Abstract
Background: More than a decade after the National Institute for Health and Clinical Excellence recommendation of home haemodialysis (home HD) for 10–15% of those needing renal replacement therapy, the uptake across different regions in the UK remains uneven.
Methods: This survey is part of the Barriers to Successful Implementation of Care in Home Haemodialysis (BASIC-HHD) study, an observational study of patient and organizational factor barriers and enablers of home HD uptake, in the UK. The study centres had variable prevalence of home HD by design [low: <3% (2), medium: 5–8% (2) and high: >8% (1)]. This survey was administered electronically in 2013, and had 20 questions pertaining to home HD beliefs and practices. A total of 104 members of staff across five study centres were approached to complete the survey.
Results: The response rate was 46%, mostly from experienced HD practitioners. Most believed in the benefits of home HD therapy. Across all centres, respondents believed that preconceptions about patients’ and carers’ ability to cope with home HD (35% to a great or very great extent) and staff knowledge and bias influenced offer of home HD therapy (45%). Also, compared with respondents from high prevalence (HP) centre, those from low prevalence (LP) centres felt that display and presentation of dialysis information lacked clarity and uniformity (44% versus 18%), and that a better set-up for training patients for self-care HD was required (72.8% versus 33.3%). A greater proportion of respondents from the HP centre expressed concerns over caregiver support and respite care for patients on home HD (63.7% versus 33.3%).
Conclusions: Survey results indicate that across all centres in the study, there is an appetite for growing home HD. There are some differences in attitudes and practice between LP and HP centres. There are other domains where all centres have expressed concern and addressing these will be influential in navigating change from the current course.
Keywords: chronic renal failure, chronic renal insufficiency, CKD, dialysis, haemodialysis
Introduction
The beginning of the 21st century has witnessed significant changes in the healthcare landscape within the National Health Service of the UK. In the context of renal replacement therapy, the emphasis has shifted from institutional care to self-managed dialysis, typically in patients’ own homes, and more recently, also in hospitals and free-standing units. These changes are compatible with higher expectations from informed patients, of their healthcare providers. In 2002, the National Institute for Health and Clinical Excellence (NICE) issued a technology appraisal guidance and provided practitioners with an ambitious target of 15% of the dialysis population for home haemodialysis (home HD) uptake in individual centres [1]. This was followed by the Renal National Service Framework (NSF) in 2004 recommending the delivery of high quality, clinically appropriate forms of dialysis to be designed around individual patient needs and preferences, keeping the target for maximizing delivery by the year 2014 [2]. Despite these initial measures, the renal registry recorded the national home HD figures at its lowest in 2006, with just 425 patients nationally (<1%) across the UK in receipt of home HD [3]. The salutary work of NHS Kidney Care, founded in 2008, and the idea of ‘care closer to home’ from Lord Darzi’s report, spanning the management of all long-term conditions [4, 5], gave the impetus to change practices across the UK.
Since 2010, there has been a gradual increase in the prevalence of home HD through several local, regional and national initiatives, and it currently stands at 4.7% nationally and varies from 0% to 14% across different centres [6]. Clearly, none of this rise is likely to have been achieved without the engagement of staff and the presence of clinical champions for home HD. In a qualitative study of financial incentives for promoting home-based HD, it was found that while the Department of Health tariff for home HD is not a clear incentive for its adoption due to uncertainty about operational costs, Commissioning for Quality and Innovation (CQUIN) targets were seen by the case study centres as a motivator to change practices [7]. The complex interplay of clinical, political and financial expertise, and interest-driven care provider attitudes to home HD therapy interleaved with ‘patient choice’ makes sustained improvement in services, tardy and varied.
In our survey of frontline healthcare providers, we seek to explore the beliefs and attitudes of the multidisciplinary team to home HD therapy, as we explore the larger question of barriers and enablers of home HD in the UK.
Materials and methods
This survey is part of the Barriers to Successful Implementation of Care in Home Haemodialysis (BASIC-HHD) study. This is a combined cross-sectional and prospective, mixed methods (convergent, parallel design) observational study of patient and organizational factors to investigate the facilitators and barriers of home HD therapy. The methodological details and scope of data collected in the BASIC-HHD study has been presented in the protocol paper [8]. The study centres had variable prevalence of home HD by design [low prevalence (LP) <3%, medium 5–8% and high prevalence (HP) >8%]. The total dialysis catchment population of all five study centres is 6.3 million.
