Abstract
Heart disease comprises a wide class of cardiovascular abnormalities, including ischemic heart disease, myocardial infarction, atherosclerosis, and coronary artery disease. It is the leading cause of death all over the world. Several traditional and novel risk factors, such as infectious and noninfectious agents, have been associated with heart disease. Out of these, Helicobacter pylori has been recently introduced as an important etiological factor for heart disease. Numerous seroepidemiological findings observed H. pylori antibodies in the blood of a patient with cardiovascular complications. The bacteria survive in the epithelial cells of gastric organs and cause digestive complications. Excess inflammatory pathogenesis and prognosis stimulate an immune response that further causes significant disturbances in various factors like cytokines, fibrinogen, triglycerides, high density lipoprotein, C-reactive protein, heat shock protein, and white blood cell count, and provoke a number of problems such as atherosclerosis and prothrombic state, and cross-reactivity which eventually leads to heart diseases. H. pylori releases toxigenic nutrients, chiefly vacuolating cytotoxin gen A (Vac A) and cytotoxin associated gene A (Cag A), of which Cag A is more virulent and involved in the formation of cholesterol patches in arteries, induction of autoimmune disorder, and release of immune mediated response. Although numerous mechanisms have been correlated with H. pylori and heart disease, the exact role of bacteria is still ambiguous.
Keywords: atherosclerosis, cardiovascular diseases, heat shock protein, Helicobacter pylori, tumor necrosis factor
1. Introduction
Introduction of heart disease to the medical community has been a focus of debate, due to the continuously increasing rate of mortality in developed and developing countries.1, 2, 3 Heart diseases or cardiovascular diseases describe several heart disorders, including elevated blood pressure, coronary artery disease, and blockage of the arteries. A number of diseases related to the heart and blood vessels can come under the umbrella of heart.4 Diverse risk factors such as hypertension, increased lipid level, obesity, diet with high fat, physical inactivity, diabetes, and stress conditions are generally associated with it. Certain microorganisms such as Chlamydia pneumoniae, Cytomegalovirus, Epstein-Barr virus, human immunodeficiency virus, Herpes simplex, and Helicobacter pylori contribute in the development of heart diseases and are considered as risk factors and infectious.5, 6, 7, 8
H. pylori infection has been reported as an important cause of chronic gastrodigestive ulcers, however the epidemiological study based on discovery of bacteria during the past two decades has suggested that the higher prevalence of H. pylori infection might be involved in the pathogenesis of heart disease.9, 10, 11, 12, 13 In recent years, a theory has been proposed that a bacterium is one of the potential mechanisms that can cause direct and indirect effects on heart disease. Inflammatory and immunological events provoked by the H. pylori infection are the main underlying causes of the heart disease.14, 15, 16 The effect of infection on cardiovascular physiology can be direct and indirect. The direct effect includes endothelial injury, dysfunction through circulating endotoxins, smooth muscle proliferation, and local inflammation, whereas the indirect effect includes proinflammatory, hypercoagulability, atherogenic action, production of cross reactive antibodies, oxidation of low density lipoprotein, molecular mimicry, oxidative modification as well as nutrient/vitamin malabsorption and metabolic disturbances such as excess ammonia production.17, 18, 19, 20, 21, 22, 23 Recent studies suggested that a highly virulent strain of H. pylori [cytotoxin associated gene A (Cag A) strain] was more strongly associated with the risk of heart diseases which was confirmed by the presence of anti H. pylori antibodies through seroprevalence.24, 25 The objective of the present review is to highlight all possible mechanisms responsible for heart disease in relation with H. pylori infection.
