Abstract
Traumatic brain injury (TBI) can lead to changes in eating behavior patterns. This report describes the case of a patient with alcohol dependence presenting with behavioral changes and eating disorder following frontal lobe trauma. A 42-year-old male, premorbidly well-adjusted presented with alcohol use in dependent pattern for years. He sustained a subdural hematoma in the frontal lobe following a road traffic accident 10 years back. Post-TBI, the patient, started having low frustration tolerance, aggressive outbursts, disinhibition, difficulty in persisting with tasks, apathy, amotivation, and craving for food with inability to control intake on the sight of food. On testing, a deficit in frontal lobe functions was seen. Magnetic resonance imaging scan showed large areas of gliosis and encephalomalacia involving both frontal lobes with parenchymal loss. Eating disorders have been reported after TBI. This case report underscores a major role of frontal-subcortical circuits in regulation of eating habits.
Keywords: Behaviors, eating disorder, frontal-subcortical circuits, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is an insult to the brain that is caused by an external force. Neuropsychiatric disorders are probably the most frequent complication of TBIs. Associations between TBI and a variety of neuropsychiatric disorders have been described since the days of yore being referred to as “traumatic insanities”
TBI is associated with a gamut of psychiatric disorders that may be divided into disorders that are also seen in patients without brain injury such as substance abuse, mood, anxiety, psychotic, personality disorders, and those that are unique to patients with brain damage, for example, involuntary emotional expression disorder, anosognosia, aprosody, and neglect.
There are very few studies that have examined the interesting area of eating disorders after TBI.
Eating disorders are a persistent disturbance of eating behavior or behavior intended to control weight, which significantly impairs physical health or psychosocial functioning.[1] They comprise a spectrum of conditions, of which bulimia nervosa and anorexia nervosa are the major categories.
The etiology and pathogenesis of eating disorders per se are still highly debatable. In most patients of eating disorders, there is no detectable focal brain abnormality. Nonetheless, associations of anorexia and bulimia nervosa with a history of perinatal complications[2,3] and head injuries[4] suggest a role of cerebral pathology in some cases.
A number of case studies describe eating disorders with intracranial tumors, injuries, or epileptogenic foci. Literature reports isolated cases of anorexia, hyperphagia, and changes in food preferences.[5] The changes in dietary habits following TBI have generally been documented with respect to appetite,[6] and sensory disturbances of taste and/or smell.[7]
In a review of 54 published clinical cases of eating disorders in focal brain injuries, it was found that although simple changes in appetite and eating behavior occur with hypothalamic, and brain stem lesions, more complex syndromes, including characteristic psychopathology of eating disorders, are associated with right frontal and temporal lobe damage.[8]
In a sample of 120 patients with severe TBI, Ciurli et al (2011) found wide range of neuropsychiatric symptoms: apathy (42%), irritability (37%), dysphoria/depressed mood (29%), disinhibition (28%), eating disturbances (27%), and agitation (24%).[9] However morbid hunger or persistent hyperphagia (as seen in our patient) after TBI are rare but potentially life threatening conditions. Diagnostic review of 88 admitted patients of TBI identified 2 (3%) patients presenting with this condition.[10] In the following case report, we describe a patient with TBI (frontal lobe hematoma). He presented to us with changes in eating pattern that were characterized by an incessant urge to eat that was difficult to control on the sight of food. This case is unique because it is rare to develop hyperphagia after TBI. It also highlights the importance of cortical structures in the genesis of abnormal eating behaviors and challenges the conventional notion that only hypothalamus is responsible for regulating eating behaviors.
CASE REPORT
Mr. S, 42-year-old, Hindu, married, male, premorbidly well-adjusted presented with alcohol use in dependent pattern for 20 years. The patient met with a road traffic accident under intoxication 10 years back. He sustained a subdural hematoma which was evacuated by right frontotemporal trephine craniotomy. The patient also suffered from left hemiplegia following the craniotomy, which recovered partially with physiotherapy over a period of 1 year. Post head injury, the patient started having low frustration tolerance, aggressive outbursts, disinhibition, difficulty in persisting with tasks, apathy, and amotivation. Patient restarted with alcohol use in dependent pattern and also started reporting craving for food which was not present before. The patient would not be able to control his craving especially on the sight of food. On occasions, he would even snatch away food articles from his children. Corroboratory information was collected from his family members who had been cohabiting with the patient. They stated that he would eat his regular three meals a day, interspersed with a lot of snacking in between meal times which mostly included oily food, chips, biscuits, sodas, and the likes. If they tried to restrict him, he would have aggressive outbursts. Gradually, since the last 10 years, his eating pattern has consistently been deranged. Patient subjectively reported that even though he does not feel hungry, he could not control his urge to eat. At times, he even exhorted money from strangers giving various excuses, to obtain food. There was no history of eating inedible substances, polyuria, or polydipsia. In the last 1 year, patient's weight had increased from 78 kg to 108 kg.