This survey was administered electronically by a third party and it comprised 20 questions pertaining to home HD beliefs and practices (generated by the research team, see Supplementary Appendix 1) alongside the use of an instrument called the Organisational Culture Inventory® (OCI®), aimed at capturing cultural norms and expectations in an institutional set-up. The findings of the OCI® are outside the scope of this article. The outcomes of the dialysis practice questionnaire will be presented here. The survey demographics included primary role as care provider, primary area of operation, seniority, years in service, gender and the centre code (provided to anonymize responses for analysis). Potential respondents were identified by the principal investigators in each study centre. A total of 104 members of staff across five study centres were approached to complete the online survey between May and July 2013, with e-reminders every 2 weeks. The respondents also had the option of not identifying their centres and choosing a ‘prefer not to respond category’. Responses were made on a 5-point Likert scale (not at all, to a slight extent, to a moderate extent, to a great extent, to a very great extent).
Statistical analysis was carried out using SPSS 22. Descriptive statistics have been used to present the results, but statistical tests have been employed to compare the responses based on centre prevalence and primary role (nurses versus medical staff) of respondents. A two-sided 5% significance level was used throughout the analysis. Chi-squared tests, Fisher’s exact tests and Mann–Whitney U-tests were used to compare responses to survey questions between groups. A further comparison was also made between responses from those who identified their centres and those who did not.
Study registration
This BASIC-HHD study was reviewed and approved by the Greater Manchester West Health Research Authority National Research Ethics Service (NRES) Reference number: 12/NW/0170. The study is on the NIHR portfolio (ID 12346).
Results
Survey demographics are presented in Table 1. The survey had a 46% response rate overall (48 complete responses). The vast majority of respondents had >10 years of experience in the field and the majority belonged to the nursing fraternity, with equal proportions of ‘in-centre’ and ‘home therapies’ nursing staff. Medical staff responses primarily came from senior clinical staff. The centres to which they belonged were identified only by 27 participants, of which 9 respondents identified themselves from LP centres, 7 from medium prevalence and 11 from HP centres. The ‘prefer not to respond’ category was chosen by 44% (n = 21) of respondents.
Table 1.
Survey demographics
| Demographic | Respondent numbers | |
|---|---|---|
| Years in service | 1–2 | 0 |
| 2–5 | 3 | |
| 5–10 | 2 | |
| >10 | 45 | |
| Prefer not to respond | 1 | |
| Gender | Male | 12 |
| Female | 38 | |
| Prefer not to respond | 1 | |
| Primary role | Nursing | 43 |
| Medical | 7 | |
| Managerial | 1 | |
| Prefer not to respond | 0 | |
| Seniority | Consultant physicians | 5 |
| Registrar grade doctors | 2 | |
| Staff nurses | 17 | |
| Specialist senior nurses | 19 | |
| Managers | 4 | |
| Prefer not to respond | 4 | |
| Primary area of operation | Pre-dialysis service | 10 |
| Hospital HD | 18 | |
| Satellite HD | 5 | |
| Home HD | 4 | |
| Combined peritoneal and home HD | 8 | |
| Prefer not to respond | 5 | |
| Centre (complete data) | Low | 9 |
| Medium | 7 | |
| High | 11 | |
| Prefer not to respond | 21 | |
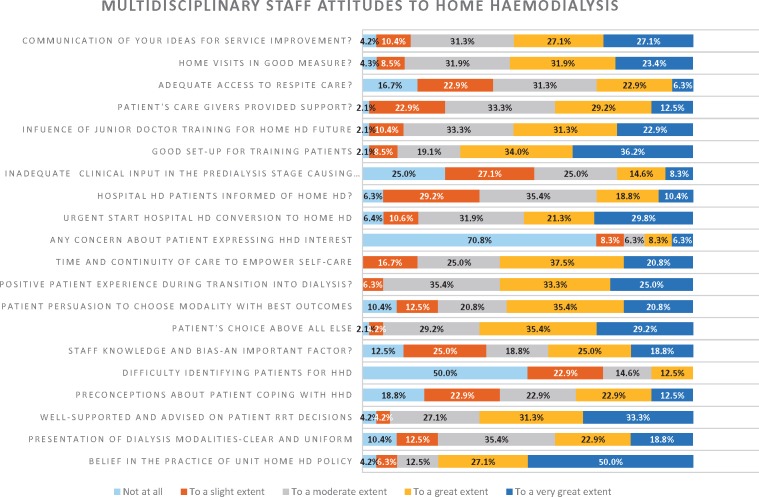
For description of responses to queries see Figure 1 and Table 2.