1.1. H. pylori
The presence of a spiral-shaped bacterial microorganism was described by Professor W. Jaworski at Cracow in Jagiellonian University, Kraków, Poland. Later, Marshall and Warren27 cultured an organism from a gastritis patient which was not exactly the same as any previous species; it perhaps belonged to the Campylobacter genus, so they named it “pyloric campylobacter” which was later changed to Campylobacter pylori, and after that, it was named H. pylori due to its distinct morphogenic structural and genetic features. It has a heterogeneous morphology and normally it is present in a helicoidal, spiral, or curved shape, while in aged culture it is observed in coccoid form.26, 27, 28, 29, 30, 31, 32
H. pylori is a unipolar and microaerophilic bacterium. It contains five major outer membrane protein families. The largest family is putative adhesions whereas the other four families include porins, iron, transporters, flagellum-associated proteins, and proteins of unknown function. As it is a Gram-negative bacterium, its outer membrane consists of phospholipids and lipopolysaccharides and it also contains cholesterol glucosides, which are found in a few other bacteria. The high motility of the bacteria is due to the presence of two to six lophotrichous flagella. These sheathed flagellar filaments are composed of two copolymerized flagellins; flagellin A and flagellin B.33, 34, 35, 36, 37 They are about 0.5–1 mm in diameter and 2.5–5.0 mm long. They require about 5% oxygen (O2) and 5–10% carbon dioxide (CO2). H. pylori produces oxidase, catalase, and urease enzymes. The ability of the bacteria to survive in the harsh environment of the stomach is because of urease synthesis, a powerful enzyme which converts urea, a chemical made by stomach cells, to carbon dioxide and ammonia. This in turn creates a protective environment to the bacteria, by neutralizing acidity in the mucus surrounding the bacteria.38, 39, 40, 41, 42 The variability among strains of H. pylori is due to the availability of multiple bacterial genome sequences. It is one of the most genetically diverse species of bacteria, as it produces a wide range of toxins. Due to high virulent factors, it has been linked with many diseases. These virulent factors mainly include vacuolating cytotoxin gene A (Vac A) production and Cag A. About 50% of H. pylori strains produce Cag A which has been specifically linked to heart disease. These toxigenic nutrients of H. pylori cause inflammation to host cells and strong cellular damage, and rapidly stimulate host factors such as interleukins (ILs; IL-1, IL-2, IL-6, IL-8, and IL-12), interferon-gamma, tumor necrosis factor-α, T and B lymphocytes, and phagocytic cells, thereby increasing chances of heart disease.43, 44, 45, 46, 47, 48
1.2. Association between H. pylori and heart diseases
Several studies have ruled out and it has been suggested that H. pylori infection is not only linked to gastroduodenal conditions, but also extragastroduodenal conditions such as heart disease. The bacterial role in several diseases has been studied on the basis of serological surveillance.49, 50, 51, 52, 53, 54 Although these studies have too many biases, for the awareness of the people regarding this asymptomatic infection, a hypothesized theory has been made using epidemiological and pathological studies which might be responsible for heart disease.
H. pylori is one of the most widespread infections in the world. Although H. pylori infection is common, it is difficult to identify. The delayed diagnosis of infection exaggerates numerous problems, thus, epidemiological studies are generally preferred to recognize the incidence of H. pylori infection. Several studies have been executed for evaluating H. pylori incidences and prevalence, transmission of infection, and associated risk factors responsible for the infection. It has been evident that the prevalence of infection was erratic from region to region, between the socioeconomic and ethnic groups. Three main factors, namely rate of acquisition of infection (incidences), the rate of loss of infection; and prolonged prevalence of the bacterial infection and eradication are mainly responsible for H. pylori infection in the community.
The prevalence of infection is about 60–70% in adults and increases with age, while in children it is 20–30%. Its prevalence is greater in men than in women and many studies have shown that nonHispanic blacks and Hispanics are more prone to infection than the White population.55, 56, 57, 58, 59 The exact mode of H. pylori infection transmission is not clear, but several transmission mechanisms have been suggested such as direct transfer from person to person (via fecal-oral or oral-oral routes), epidemiological factors (food borne, water borne), and some zoonotic transmission (primates, domestic cats, and sheep). It is specifically seen in poorly sanitized people, in crowded living conditions, and with diminished hygiene.60, 61, 62, 63, 64, 65, 66, 67
2. Pathological mechanism
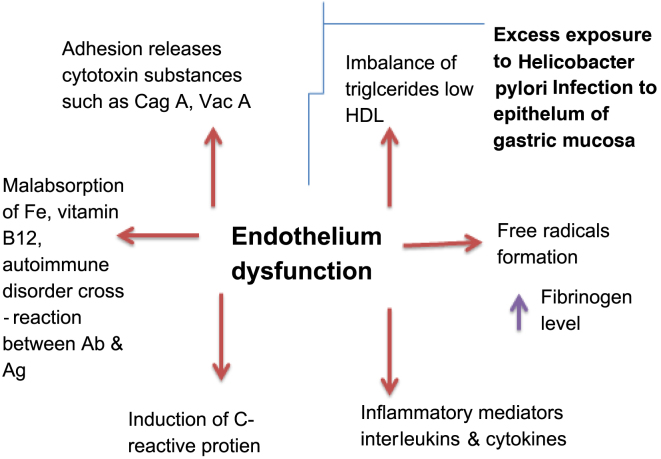
No single factor could account for infection related heart diseases, as the infection is a multifactorial process. Several potential mechanisms and pathways allied with H. pylori contribute in infection-induced cardiovascular complications. Fig. 1 briefly focuses on different mechanisms by which H. pylori contributes to heart diseases.
