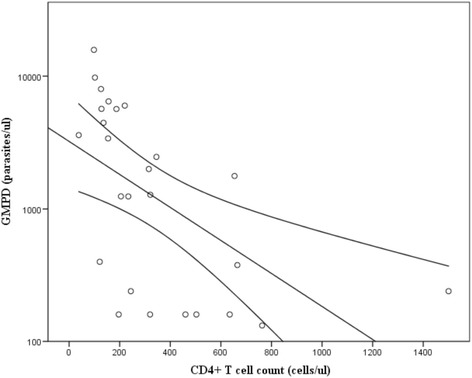
Fitted plot of CD4 + T cell count against malaria parasite density showing a negative correlation (r = −0.465, p = 0.019)
Discussion
Due to the overlapping distribution of malaria and HIV, coinfection between malaria and HIV are therefore common in SSA. With the declining trend in the global incidence of malaria [1], it is important to generate updated data on the burden of malaria in HIV. This study was aimed at determining the prevalence of malaria in PLWHIV in Yaounde, as wells as investigate the association between CD4+ T cell count and malaria.
In the current study. A prevalence of 7.3 % for malaria parasite was observed. This prevalence is lower compared to the prevalence of 34 % for malaria reported in the general population of Yaounde [19]. This prevalence is however higher compared to the 2.24 % reported in PLWHIV in Bamenda in the Northwest region of Cameroon [15]. Furthermore, the prevalence observed in this study is lower compared to similar studies performed in other countries; 11.75 % in Ghana [14], and 18.5 % in Nigeria [23]. The difference between the prevalence observed in these studies and ours could be due to the geographical differences in the study populations and the differences in the level of malaria endemicity. Malaria in Yaounde can be described as holoendemic and seasonal [18]. The prevalence is also very low compared to the prevalence of malaria in the other high risk groups including children (where prevalence could be as high as 98 % in some settings) [24], and pregnant women [25]. The low prevalence of malaria in this group could be attributed to the health seeking attitude of HIV patients. Studies have shown that malaria in HIV is more severe [8–13] and patients infected with malaria will quickly go down with the disease and seek medical attention faster. Another factor that could be responsible for the low prevalence of malaria in the target population is the use of cotrimoxazole (CTX) based chemoprophylaxis which is recommended for the protection against opportunistic infection in all PLWHIV in Cameroon. In this study, the prevalence of malaria among participants who were not on prophylaxis with cotrimoxazole was significantly higher than those who were on cotrimoxazole prophylaxis (p = 0.002). Trimethoprim-Sulfamethoxazole which is the active ingredient of CTX is also effective therapeutically against malaria [26, 27]. A study performed in Mozambique had shown that patients that were on CTX had lower risk of malaria compared to those that were not on CTX [13]. Regular use of ITNs could also be responsible for the low prevalence of malaria as evident from this study that 78.9 % of the patients reported to have been cautiously sleeping in ITNs bearing in mind their current status. ITNs have been made available to almost every household in Cameroon thanks to government efforts to increase coverage and encourage usage. In this study, the prevalence of malaria was significantly (p <0.001) higher in participants that were not sleeping under ITNs compared to those who were (24 % vs. 2.9 %), which confirms the benefit of using the ITNs. This finding is contrary to the study by Njunda et al. [15] in which no association was observed between the use of ITNs and prevalence of malaria.
In the current study, no significant association was observed between the prevalence of malaria and age (p = 0.960) or gender (p = 0.388). These findings echo earlier reports by Njunda et al. [15] and Ojurongbe et al. [23]. The majority of the study participants were adults which represent a low risk group for malaria unlike children (especially those below 5 years) who represent the most at risk group [1]. This may also have accounted for the low prevalence of malaria in this study. Studies investigating the burden of malaria in HIV-infected children will be required in the study area to provide a clearer picture. In the current study, no significant difference was observed in the prevalence of malaria between PLWHIV on ART and treatment naïve group (p = 0.540). This finding is in resonance with the study by Kimbi et al. [28].