Fig. 1.
Multidisciplinary staff attitudes to home HD. HHD, home HD; RRT, renal replacement therapy.
Table 2.
Responses to questions depicted by centre prevalence and primary role provider
| Question | Response category | Centre prevalence |
Primary role provider |
|||
|---|---|---|---|---|---|---|
| Low (n = 9) (%) | High (n = 11) (%) | Nurse (n = 40) (%) | Medical + Managerial (n = 8) (%) | |||
| Q1 | Belief in the practice of unit home HD policy | Great extent + very great extent | 44.4 | 81.8 | 80 | 62.5 |
| Q2 | Presentation of dialysis information—clear and uniform | Not at all + to a slight extent | 44.4 | 18.2 | 20 | 37.5 |
| Q3 | Well supported and advised on patient RRT decisions | Great extent + very great extent | 66.6 | 63.7 | 62.5 | 75 |
| Q4 | Preconceptions about patients’ coping with home HD | Not at all + to a slight extent | 55.5 | 18.2 | 35 | 75 |
| Q5 | Difficulty identifying patients for home HD | Not at all + to a slight extent | 66.6 | 72.8 | 70 | 87.5 |
| Q6 | Staff knowledge and bias—an important factor? | Great extent + very great extent | 55.5 | 36.4 | 40 | 62.5 |
| Q7 | Patients’ choice above all else? | Great extent + very great extent | 44.4 | 54.6 | 65 | 62.5 |
| Q8 | Patient persuasion to choose modality with best outcomes | Not at all + to a slight extent + moderate extent | 55.5 | 36.4 | 50 | 12.5 |
| Q9 | Positive patient experience during transition into dialysis | Not at all + to a slight extent | 66.7 | 54.6 | 7.5 | 0 |
| Q10 | Time and continuity of care for to empower self-care in patients | Great extent + very great extent | 88.9 | 54.6 | 57.5 | 57.5 |
| Q11 | Any concern about patient expressing home HD interest? | Great extent + very great extent | 22.2 | 27.3 | 17.5 | 0 |
| Q12 | Urgent start hospital HD conversion to home HD | Great extent + very great extent | 44.4 | 53.8 | 46.1 | 75 |
| Q13 | Hospital HD patients informed of home HD? | Not at all + to a slight extent + moderate extent | 100 | 91 | 70 | 75 |
| Q14 | Inadequate clinical input in the pre-dialysis stage | Moderate extent + great extent + very great extent | 66.6 | 54.6 | 45 | 62.5 |
| Q15 | Good set-up for training patients in home HD | Great extent + very great extent | 33.3 | 72.8 | 67.5 | 85.7 |
| Q16 | Influence of junior doctor training for home HD future | Great extent + very great extent | 55.5 | 45.5 | 52.5 | 62.5 |
| Q17 | Patients’ caregiver provided support? | Not at all + to a slight extent | 22.2 | 45.5 | 22.5 | 37.5 |
| Q18 | Adequate access to respite care? | Not at all + to a slight extent | 33.3 | 63.7 | 40 | 37.5 |
| Q19 | Home visits in good measure? | Great extent + very great extent | 44.4 | 45.5 | 56.4 | 50 |
| Q20 | Communication of your ideas for service improvement | Not at all + to a slight extent | 22.2 | 18.2 | 50 | 75 |
Statistical tests using Fisher’s exact test was performed to determine the significance of the difference in proportions.
None of the differences reported is statistically significant, due to small numbers of respondents.
A 55% or greater difference in proportion would be statistically significant. RRT, renal replacement therapy.
The responses to the survey questions from 48 respondents have been depicted in a bar graph in Figure 1. The text below presents the results by categories of analyses. Although the responses were made on a Likert scale and have been presented as such in Figure 1, analysis was carried out by merging appropriate responses within the Likert scale, to suit the question being posed to the participant. Also, centre prevalence responses are presented between the extreme categories of LP and HP, so as to separate the responses.