Fig. 1.
Helicobacter pylori infection induced immune response
HDL, high density lipoprotein.
Inflammation is a protective multistep process of the immune system. Repeated exposure to H. pylori infection leads to failure of the inflammation process and inability to combat progress of infectious agents, which leads to a number of diseases such as heart disease and cancer. This continuous over stress causes weakening of the body.68, 69, 70, 71, 72 Chronic stimulation of inflammatory responses due to bacterial infection in gut and gastric organs further produces induction of dyslipidemia, increases the levels of fibrinogen, stimulates release of C-reactive protein, escalates blood leukocytes and homocysteine, induces hypercoagulability, stimulates immune cross-reactivity, increases proinflammatory cytokines (ILs, lymphocytes) and other cytotoxic agents. This dramatic rise in the production of various proinflammatory and inflammatory metabolites affects blood vessel motility and provokes endothelial dysfunctioning, which results in blocking of arteries, thereby increasing the chances of heart attack. It has been reported that C-reactive protein is a potential indicator of disease associated with the heart and may play a crucial role in vessel mortality. Bacterial infection also enhances the release of IL-8, a small peptide (chemokine) secreted by various cell types, which serves as a potent inflammatory mediator recruiting and activating neutrophils such as T and B lymphocytes. Thus, chronic H. pylori infection results in disturbed immune response, which ultimately contributes to cardiovascular abnormalities including coronary artery diseases.73, 74, 75
Increased inflammation and cellular damage caused by adhesion of H. pylori infection in the body may increase the release of toxins such as Cag A and Vac A. Recently, it has been revealed that Cag A positive strain has been linked to H. pylori-associated heart disease more virulently than the Cag-A negative strain. It has been observed that Cag A strains enhance the activity of cycloxygenase-1 and -2 in vascular endothelial cells. Also, Cag A-induced inflammation may encourage the immune-mediated release of cytokines such as IL1–12, monocytes, macrophages (tumor necrosis factor α), and T and B lymphocytes, thereby causing heart disease or heart shock. Also, an autoimmune reaction could be postulated which includes cross-reactivity between anti-Cag A antibodies and vascular wall antigens, suggesting that these antibodies may contribute to the activation of inflammatory cells within atherosclerotic lesions.76, 77, 78, 79, 80
H. pylori infection exaggerates disturbances in the metabolism of lipid and lipoprotein. Triglyceride levels usually rise and the level of high density lipoprotein-cholesterol decreases. This could be due to the involvement of cytokines, especially tumor necrosis factor-α, which inhibits lipoprotein lipase and enhances free radical generation. This in turn facilitates the oxidation of low density lipoprotein, which is a key event in atherosclerosis. Free radicals also provoke activation of platelet and leukocyte chemotaxis, and might be responsible for thrombus formation. Increased release of various factors such as fibrinogen, C-reactive protein, tumor necrosis factor, IL-6, and white blood cell count might induce a prothrombotic state.81, 82, 83
Some studies revealed that H. pylori also decreases absorption of iron through reduction of the ferric to the ferrous form. Generally, this reaction is enhanced by ascorbic acid, but in the presence of H. pylori infection, decreases its concentration. It has been suggested that there is a competition between the bacteria and host for iron, as it is an essential element for growth. Thus, starvation of iron results in pernicious anemia, which further leads to the reduction in the number of circulating red blood cells, bleeding, and malabsorption of vitamin B12.84, 85
H. pylori burden contains a protein on the arterial cell surface that is similar to the heat shock protein-60 found in endothelial cells. Therefore, an immune response to H. pylori may induce immune cross-reaction between human and bacterial heat shock protein-60, which in turns leads to an autoimmune reaction and local inflammation of the artery.86 There is also speculation regarding the role of H. pylori in atherosclerotic plaque development, because some studies have found bacterial deoxyribonucleic acid in arterial plaques where it forms patches of infection, which results in heart disease.86
3. Conclusion
Infection of H. pylori bacteria infection is directly or indirectly involved in the development of cardiovascular diseases. Several serological based findings have revealed the active role of H. pylori in heart diseases. Activation of inflammatory mediators, proinflammatory factors, release of toxins, abnormal lipid metabolism, altered iron metabolism, and autoimmune reaction are the leading mechanisms of H. pylori, which contributes in cardiovascular anomalies. The chief leading role in the cause of heart disease is the improper functioning of the immune system, both at the cellular and systemic level. Most of these findings are based on serological findings. Further studies are needed to recognize the exact involvement of H. pylori in these diseases.