Overall, the mean CD4 + T cell count observed was 503.5 cells/μl. As recommended by the government, treatment of HIV/AIDS in Yaounde and Cameroon as a whole commences at diagnosis and not dependent on the CD4 + T cell count as it was before. This may explain the generally high CD4 + T cell count of the study population. The prevalence of malaria was progressively higher in patients with CD4 + T cell count below 200cells/μl (p < 0.001). This is contrary to the study performed by Iroezondu et al. [29]. Furthermore, the CD4 + T cell count was significantly lower in HIV patients coinfected with malaria compared to those without, which confirms the study by Tay et al. [14] in which patients with malaria were also observed to have lower CD4 + T cell count. The finding of a significant association between malaria prevalence and CD4 + T cell count is contrary to studies performed elsewhere [23, 25].
The GMPD observed in this study was 1219 parasites/μl. The GMPD was also observed to be progressively higher in patients with CD4 + T cell count below 200cells/μl (p = 0.005). This increasing parasite density with decreasing CD4 + T cell count could be attributed to the weakening of the immune responses of these patients. Both the cellular and humoral immune responses are thought to play a role in the protection against malaria [30], and their activity is regulated by the CD4 + T cell. A depletion in the number of CD4 + T cells will therefore affect the cellular and humoral immune responses and consequently the immune responsiveness to malaria antigens [31, 32]. As the immunity weakens, it allows for the parasites to multiply hence disease progression. The finding of a significant negative correlation in this study further supports this hypothesis.
In the current study, only participants who attended the HIV/AIDS treatment center of the Yaounde Military Hospital were recruited. This may be biased against PLWHIV do not attend the facility or who did not come to the facility within the study timeframe. This may not give a true representation of PLWHIV in Yaounde. This serves as a major limitation of the study. In addition, the study was performed during the rainy season, a period well known for high malaria transmission. This also, may have affected the true representation of the prevalence of malaria in the study population, as data collected during the dry season may be lower. Studies to determine how the prevalence of malaria among PLWHIV varies with respect to season will therefore be needed in the study area.
Conclusion
A low prevalence of malaria was observed among PLWHIV in Yaounde, which is lower compared to prevalence reported in the general population of Yaounde. The prevalence was also lower compared to the prevalence reported in other countries in Sub-Saharan Africa. The low prevalence of malaria could be attributed to the wide use of insecticide treated bed nets and the cotrimoxazole based chemoprophylaxis in the study population. The prevalence of malaria parasitaemia was not observed to be associated with age or gender. The findings of a high prevalence of malaria and a higher parasite density in participants with CD4 + T cell count below 200cells/μl, as well as a negative correlation between the parasite density and the CD4 + T cell count is indicative of the role of the immune response in the protection against malaria in the target population.
Acknowledgement
The authors wish to thank the director, doctors, nurses and laboratory staff of the Yaounde Military hospital for allowing us to use their patients and for their help in data collection. Our sincere gratitude also goes to the patients who took part in this study.
Funding
This study was funded through the departmental research grant of the department of Medical Laboratory Sciences of the University of Buea.
Availability of data and materials
All the data supporting this findings have been presented in the manuscript.
Authors’ contributions
ALN conceived, designed and coordinated the study, and critically revised the paper. CN participated in the data collection, took part in the analyses and interpretation, and conducted the literature search and review. DSN and JCNA participated in the design of the study and the statistical analysis, and critically revised the paper. TEK participated in the data collection, took part in the analyses and interpretation, conducted the literature search and review, and wrote the first draft of the paper. All authors read and approved the final paper.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the Faculty of Health Sciences Institutional Review Board (IRB) of the University of Buea, Cameroon. Written informed consent was obtained from all participants prior to their inclusion.
Abbreviations
- ART
Antiretroviral therapy
- CD
Cluster of differentiation
- CTX
Cotrimoxazole
- GMPD
Geometric mean parasite density
- HIV
Human Immunodeficiency Virus
- ITN
Insecticide treated bed nets
- PLWHIV
People living with HIV
- SSA
Sub-Saharan Africa
Contributor Information
Anna Longdoh Njunda, Email: ann_njunda@yahoo.com.
Charles Njumkeng, Email: emmakwen@gmail.com.
Shey Dickson Nsagha, Email: nsaghads@hotmail.com.
Jules Clement Nguedia Assob, Email: juleclement@yahoo.fr.
Tebit Emmanuel Kwenti, Phone: + (237)697979776, Email: kwentitebit@yahoo.com.
References
- 1.World Health Organisation . World malaria report 2015. Geneva: World Health Organisation; 2015. [Google Scholar]
- 2.World Health Organisation . Cameroon: epidemiological profile. World malaria report. Geneva: WHO; 2010. [Google Scholar]
- 3.UNAIDS. Fact sheet 2015. http://www.unaids.org/sites/default/files/media_asset/20150901_FactSheet_2015_en.pdf. Accessed 17 Dec 2015.