Responses based on centre prevalence of home HD
It is evident from the bar graph that overall, there is a small proportion of respondents (10%) who do not identify with their unit HD policy. There exists a difference between the responses from participants in centres with LP (44.4%) and HP (81.8%) of home HD. Less than half (42%) of all respondents believed to a great extent that information was being presented clearly and uniformly by all staff members, with a greater proportion (44.4% versus 18.2%) of LP centres expressing concern. About 35% of respondents believed to a great or very great extent that their preconceptions about the patient’s ability to cope influenced their offer of home HD to the patient. This proportion was higher in the HP centre at 55.5% versus 18.2% in the LP centres. A larger proportion of respondents in the LP centre (55.5%) believe that staff knowledge and bias are important factors in home HD uptake compared with 36% in HP centre. About 89% of LP centre respondents and 54.6% of HP centre respondents felt to a great or very great extent that they could afford the time the patients needed to promote self-care. Only 29% of respondents across all centres felt that information on home HD transition was available for hospital HD patients. None of the respondents from LP centres and 9% of respondents from HP centre report that this information is adequately available to hospital HD patients. Only one-third of the respondents from LP centre (33%) as against 73% of respondents from HP centre believe they have a good training set-up for self-care HD. About 40% of all respondents feel patients have either no access or minimal access to respite care. This response is exaggerated from HP centres, with 63.7% of respondents feeling that patients have less access to respite care compared with 33.3% of LP centres’ and 28.6% of medium prevalence centres’ respondents.
Responses based on primary role of respondents
Table 2 depicts the responses of care providers in two categories—nursing staff and medical staff. Responses of managers who answered the survey (n = 1) have been combined with the responses of the medical staff due to their small numbers.
The majority of respondents from the medical and nursing fraternity appreciate home HD, although the medical staff does not believe that preconceived notions about the patient’s ability to cope with home HD is a deterrent to the offer of the therapy (75% versus 35%). All respondents agree that staff knowledge and bias is a significant issue and this is reported by a greater proportion of medical staff than nursing staff (62.5% versus 40%). Nursing staff are less likely to persuade patients to choose a specific modality based on better outcomes even when the patients are nervous about trying them (50% versus 12.5%). Some 75% of medical staff compared with 46% of nursing staff felt to a great or very great extent that urgent starts on hospital HD could convert to home HD at every available opportunity. Generally, providers report that inadequate clinical input in the pre-dialysis stage is the reason for high hospital dialysis starts, but this response is higher from medical staff (62.5% versus 45%).
Centre identifiers versus non-identifiers
Generally, for all the survey questions we examined the differences in responses to queries from those who identified their centres versus those who did not. No significant differences were observed in the pattern of their responses.
Statistical testing using Fisher’s exact test was performed to determine the significance of the difference in proportions. None of the differences reported is statistically significant, due to small numbers of respondents. A 55% or greater difference in proportion would be statistically significant.
Discussion
Several studies have been carried out over the years to better understand healthcare practitioners’ attitudes to home-based dialysis therapies [9–11]. Most practices globally have reported that the most commonly encountered impediments to expanding home-based HD services are financial disadvantage for home HD patients, and lack of physical infrastructure for training, support and education. The majority of nephrologists would recommend home HD to more patients if these impediments could be overcome [11].
This survey attempts to capture the gap between intent and practice of home HD across five locations in the UK with variable prevalence of home HD. In the decade since the NICE guidance, several schemes to incentivize home-based dialysis have been promoted by the Department of Health. The uptake of self-care dialysis therapies by patients can only be sustained by staff interest and expertise, although financial support can help resource these long-term projects. Patients engage with several members of staff during their treatment journey who provide their perspective on home HD, irrespective of the unit’s overarching policy on home therapies.
It is evident from our survey that not all healthcare professionals in an organization feel the same way about home HD. Therefore, there is likely to be asymmetry of intent and/or practice between centres with HP and LP of home HD. The majority of care providers do believe in the merits of home HD treatment. However, the chasm between the nature of responses from LP and HP centres in support of home HD may come as a surprise. Belief in therapy is paramount to promoting its practice. This is not limited to physicians alone and in fact applies to all members of the team who care for patients with end-stage renal disease (ESRD). Another aspect of practice that seemed obviously different between LP and HP centres was one of determining the patient’s suitability for home HD. While informed judgement of patients’ and carers’ ability to cope with home HD is welcome and essential, preconceptions about this may be misleading and deny the patient’s possibility of home HD therapy. Specific issues to consider include patient’s cognitive and technical ability, patient’s resolve, family support systems, etc., which may not be apparent at the outset. Our survey has shown that responses from practitioners in the HP centre have greater experience of larger numbers on home HD. More liberal criteria may allow for greater numbers of patients to consider this therapy, as greater experience is gathered. There may be greater risk of training failure in doing so, but it allows for objective evaluation of the patient’s ability to undertake self-care HD [12]. A recent study has established that an education initiative can modify the opinions of in-centre HD nurses towards home modalities and this should be incorporated into the many strategies for expanding a home HD programme [13].