Conflicts of interest
We declare that we have no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the Dean and Director of the School of Pharmacy, Swami Ramanand Teerth Marathwada University, Nanded, Maharashtra, India for providing facilities for this review work.
References
- 1.Strachan D.P., Mendall M.A., Carrington D., Path F.R.C., Butland B.K., Yarnell J.W.G. Relation of Helicobacter pylori infection to 13-year mortality and incident ischemic heart disease in the caerphilly prospective heart disease study. Circulation. 1998;98:1286–1290. doi: 10.1161/01.cir.98.13.1286. [DOI] [PubMed] [Google Scholar]
- 2.Eskandarian R., Moosavi S., Babai M., Toussy J., Ghorbani R., Malek M. Impact of Helicobacter pylori on prognosis of patients with acute coronary syndrome. Arya J. 2006;1:164–169. [Google Scholar]
- 3.AL-Obeidy E.S., Saeed B.N. Helicobacter pylori in Iraq patient with ischemic heart disease. Fac Med Baghdad. 2011;53:29–31. [Google Scholar]
- 4.Braunwald E., Zipes D.P., Libby P. 6th ed. W.B. Saunders Company; Philadelphiya: 2001. Heart Disease: A Textbook of Cardiovascular Medicine; p. 031. [Google Scholar]
- 5.Torresa A.M., Gaensly M.M. Helicobacter pylori: A new cardiovascular risk factor. Rev Esp Cardiol. 2002;55:652–656. doi: 10.1016/s0300-8932(02)76673-6. [DOI] [PubMed] [Google Scholar]
- 6.Gillum R.F. Infection with Helicobacter pylori coronary heart disease, cardiovascular risk factors and systemic inflammation: The Third National Health and Nutrition Examination Survey. J Natl Med Assoc. 2004;96:1470–1476. [PMC free article] [PubMed] [Google Scholar]
- 7.Danesh J., Scholar R., Peto R. Risk factors of coronary heart disease infection with Helicobacter pylori: meta analysis of 18 studies. BMJ. 1998;316:1130. doi: 10.1136/bmj.316.7138.1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasceri V., Cammarota G., Patti G., Cuoco L., Gasbarrini A., Grillo R. Association of virulent Helicobacter pylori strains with ischemic heart disease. Circulation. 1998;97:1675–1679. doi: 10.1161/01.cir.97.17.1675. [DOI] [PubMed] [Google Scholar]
- 9.Folsom A.R., Nieto F.J., Sorlie P., Chambless L.E., Graham D.Y. Helicobacter pylori seropositivity and coronary Heart disease incidence. Circulation. 1998;98:845–850. doi: 10.1161/01.cir.98.9.845. [DOI] [PubMed] [Google Scholar]
- 10.Patel P., Mendall M.A., Carrington C., Strachan D.P., Leatham E., Molineaux N. Association of Helicobacter pylori and chlamydia pneumonia with coronary heart disease and cardiovascular risk factor. BMJ. 1995;311:711. doi: 10.1136/bmj.311.7007.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donagh T.A., Woodward M., Morrison C.E., McMurry J.J.V., Tunstall-Pedoe H., Lowe G.D.O. Helicobacter pylori infection and coronary heart disease in north Glasgow MONICA population. Eur Heart J. 1997;18:1257–1260. doi: 10.1093/oxfordjournals.eurheartj.a015436. [DOI] [PubMed] [Google Scholar]
- 12.Kowalski M., Pawlik M., Konturek J.W., Konturek S.J. Helicobacter infection in coronary artery disease. J Physiol Pharmacol. 2006;3:101–111. [PubMed] [Google Scholar]
- 13.Whincup P.H., Mendall M.A., Perry I.J., Strachan D.P., Walker M. Prospective relations between Helicobacter pylori infection, coronary heart disease, and stroke in middle aged men. Heart. 1996;75:568–572. doi: 10.1136/hrt.75.6.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mendall M.A., Goggin P.M., Molineaux N., Levy J., Toosy T., Strachan D. Relation of Helicobacter pylori infection and coronary heart disease. Br Heart J. 1994;71:437–439. doi: 10.1136/hrt.71.5.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gasbarrini A., Franceschi F., Armuzi A., Ojetti V., Candelli M., Torre E.S. Extradigestive manifestation of Helicobacter pylori gastric infection. Gut. 1999;45:112. doi: 10.1136/gut.45.2008.i9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee S.Y., Kim D.K., Son H.J., Lee J.H., Kim Y.H., Kim J.J. The impact of Helicobacter pylori infection on coronary heart disease in Korean Population. Korean J Gastroenterol. 2004;44:193–198. [PubMed] [Google Scholar]