- 4.UNAIDS. Cameroon: Epidemiological fact sheet on HIV and AIDS. http://www.unaids.org/sites/default/files/epidocuments/CMR.pdf. Accessed 17 Dec 2015.
- 5.Kwenti TE, Nsagha DS, Kwenti BDT, Njunda AL. Sexual risk behaviours among people living with HIV and implications for control in the north west region of Cameroon. World Journal of AIDS. 2014;4:198–205. doi: 10.4236/wja.2014.42025. [DOI] [Google Scholar]
- 6.Nsagha DS, Bissek AC, Nsagha SM, Assob JC, Kamga HL, Njamnshi DM, et al. The burden of orphans and vulnerable children Due to HIV/AIDS in Cameroon. Open AIDS J. 2012;6:245–58. doi: 10.2174/1874613601206010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamya MR, Gasasira AF, Yeka A, Bakyaita N, Nsobya SL, Francis D, et al. Effect of HIV-1 infection on antimalarial treatment outcomes in Uganda: a population-based study. J Infect Dis. 2006;193(1):9–15. doi: 10.1086/498577. [DOI] [PubMed] [Google Scholar]
- 8.Grimwade K, French N, Mbatha DD, Zungu DD, De-dicoat M, Gilks CF. Childhood malaria in a region of unstable transmission and high human immunodeficiency virus prevalence. Pediatr Infect Dis J. 2003;22(12):1057–1063. doi: 10.1097/01.inf.0000101188.95433.60. [DOI] [PubMed] [Google Scholar]
- 9.Grimwade K, French N, Mbatha DD, Zungu DD, De-dicoat M, Gilks CF. HIV infection as a cofactor for severe falciparum malaria in adults living in a region of unstable malaria transmission in South Africa. AIDS. 2004;18(3):547–554. doi: 10.1097/00002030-200402200-00023. [DOI] [PubMed] [Google Scholar]
- 10.Cohen C, Karstaedt A, Frean J, Thomas J, Govender N, Prentice E, et al. Increased prevalence of severe malaria in HIV-infected adults in South Africa. Clin Infect Dis. 2005;41(11):1631–1637. doi: 10.1086/498023. [DOI] [PubMed] [Google Scholar]
- 11.Otieno RO, Ouma C, Ong’echa JM, Keller CC, Were T, Waindi EN, et al. Increased severe anemia in HIV-1-exposed and HIV-1-positive infants and children during acute malaria. AIDS. 2006;20(2):275–280. doi: 10.1097/01.aids.0000200533.56490.b7. [DOI] [PubMed] [Google Scholar]
- 12.Nkuo-Akenji T, Tevoufouet EM, Nzang F, Ngufor N, Fon E. High prevalence of HIV and malaria co-infection in urban Douala, Cameroon. Afr J AIDS Res. 2008;7(2):229–235. doi: 10.2989/AJAR.2008.7.2.8.525. [DOI] [PubMed] [Google Scholar]
- 13.Saracino A, Nacarapa EA, da Costa Massinga EA, Martinelli D, Scacchetti M, de Oliveira C, et al. Prevalence and clinical features of HIV and malaria co-infection in hospitalized adults in Beira, Mozambique. Malar J. 2012;11:241. doi: 10.1186/1475-2875-11-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tay SCK, Badu K, Mensah AA, Gbedema SY. The prevalence of malaria among HIV seropositive individuals and the impact of the co- infection on their hemoglobin levels. Ann Clin Microbiol Antimicrob. 2015;14:10. doi: 10.1186/s12941-015-0064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Njunda LA, Kamga HLF, Nsagha DS, Assob JCN, Kwenti TE. Low malaria prevalence in HIV-positive patients in Bamenda, Cameroon. J Microbiol Res. 2012;2(3):56–59. doi: 10.5923/j.microbiology.20120203.03. [DOI] [Google Scholar]
- 16.World Gazetteer . Cameroon: largest cities and towns and statistics of their population. 2013. [Google Scholar]
- 17.Climate: Cameroon. http://en.climate-data.org/country/142/#example0. Accessed 17 Dec 2015.