A higher proportion of individuals in an LP centre feel that staff knowledge and bias influences offer of home HD therapy. Up to 45% of respondents across all centres believe this to be the case. There is evidence from other long-term conditions, such as diabetes, that structured self-management training programmes are vital initiatives to ensure uniform and consistent staff knowledge. Basing self-management practices upon knowledge and skills developed through practice and experience alone has been found to be insufficient preparation to deliver self-management in other chronic ailments, and in fact may be ineffective and inappropriate [14–16]. With an increasing trend for home HD, a nationally agreed structured educational initiative for all healthcare providers would be an appropriate next step in the ESRD self-care context. Trainees in nephrology need to be provided opportunities to train in home therapies. This may well include working alongside nurses, clinical psychologists and social workers, including visiting patients in their own homes, so that clinical medicine is not practised in a vacuum but in an appropriate, personalized, psychosocial context.
There appear to be other differences from a practice perspective too between LP and HP centres. These differences exist in the manner of display and presentation of dialysis information, perceived as being less uniform in LP centres. Over one-third of all practitioners surveyed also felt that hospital HD patients were not provided sufficient information to make a home transition. There are multiple information resources for patients during the pre-dialysis and hospital HD stages, but there is compelling evidence to suggest that an effective educational programme bodes well for self-care dialysis choice by patients [17]. More recently, a consensus conference outcome on the quality standards for pre-dialysis education was published [18]. Most of these recommendations are based on available qualitative and quantitative evidence, and need to be embraced more widely for a more uniform uptake of home HD.
Our survey shows that a greater proportion of respondents, particularly physicians, would persuade their patients to try home therapy. This is quite important as it is well known that physician validation of patient’s choice and confidence goes quite some way in helping patients choose home-based treatment [19]. The set-up for training patients to undertake self-care HD is vital to its success. Only one-third of the LP centre respondents felt satisfied with the infrastructure to train patients for home HD. Exemplary units with successful programmes have been forthcoming with how they have built their programmes on knowledge-sharing platforms such as conferences and also through team visits to such units. Initiatives such as the ‘Implementing hemodialysis in the home: A Practical Manual’, a peer-reviewed, comprehensive, open-source, web-enabled, practical manual supported by the International Society for Hemodialysis, can help discern the nuances of starting or expanding a home HD programme [20].
The survey also shows that a greater proportion of respondents from the HP centre expressed concerns over caregiver support and respite care for patients on home HD. While it is true that such problems are more obvious in centres that have larger patient numbers on home HD, informal caregiver support and respite care are crucial for the long-term success of a home HD programme [21]. The home respite care model may come with its own additional expenditure and staffing issues and the ‘in-centre’ respite care model may be inflexible with frequency of schedules or duration of treatment in what are usually dialysis units running to full capacity. The need to incorporate this aspect of care when designing the home programme cannot be emphasized enough. Other aspects of service provision that have been highlighted in this survey include the need to improve patient experience in transition from pre-dialysis to the dialysis phase, as less than 60% of respondents perceive it to be optimal and 50% of respondents feel the need for greater clinical input in the pre-dialysis stage to optimize self-care dialysis uptake.
The survey has its limitations in the 46% response rate and is further limited by the option of anonymized centre responses. That having been said, there was no difference in the type of responses from either group. Typically, a survey can project only broad perspectives. Survey responses may be limited by the number of questions posed. Practices in individual units may be influenced by local agreements with clinical commissioning groups and may change over time to reflect the national recommendations. The process of recruiting respondents for the survey may be biased despite attempts to include all care providers in the patients’ treatment journey, perhaps limiting responses only from enthusiastic professionals or a selection bias by the local investigator.
In conclusion, across all centres in the study, there is an appetite for growing home HD. There are some differences in attitudes and areas of practice between LP and HP centres, articulated in the responses to the survey questions. There are other domains where all centres have expressed concern and addressing these will be influential in navigating change from the current course.
Supplementary data
Supplementary data are available online at http://ckj.oxfordjournals.org.
Supplementary Material
Acknowledgements
We acknowledge the contribution of Human Synergistics International in administering the dialysis practice questionnaire annexed to Organisational Culture Inventory®. Baxter Healthcare Corporation is also acknowledged for the funding of the larger project, the BASIC-HHD study through the Baxter Extramural Grant. We sincerely thank all healthcare professionals who participated in this survey for their time and effort in contributing to our understanding of the barriers to and enablers of home haemodialysis.