- 17.Vafaeimanesh J., Hejazi S.F., Damanpak V., Vahedian M., Sattari M., Seyyedmajidi M. Association of Helicobacter pylori infection with coronary artery disease. Is Helicobacter pylori a risk factor. Scientific World Journal. 2014:1–6. doi: 10.1155/2014/516354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nozari Y., Akiash N., Daryani N.E., Abdollahi A. Association between Helicobacter pylori infection and atherosclerotic coronary artery disease. Iran J Pathol. 2009;4:1–4. [Google Scholar]
- 19.Ismail A., Khosravi H., Olson H. The role of infection in atherosclerosis and coronary heart disease; A new therapeutic target. Heart Dis. 1999;1:233–240. [PubMed] [Google Scholar]
- 20.Ellis R.W. Infection and coronary heart disease. J Med Microbial. 1997;46:535–539. doi: 10.1099/00222615-46-7-535. [DOI] [PubMed] [Google Scholar]
- 21.Ahmet A., Vardar R., Evrengul H., Ungan M., Yilmaz M., Payzin S. Does Helicobacter pylori infection have a role in coronary artery disease. Turk J Gastroenterol. 2001;12:287–293. [Google Scholar]
- 22.Manolakis A., Kapsoritakis A.N., Potamianos S.P. A review of postulated mechanisms concerning association of Helicobacter pylori with ischemic heart disease. Helicobacter. 2007;12:287–297. doi: 10.1111/j.1523-5378.2007.00511.x. [DOI] [PubMed] [Google Scholar]
- 23.Ei-Mashad N., El-Emshaty W.M., Arfat M.S., Koura B.A., Metwally S.S. Relation of Cag-A positive Helicobacter pylori strain and some inflammatory markers in patients with ischemic heart disease. Egypt J Immunol. 2009;16:39–47. [PubMed] [Google Scholar]
- 24.Gabriellie M., Santoliquido A., Cremonini F., Cicconi V., Candelli M., Serricchio M. Cag A-Positive cytotoxic H. pylori strains as a link between plaque instability and atherosclerotic stroke. Eur Heart J. 2004;25:64–68. doi: 10.1016/j.ehj.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Marshall B.J. History of discovery of C. pylori. In: Blaser M.J., editor. Campylobacter pylori in gastritis and peptic ulcer disease. Igaku Shoin; New York: 1989. [Google Scholar]
- 26.Kamangar F., Sheikhattari P., Mohebtash M. Helicobacter pylori and its effect on human health and disease. Arch Iran Med. 2011;14:192–199. [PubMed] [Google Scholar]
- 27.Marshall B.J., Warren J.R. Unidentified curved bacilli on gastric in active epithelium in active chronic gastritis. Lancet. 1983;1:1273–1275. [PubMed] [Google Scholar]
- 28.Graham D.Y., Uemura N. Natural history of gastric cancer after Helicobacter pylori eradication in Japan: after endoscopic resection, after treatment of the general population, and naturally. Helicobacter. 2006;11:139–143. doi: 10.1111/j.1523-5378.2006.00391.x. [DOI] [PubMed] [Google Scholar]
- 29.Konturek J.W. Discovery by Jaworski of Helicobacter pylori and its pathogenic role in peptic ulcer, gastritis and gastric cancer. J Physiol Pharmacol. 2003;54:23–41. [PubMed] [Google Scholar]
- 30.Marshall B.J., Warren J.R. Unidentified curved bacilli in the stomach of patent gastritis and peptic ulceration. Lancet. 1984;1:1311–1315. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 31.Yamoka Y. Caister Academic Press; Norflolk, UK: 2008. Helicobacter Pylori: Molecular genetics and cellular biology. [Google Scholar]
- 32.Goodwin C.S., Worsely B.W. Microbiology of Helicobacter pylori. Gastroenterol Clin North Am. 1993;22:5–19. [PubMed] [Google Scholar]
- 33.Mehmood A., Akram M., Shahab-uddin A.A., Usmanghani K., Hannan A., Mohiuddin E. Helicobacter pylori infection: An introduction. Int J Appl Biol Pharm. 2010;1:1337–1350. [Google Scholar]
