Figure 3.
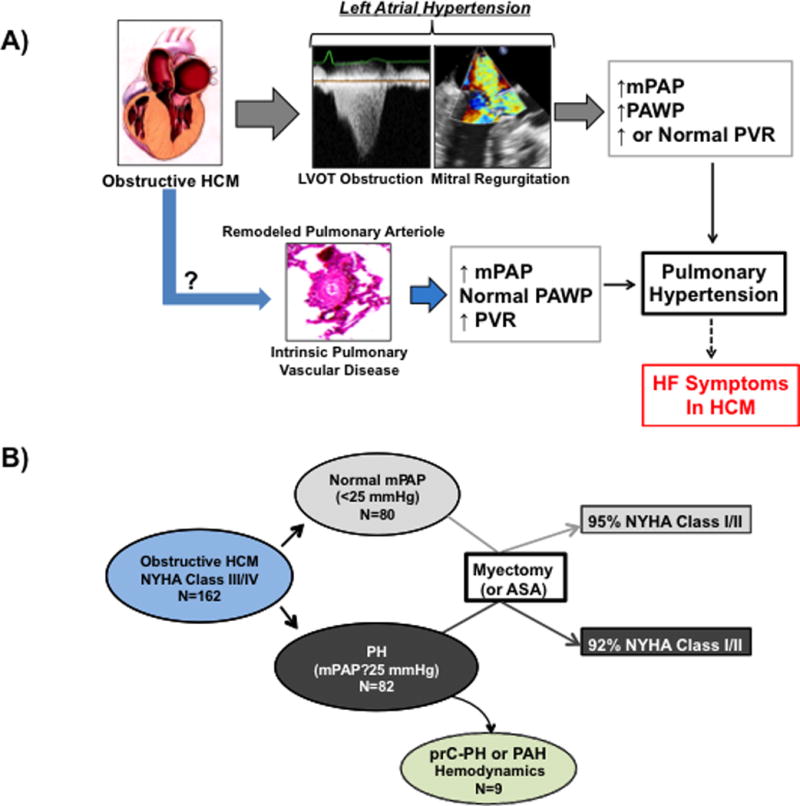
Pulmonary hypertension and the pathophysiology of heart failure symptoms in obstructive HCM. (A) Our findings suggest that in patients with obstructive HCM referred for septal reduction therapy, pulmonary hypertension is common and may be one pathophysiology underlying heart failure symptoms in this patient population. Analysis of invasive cardiopulmonary hemodynamics prior to surgical myectomy or alcohol septal ablation suggests that pulmonary hypertension is often associated with left atrial hypertension, which may be due to dynamic left ventricular outflow tract obstruction and mitral regurgitation. However, we also observed in some patients an increase in pulmonary artery pressure without left atrial hypertension or other cardiopulmonary diseases commonly associated with pulmonary hypertension, raising the possibility that intrinsic pulmonary vascular remodeling was present in this obstructive HCM patient subgroup. (B) A significant difference in clinical response to septal reduction therapy with surgical myectomy or alcohol septal ablation (ASA) was not observed in patients with preprocedural pulmonary hypertension compared to patients with normal preprocedural mean pulmonary artery pressure (mPAP). LVOT, left ventricular outflow tract; PAWP, pulmonary artery wedge pressure; PVR, pulmonary vascular resistance; HF, heart failure; NYHA, New York Heart Association; prC-PH, pre-capillary pulmonary hypertension; PAH, pulmonary arterial hypertension. The image of obstructive HCM was reproduced with permission from Nishimura RA, Ommen SR, Tajik AJ. Hypertrophic cardiomyopathy: A patient perspective. Circulation 2003;108:e133–e135.