Conflict of interest statement
None declared.
References
- 1. NICE/TA48. Guidance on home compared with hospital haemodialysis for patients with end-stage renal failure.2002. https://www.nice.org.uk/guidance/ta48 (10 January 2016, date last accessed)
- 2. Department of Health, Renal team. The National Service Framework for Renal Services Part 1: Dialysis and Transplantation 2004. (10 January 2016, date last accessed)
- 3. Castledine C, Gilg J, Rogers C et al. UK Renal Registry 13th Annual Report (December 2010): Chapter 15: UK renal centre survey results 2010: RRT incidence and use of home dialysis modalities. Nephron Clin Pract 2011; 119 (Suppl 2): c255–c267 [DOI] [PubMed] [Google Scholar]
- 4. Department of Health. A mandate from the Government to the NHS Commissioning Board: April 2013 to March 2015.2013. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/256497/13-15_mandate.pdf. (10 January 2016, date last accessed)
- 5. Darzi LA. High quality care for all. NHS Next Stage Review Final Report.2008. (10 January 2016, date last accessed)
- 6. Rao A, Casula A, Castledine C.. UK Renal Registry 17th Annual Report: Chapter 2 UK Renal Replacement Therapy Prevalence in 2013: National and Centre-specific Analyses. Nephron 2015; 129 (Suppl 1): 31–56 [DOI] [PubMed] [Google Scholar]
- 7. Abma I. et al. Perceptions and experiences of financial incentives: a qualitative study of dialysis care in England. BMJ Open 2014; 4: e004249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jayanti A. et al. Barriers to successful implementation of care in home haemodialysis (BASIC-HHD): 1. Study design, methods and rationale. BMC Nephrol 2013; 14: 197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ludlow MJ. et al. How Australian nephrologists view home dialysis: results of a national survey. Nephrology 2011; 16: 446–452 [DOI] [PubMed] [Google Scholar]
- 10. Jayanti A. et al. Home hemodialysis: beliefs, attitudes, and practice patterns. Hemodial Int 2014; 18: 767–776 [DOI] [PubMed] [Google Scholar]
- 11. Fluck RJ, Fouque D, Lockridge RS Jr.. Nephrologists’ perspectives on dialysis treatment: results of an international survey. BMC Nephrol 2014; 15: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jayanti A. et al. Technique survival in home haemodialysis: a composite success rate and its risk predictors in a prospective longitudinal cohort from a tertiary renal network programme. Nephrol Dial Transplant 2013; 28: 2612–2620 [DOI] [PubMed] [Google Scholar]
- 13. Phillips M. et al. An education initiative modifies opinions of hemodialysis nurses towards home dialysis. Can J Kidney Health Dis 2015; 2: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Partridge MR, Hill SR.. Enhancing care for people with asthma: the role of communication, education, training and self-management. 1998 World Asthma Meeting Education and Delivery of Care Working Group. Eur Respir J 2000; 16: 333–348 [DOI] [PubMed] [Google Scholar]
- 15. Lake AJ, Staiger PK.. Seeking the views of health professionals on translating chronic disease self-management models into practice. Patient Educ Couns 2010; 79: 62–68 [DOI] [PubMed] [Google Scholar]
- 16. Young HM. et al. Important, misunderstood, and challenging: a qualitative study of nurse’ and allied health professionals’ perceptions of implementing self-management for patients with COPD. Int J Chron Obstruct Pulmon Dis 2015; 10: 1043–1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Manns BJ. et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int 2005; 68: 1777–1783 [DOI] [PubMed] [Google Scholar]
- 18. Isnard Bagnis C. et al. Quality standards for predialysis education: results from a consensus conference. Nephrol Dial Transplant 2015; 30: 1058–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walker RC. et al. Patient and caregiver perspectives on home hemodialysis: a systematic review. Am J Kidney Dis 2015; 65: 451–463 [DOI] [PubMed] [Google Scholar]
- 20. Marshall MR, Chan CT. An open-source practical manual for home hemodialysis: a catalyst for change! Hemodial Int 2014; 18: 716–719 [DOI] [PubMed] [Google Scholar]
- 21. Bennett PN, Schatell D, Shah KD.. Psychosocial aspects in home hemodialysis: a review. Hemodial Int 2015; 19 (Suppl 1): S128–S134 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.