- 34.Malfertheiner P., Megraud F., O’Morain C., Bazzoli F., El-Omar E., Graham D. Current European concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772–781. doi: 10.1136/gut.2006.101634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eaton K.A., Suerbaun S., Josenhans C., Krakowka S. Colonization of gnotobiotic piglets by Helicobacter pylori deficient in two flagellin genes. Infect Immun. 1996;64:2445–2448. doi: 10.1128/iai.64.7.2445-2448.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Josenhans C., Eaton K.A., Theventon T., Suerbaun S. Switching of flagellar motility in Helicobacter pylori by reversible length variation of a short homopolymeric sequence repeat in fliP, a gene encoding a basal body protein. Infect Immun. 2000;68:4598–4603. doi: 10.1128/iai.68.8.4598-4603.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sikandar K.S., Haider S.S., Kazmi S.U. Helicobacter pylori: Gastric ulcer and cancer causing burg. Int J Adv Res. 2013;1:399–405. [Google Scholar]
- 38.Kusters J.G., Vliet A.H., Kuipers E.J. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19:449–490. doi: 10.1128/CMR.00054-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rektorschek M., Weeks D., Sachs G., Melcher K. Influence of pH on metabolism and urease activity of Helicobacter pylori. Gastroenterology. 1998;115:628–641. doi: 10.1016/s0016-5085(98)70142-8. [DOI] [PubMed] [Google Scholar]
- 40.Konturek P.C., Konturek S.J., Bobrzynski A., Kwiecien N., Obtulowicz W., Stachura J. Helicobacter pylori and impaired gastric secretory functions associated with duodenal ulcer and atrophic gastritis. J Physiol Pharmacol. 1996;47:365–373. [PubMed] [Google Scholar]
- 41.Suerbaun S., Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175–1186. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 42.Ridker P.M., Danesh J., Youngman L., Collins R., Stampfer M.J., Peto R. A prospective study of Helicobacter pylori seropositivity and the risk for future myocardial infarction among socioeconomically similar U.S. men. Ann Intern Med. 2001;135:184–188. doi: 10.7326/0003-4819-135-3-200108070-00010. [DOI] [PubMed] [Google Scholar]
- 43.Pasceri V., Patti G., Cammarota G., Pristipino C., Richichi G., Di S.G. Virulent strains of Helicobacter pylori and vascular disease: a meta-analysis. Am Heart J. 2006;151:1215–1222. doi: 10.1016/j.ahj.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 44.Shuo Z., Yang G., Yan M.A., Yue T. Cytoxin-associated gana-A-seropositive virulent strains of Helicobacter pylori and atherosclerotic disease: a systemic review. Chin Med J. 2008;121:946–951. [PubMed] [Google Scholar]
- 45.Franceschi F., Niccoli G., Ferrente G., Gasbarrini A., Baldi A., Candelli M., Cag A. antigen of Helicobacter pylori and coronary instability: insight from a clinico-pathological study and meta-analysis of 4241 cases. Atherosclerosis. 2009;202:535–542. doi: 10.1016/j.atherosclerosis.2008.04.051. [DOI] [PubMed] [Google Scholar]
- 46.Atherton J.C. H. pylori Virulence factors. Br Med Bull. 1998;54:105–120. doi: 10.1093/oxfordjournals.bmb.a011662. [DOI] [PubMed] [Google Scholar]
- 47.Israel D.A., Salama N., Arnold C.N., Moss S.F., Ando T., Wirth H.P. Helicobacter pylori strain-specific differences in genetic content, identified by microarray, influence host inflammatory responses. J Clin Invest. 2001;107:611–620. doi: 10.1172/JCI11450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsang K.W., Lam S.K. Extragastroduodenal conditions associated with Helicobacter pylori infection. Hong Kong Med J. 1999;2:169–174. [PubMed] [Google Scholar]
- 49.Nilsson H., Pietroiusti A., Gabrielli M., Zocco M.A., Gasbarrini G., Gasbarrini A. Helicobacter pylori and extragastric disease and other Helicobacter. Helicobacter. 2005;10:54–65. doi: 10.1111/j.1523-5378.2005.00334.x. [DOI] [PubMed] [Google Scholar]
- 50.Sawayama Y., Ariyama I., Hamada M., Otaguro S., Machi T., Taira Y. Association between chronic Helicobacter pylori infection and acute ischemic stroke: Fukuoka Harasanshin Atherosclerosis Trial (FHAT) Atherosclerosis. 2005;178:303–309. doi: 10.1016/j.atherosclerosis.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 51.Strandberg T.E., Tilvis R.S., Vuoristo M., Lindroos M., Kosumen T.U. Prospective study Helicobacter pylori seropositivity and cardiovascular in a general elderly population. BMJ. 1997;314:1317–1318. doi: 10.1136/bmj.314.7090.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rogha M., Dadkhan D., Pourmoghaddas Z., Shirneshan K., Nikvarz M., Pourmoghaddas M. Association between Helicobacter pylori infection with severity of coronary heart disease. Arya Atherosclerosis. 2012;7:138–141. [PMC free article] [PubMed] [Google Scholar]