- 18.Craig M, Snow R, le Sueur D. A climate-based distribution model of malaria transmission in sub-Saharan Africa. Parasitol Today. 1999;15(3):105–111. doi: 10.1016/S0169-4758(99)01396-4. [DOI] [PubMed] [Google Scholar]
- 19.van der Kolk M, Etti Tebo A, Nimpaye H, Ngo Ndombol D, Sauerwein R, Eling W. Transmission of Plasmodium falciparum in urban Yaoundé Cameroon is seasonal and age-dependent. Trans R Soc Trop Med and Hyg. 2003;97:375–379. doi: 10.1016/S0035-9203(03)90059-9. [DOI] [PubMed] [Google Scholar]
- 20.Swinscow TDV, Campbell MJ. Statistics at square. 10. London: BMJ books; 2002. [Google Scholar]
- 21.Njunda AL, Assob NJC, Nsagha SD, Kamga FHL, Mokenyu MD, Kwenti ET. Comparison of capillary and venous blood using blood film microscopy in the detection of malaria parasites: A hospital based study. Sci J Microbiol. 2013;2(5):89–94. [Google Scholar]
- 22.Research Malaria Microscopy Standards Working Group . Microscopy for the detection, identification and quantification of malaria parasites on stained thick and thin films. Geneva: World Health Organization; 2015. p. 25. [Google Scholar]
- 23.Ojurongbe O, Oyeniran OA, Alli OAT, Taiwo SS, Ojurongbe TA, et al. Prevalence of Plasmodium falciparum Parasitaemia and Its Correlation with Haematological Parameters among HIV-Positive Individuals in Nigeria. J Trop Med. 2014;161284:6. doi: 10.1155/2014/161284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Njunda AL, Fon SG, Assob JCN, Nsagha DS, Kwenti TDB, Kwenti ET. Malaria and intestinal parasitic coinfection and their contribution to anaemia in children in Cameroon. Infect Dis Poverty. 2015;4:43. doi: 10.1186/s40249-015-0078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnbull OS, Uche AP, Kesiena AJ, Francis FA, Oyemocho A, Obianwu IM, et al. Prevalence and risk factors of malaria in HIV-infected pregnant women on anti-retroviral therapy in Enugu, South East Nigeria. J AIDS Clin Res. 2014;5:321. [Google Scholar]
- 26.Wiktor SZ, Sassan-Morokro M, Grant AD, Abouya L, Karon JM, Maurice C, et al. Efficacy of trimethoprim-sulphamethoxazole prophylaxis to decrease morbidity and mortality in HIV-1-infected patients with tuberculosis in Abidjan, Côte d’Ivoire: a randomised controlled trial. Lancet. 1999;353:1469. doi: 10.1016/S0140-6736(99)03465-0. [DOI] [PubMed] [Google Scholar]
- 27.Hamel MJ, Greene C, Chiller T, Ouma P, Polyak C, Otieno K, et al. Does cotrimoxazole prophylaxis for the prevention of HIV-associated opportunistic infections select for resistant pathogens in Kenyan adults? Am J Trop Med Hyg. 2008;79:320. [PubMed] [Google Scholar]
- 28.Kimbi HK, Njoh DT, Ndamukong KJN, Lehman LG. Malaria in HIV/AIDS Patients at Different CD4+ T Cell Levels in Limbe, Cameroon. J Bacteriol Parasitol. 2013;4:164. [Google Scholar]
- 29.Iroezindu MO, Agaba EI, Okeke EN, Daniyam CA, Obaseki DO, Isa SE, et al. Prevalence of malaria parasitaemia in adult HIV-infected patients in Jos, North-central Nigeria. Niger J Med. 2012;21(2):209–13. [PubMed] [Google Scholar]
- 30.Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22(1):13–36. doi: 10.1128/CMR.00025-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ho M, Webster HK, Looareesuwan S, Supanaranond W, Phillips RE, Chanthavanich P, et al. Antigen-specific immunosuppression in human malaria due to Plasmodium falciparum. J Infect Dis. 1986;153:763–71. doi: 10.1093/infdis/153.4.763. [DOI] [PubMed] [Google Scholar]
- 32.Hviid L, Theander TG, Abu-Zeid YA, Abdulhadi NH, Jakobsen PH, Saeed BO, et al. Loss of cellular immune reactivity during acute Plasmodium falciparum malaria. FEMS Microbiol Immunol. 1991;3:219. doi: 10.1111/j.1574-6968.1991.tb04218.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data supporting this findings have been presented in the manuscript.