Lobar function tests of the patient showed a deficit in frontal lobe and he was unable to do the clock draw test.
All laboratory investigations were within normal limits except high-density lipoprotein 34 mg/dL (normal value [N] ≥ 40 mg/dL), triglycerides 230 mg/dL (N < 150 mg/dL), fasting plasma glucose 119 mg/dL (N < 100 mg/dL), 2 h plasma glucose 201 mg/dL (N < 140 mg/dL), and HbA1c-6.9% (N < 5.6%).
Magnetic resonance imaging scan revealed large areas of damage involving both frontal lobes in the form of gliosis and encephalomalacia, along with diffuse cerebral atrophy [Figure 1a and b].
Figure 1.
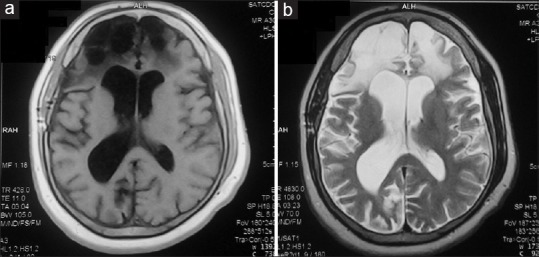
(a) T1 image and (b) T2 image showing large areas of gliosis and encephalomalacia seen involving both frontal lobes. There is evidence of parenchymal loss seen with dilation of both frontal horns. Diffuse prominence of the cerebral sulci is seen suggesting diffuse cerebral atrophy
On admission, alcohol withdrawal symptoms were managed with tapering doses of benzodiazepines. The patient was asked to make a food diary as a part of the self-monitoring activity. The patient was however not very honest with the same as he did not consider his eating to be a problem and would consume food secretly.
Endocrinology consultation and dietary advice were sought for his deranged blood glucose levels and he was started on metformin.
Taking into consideration his weight gain and alcohol intake he was also prescribed topiramate 100 mg along with amisulpride 200 mg to control the behavioral disturbances.
At discharge patient's blood glucose was within normal limits; however, there was no respite in his eating pattern. Educating the patient and engaging him in simple behavioral interventions is being planned for the follow-up visits.
DISCUSSION
In our case, it is clear that the onset of eating disorder was temporally correlated with trauma to the frontal lobe. Executive functions have been proposed to play an important role in regulating a wide array of behaviors and eating behavior has been proposed to be one of them.
Frontal-subcortical (FSC) circuits, in particular, are effector mechanisms that allow the organism to act in its environment. There are five major FSC circuits out of which three originate from dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex (ACC), orbitofrontal cortex (OFC). The prototypic FSC circuit is a closed loop that originates in the frontal cortex, projects onto the striatal structures (caudate, putamen, and ventral striatum), from striatum connects to substantia nigra (SN) and globus pallidus (GP), from these two structures connects to specific thalamic nuclei, from where it projects back to frontal cortex. Thus, striatum, SN, GP, and thalamus are the subcortical structures which are under the influence of frontal cortex. The DLPFC allows the organization of information to facilitate a response; the ACC is required for motivated behavior, and the OFC allows the integration of limbic and emotional information into behavioral responses. Impaired executive functions, apathy, and impulsivity are hallmarks of FSC circuit dysfunction[11] which was seen in our patient.
Eating disorders could be understood as forms of dysregulation of behavior that is suggestive of PFC dysfunction. Several research studies indicate that the PFC plays a pivotal role in the control of eating behavior. Prefrontal-subcortical networks regulate eating via connections with the hypothalamus. Various neuroimaging studies have also indicated that PFC, particularly OFC, plays an important role in the reinforcing value of food. With functional neuroimaging studies, hunger and satiety have been represented in prefrontal-subcortical systems and taste and olfactory processing in OFC. Eating behaviors are seen to be disturbed in various illnesses that involve prefrontal-subcortical systems. TBI can damage frontotemporal structures which can induce a lack of self-restraint in eating that is resistant to behavior modification and appetite suppressants[12] which was seen in our patient.
Literature also suggests that substance use and eating disorders can both be conceptualized as maladaptive impulsive and compulsive behaviors. The case discussed above suffered TBI on the background of alcohol dependence and further progressed on to develop dysregulated eating behavior. Thus, changes in eating habits, substance use and behavior following head trauma can be explained by involvement of frontal, prefrontal areas, and subcortical circuits. This challenges the traditional view that only hypothalamic disturbance underlies eating disorder and underscores the involvement of other brain areas and circuits that could be implicated in causation of eating disorders. Cortical lesions cause eating disorders, typically when located in temporal and frontal association areas that are strongly connected to basal and diencephalic systems controlling appetite.[13] Implication of frontotemporal circuits is consistent with functional neuroimaging research in eating disorders[14,15] and also with benign changes in eating, such as the Gourmand syndrome[13] described as a preoccupation with food and a preference for fine eating; it is a benign eating disorder associated with lesions involving parts of the right anterior cerebral hemisphere.