- 53.Rathorne B., Martin D., Stephens J., Thompson J.R., Samani N.J. Helicobacter pylori seropositivity in subjects with acute myocardial infarction. Heart. 1996;76:308–311. doi: 10.1136/hrt.76.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duynhoven Y.T.H.P., Jonge R.D. Transmission of Helicobacter pylori: A role for food. Bull World Health Organ. 2001;79:455–460. [PMC free article] [PubMed] [Google Scholar]
- 55.Pounder R.E. The prevalence of Helicobacter pylori infection in different countries. Aliment Pharmacol Ther. 1995;9:33–39. [PubMed] [Google Scholar]
- 56.Smoak B.L., Kelley P.W., Taylor D.N. Seroprevalence of Helicobacter pylori infections in a cohort of US Army recruits. Am J Epidemiol. 1994;139:513–519. doi: 10.1093/oxfordjournals.aje.a117034. [DOI] [PubMed] [Google Scholar]
- 57.Everhart J.E., Kruszon-Moran D., Perez G.I., Tralka T.S., McQuillan G. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis. 2000;181:1359–1363. doi: 10.1086/315384. [DOI] [PubMed] [Google Scholar]
- 58.Lynch N.A. Helicobacter pylori and ulcers: a paradigm revised. J Chron Dis. 1967;20:435–456. [Google Scholar]
- 59.Nouraie M., Latifi-Navid S., Rezvan H., Radmard A.R., Maghsudlu M., Zaer-Rezaii H. Childhood hygienic practice and family education status determine the prevalence of Helicobacter pylori infection in Iran. Helicobacter. 2009;14:40–46. doi: 10.1111/j.1523-5378.2009.00657.x. [DOI] [PubMed] [Google Scholar]
- 60.Safaei H.G., Rahim E., Rashidipour R. Helicobacter pylori as a zoonotic infection: the detection of H. pylori antigens in the milk and the faeces of cows. J Res Med Sci. 2011;16:184–187. [PMC free article] [PubMed] [Google Scholar]
- 61.Megraud F. Transmission of Helicobacter pylori: Faecal-oral versus oral-oral route. Aliment Pharmacol Ther. 1995;2:85–91. [PubMed] [Google Scholar]
- 62.Handt L.K., Fox J.G., Dewhirst F.E., Fraser G.J., Paster B.J., Yan L.L. Helicobacter pylori isolated from the domestic cat: Public Health implication. Infect Immun. 1994;62:2367–2374. doi: 10.1128/iai.62.6.2367-2374.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dore M.P., Sepulveda A.R., EI-Zimaity H., Yamaoka Y., Osato M.S., Mototsugu K. Isolation of Helicobacter pylori from sheep-implications for transmission to humans. AM J Gastroenterol. 2001;96:1396–1401. doi: 10.1111/j.1572-0241.2001.03772.x. [DOI] [PubMed] [Google Scholar]
- 64.Perry S., Delaluz S.M., Yang S., Haggerty T.D., Hurst P., Perez-Perez G. Gastroenteritis and transmission of Helicobacter pylori infection in households. Emerg Infect Dis. 2006;12:1701–1708. doi: 10.3201/eid1211.060086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hulten K., Han S.W., Enroth H., Klein P.D., Opekun A.R., Gilman R.H. Helicobacter pylori in the drinking water in Peru. Gastroenterology. 1996;110:1031–1035. doi: 10.1053/gast.1996.v110.pm8612990. [DOI] [PubMed] [Google Scholar]
- 66.Bellack N.R., Koehoorn M.W., MacNab Y.C., Morshed M.G. A conceptual model of water's role as a reservoir in Helicobacter pylori transmission: a review of the evidence. Epidemiol Infect. 2006;134:439–449. doi: 10.1017/S0950268806006005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mehta J.L., Saldeen T.G.P., Rand K. Interactive role of infection, inflammation and tradition risk factors in atherosclerosis and coronary artery disease. JACC. 1998;31:1217–1225. doi: 10.1016/s0735-1097(98)00093-x. [DOI] [PubMed] [Google Scholar]
- 68.Al-Soud A.A., Mostafa A.A., El-Sayed S., Mahmoud A. The role of Helicobacter pylori infection in patients with chest pain. MMJ. 2008;21:109–122. [Google Scholar]
- 69.Al-Obeidy E.S., Saeed B.N. Helicobacter pylori infection in Iraq patients with ischemic heart disease. Fac Med Baghdad. 2011;53:29–31. [Google Scholar]