CONCLUSION
We, therefore, conclude that the current evidence favors cortical mechanisms in the genesis of eating disorders over hypothalamic ones. FSC circuits regulate behaviors and any illness or lesion involving them can trigger maladaptive behavior. More research is needed in this area as it could have importance not only in widening our understanding of the neurobiology of eating disorders but could also have therapeutic implications, thus improving management and long-term outcome of patients with eating disorders.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fairburn CG, Walsh BT. Atypical eating disorders (eating disorder not otherwise specified) In: Fairburn CG, Brownell KD, editors. Eating Disorders and Obesity: A Comprehensive Handbook. 2nd ed. New York: Guilford Press; 2002. pp. 171–7. [Google Scholar]
- 2.Cnattingius S, Hultman CM, Dahl M, Sparén P. Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch Gen Psychiatry. 1999;56:634–8. doi: 10.1001/archpsyc.56.7.634. [DOI] [PubMed] [Google Scholar]
- 3.Foley DL, Thacker LR, 2nd, Aggen SH, Neale MC, Kendler KS. Pregnancy and perinatal complications associated with risks for common psychiatric disorders in a population-based sample of female twins. Am J Med Genet. 2001;105:426–31. [PubMed] [Google Scholar]
- 4.Damlouji NF, Ferguson JM. Three cases of posttraumatic anorexia nervosa. Am J Psychiatry. 1985;142:362–3. doi: 10.1176/ajp.142.3.362. [DOI] [PubMed] [Google Scholar]
- 5.Castaño B, Capdevila E. Eating disorders in patients with traumatic brain injury: A report of four cases. NeuroRehabilitation. 2010;27:113–6. doi: 10.3233/NRE-2010-0586. [DOI] [PubMed] [Google Scholar]
- 6.Lewin J, Sumners D. Anorexia due to brain injury. Brain Inj. 1992;6:199–201. doi: 10.3109/02699059209029660. [DOI] [PubMed] [Google Scholar]
- 7.Schechter PJ, Henkin RI. Abnormalities of taste and smell after head trauma. J Neurol Neurosurg Psychiatry. 1974;37:802–10. doi: 10.1136/jnnp.37.7.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uher R, Treasure J. Brain lesions and eating disorders. Journal of Neurology, Neurosurgery & Psychiatry. 2005;76:852–7. doi: 10.1136/jnnp.2004.048819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciurli P, Formisano R, Bivona U, Cantagallo A, Angelelli P. Neuropsychiatric disorders in persons with severe traumatic brain injury: Prevalence, phenomenology, and relationship with demographic, clinical, and functional features. The Journal of head trauma rehabilitation. 2011;26:116–26. doi: 10.1097/HTR.0b013e3181dedd0e. [DOI] [PubMed] [Google Scholar]
- 10.Faruqui R, Rowell A. P02-54 Organic eating disorders of Morbid Hunger & Hyperphagia after traumatic brain injury (TBI): Presentation and prevalence. European Psychiatry. 2009;24:S744. [Google Scholar]
- 11.Cummings JL. Frontal-subcortical circuits and human behavior. Arch Neurol. 1993;50:873–80. doi: 10.1001/archneur.1993.00540080076020. [DOI] [PubMed] [Google Scholar]
- 12.Spinella M, Lyke J. Executive personality traits and eating behavior. Int J Neurosci. 2004;114:83–93. doi: 10.1080/00207450490249356. [DOI] [PubMed] [Google Scholar]
- 13.Regard M, Landis T. “Gourmand syndrome”: Eating passion associated with right anterior lesions. Neurology. 1997;48:1185–90. doi: 10.1212/wnl.48.5.1185. [DOI] [PubMed] [Google Scholar]
- 14.Gordon CM, Dougherty DD, Fischman AJ, Emans SJ, Grace E, Lamm R, et al. Neural substrates of anorexia nervosa: A behavioral challenge study with positron emission tomography. J Pediatr. 2001;139:51–7. doi: 10.1067/mpd.2001.114768. [DOI] [PubMed] [Google Scholar]
- 15.Uher R, Murphy T, Brammer MJ, Dalgleish T, Phillips ML, Ng VW, et al. Medial prefrontal cortex activity associated with symptom provocation in eating disorders. Am J Psychiatry. 2004;161:1238–46. doi: 10.1176/appi.ajp.161.7.1238. [DOI] [PubMed] [Google Scholar]