- 70.Tarresa A.M., Gaensly M.M. A Helicobacter: A new cardiovascular risk factor. Rev Esp Cardiol. 2002;55:652–656. doi: 10.1016/s0300-8932(02)76673-6. [DOI] [PubMed] [Google Scholar]
- 71.Danesh J., Wheeler J.G., Hirschfield G.M., Eda S., Eiriksdottir G., Rumley A. C-reactive protein and other circulating markers of inflammation in the prediction of coronory heart disease. N Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 72.Vareki S.M., Zarkesh-Esfahani H., Behjati M. Helicobacter pylori's evasion of the immune system could establish an inflammatory environment that potentially induces the development of coronary artery disease. Jundishapur J Microbiol. 2013;6:243–247. [Google Scholar]
- 73.Ishida Y., Suzuki K., Taki K., Niwa T., Kurotsuchi S., Ando H. Significant association between Helicobacter pylori infection and serum C-reactive protein. Int J Med Sci. 2008;5:224–229. doi: 10.7150/ijms.5.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nabipour I., Vahadt K., Jafari S.M., Pazoki R., Sanjdideh Z. The association of metabolic syndrome Chlamydia pneumonia, Helicobacter pylori, cytomegalovirus, and herpes simplex virus type 1: The Persian Gulf Healthy Heart Study. Cardiovasc Diabetol. 2006;5:2840. doi: 10.1186/1475-2840-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kaloorazi N.A., Mohammadi M. Helicobacter pylori infection and extragastric diseases. J Biol Today's World. 2013;2:121–132. [Google Scholar]
- 76.Félétou M., Huang Y., Vanhoutte P.M. Endothelium-mediated control of vascular tone: COX1 & COX 2 products. Br J Pharmacol. 2011;164:894–912. doi: 10.1111/j.1476-5381.2011.01276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kaperonis E.A., Liapis C.D., Kakisis J.D., Dimitroulis D., Papavassiliou V.G. Inflammation and atherosclerosis. Eur Vasc J Endovasc Surg. 2006;31:386–393. doi: 10.1016/j.ejvs.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 78.Rasmi Y., Seyyed-Mohammadzad M. Frequency of Helicobacter pylori and cytotoxin associated gene A in patients with cardiac syndrome. J Cardiovasc Dis Res. 2012;3:16–21. doi: 10.4103/0975-3583.91597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Al-Quarashi A.M., Hodhod T.E. The association of Cag A-positive Helicobacter pylori and atherosclerosis in Najran area, Saudi Arabia. J Am Sci. 2013;9:356–361. [Google Scholar]
- 80.Shmuely H., Passaro D.J., Vaturi M., Sagie A., Pitlik S., Samra Z. Association of Cag A+ Helicobacter pylori with aortic atheroma. Atherosclerosis. 2005;179:127–132. doi: 10.1016/j.atherosclerosis.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 81.Aydemir S., Eren H., Tekin I.O., Harmandar F.A., Demircan N., Cabuk M. Helicobacter pylori eradication lowers serum asymmetric dimethylarginine levels. Mediators Inflamm. 2010;2010:1–4. doi: 10.1155/2010/685903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Faghihi A.H., Agah S., Fereshtehnejad S.M., Bahar M.A. Assessment of the relationship between serum fibrinogen level and Helicobacter pylori infection in patients with or without ischemic heart disease. Med J Islam Repub Iran. 2007;21:105–110. [Google Scholar]
- 83.Frostegard J. Immunity, atherosclerosis and cardiovascular disease. BMC Med. 2013;11:117. doi: 10.1186/1741-7015-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fernandez-Banares F., Monzon H., Forne M. A Short review of malabsorption and anaemia. World J Gastroenterol. 2009;15:4644–4652. doi: 10.3748/wjg.15.4644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jafarzadeh A., Nemati M., Tahmasbi M., Ahmadi P., Rezayati M.T., Sayadi A.R. The association between infection and infection burden in Iranian patients with acute myocardial infarction and unstable angina. Acta Med Indones. 2011;43:105–111. [PubMed] [Google Scholar]
- 86.Sulewska A., Modrzejewski W., Kovalchuk O., Kasacka I., Jackowski R., Hirnle T. Attempts to detect Helicobacter pylori in the atherosclerotic plaques. Rocz Akad Med Bialymst. 2004;49:239–241. [PubMed] [Google Scholar]