Abstract
INTRODUCTION
The 2012 British Association of Endocrine and Thyroid Surgeons audit report showed that only 86 of 1359 patients who underwent adrenalectomy had a bilateral operation; thus the experience with this procedure remains limited.
METHODS
Retrospective review of patients undergoing bilateral adrenalectomy in a tertiary referral centre.
RESULTS
Between November 2005 and January 2016, bilateral adrenalectomy was performed in 23 patients (6 male, 17 female, age 43 ± 4 years) diagnosed with Cushing’s disease (n = 13), hereditary phaeochromocytomas (n = 6), adrenocortical cancer (n = 2), colorectal metastatic disease (n = 1) and adrenocortical adenomas (n = 1).
A laparoscopic transperitoneal approach was used in 17 patients, with one conversion to open. Three patients had open adrenalectomies for adrenocortical cancer and for simultaneous phaeochromocytomas and pancreatic neuroendocrine tumours in a patient with Von Hippel-Lindau syndrome. Three patients with Cushing’s had a bilateral retroperitoneoscopic operation. The mean operating time was 195 ± 16 minutes for laparoscopic operations (n = 16), 243 ± 44 minutes for open adrenalectomies (n = 4) and 151 ± 12 minutes for retroperitoneal operations. It was significantly shorter for Cushing’s disease than for phaeochromocytomas (162 ± 8 vs. 257 ± 39 minutes, P < 0.01).
Median length of hospital stay was 5 days. Postoperative complications (Clavien-Dindo classification) included one chest infection (level 2), one postoperative haemorrhage and two chest drains for pneumothorax (level 3), two postoperative cardiac arrests (level 4) and one late cancer death from complications related to uncontrolled hypercortisolism (level 5).
DISCUSSION
Synchronous bilateral adrenalectomy remains an infrequent operation. The laparoscopic approach is feasible in the majority of patients. It is likely that the retroperitoneoscopic adrenalectomy will become the standard approach for bilateral operations.
Keywords: Adrenalectomy, Bilateral, Laparoscopic, Retroperitoneal
Introduction
Adrenalectomy remains a rarely encountered operation in most surgical centres. An analysis of 3144 cases operated in the USA over a decade showed that, in 2005, adrenalectomies represented only 14 of 100,000 discharges, with high-volume surgeons being defined as those doing over 4 cases/year and high-volume centres operating over 14 cases/year.1 Similarly, analysis of 7829 patients recorded in the nationwide inpatient sample between 2003 and 2009 concluded that high-volume surgeons were those who operated over five cases/year.2 The vast majority of patients captured in these statistics underwent unilateral adrenalectomy, bilateral operations representing only a small minority. Data describing the provision of adrenalectomy within the National Health Service in the UK are currently being prepared for publication and the only information available to date reflects the activity of surgeons who are members of the British Association of Endocrine and Thyroid Surgeons (BAETS) whose workload has been reported in the 2012 audit.3
Synchronous bilateral adrenalectomy (SBA) is one of the rarest operation performed worldwide because of its indications are restricted to the small number of patients with bilateral phaeochromocytomas and those with adrenocorticotropic hormone (ACTH)-dependent hypercortisolism, most commonly after failed pituitary surgery. The BAETS 2012 audit showed that only 86 of 1359 patients (6%) who underwent adrenalectomy had a bilateral operation.4
Laparoscopic unilateral adrenalectomy was initially reported in 19925 and within the last two decades has become the standard of care for benign adrenal tumours. It has been widely adopted because of its decreased morbidity and perioperative complications compared with the open approach. In recent years there has been increasing enthusiasm about learning the retroperitoneoscopic approach for adrenalectomy. This was first described in mid 1990s by Martin Walz from Essen, Germany,6 but many surgeons have been reluctant to adopt it because of their own lack of familiarity with a retroperitoneal approach.7 The different techniques have been applied for bilateral adrenalectomy but the optimal surgical approach has yet to be defined.
Before 2000, the two-staged laparoscopic adrenalectomy was used for patients with bilateral adrenal disease because of concerns about perioperative comorbidities and/or postoperative adrenal insufficiency. With an increasing number of patients with bilateral disease and the development of endocrine management of these patients, SBA has been performed on increasing number of selected patients with ACTH-dependent Cushing’s syndrome (i.e. Cushing’s disease or ectopic ACTH syndrome) or bilateral phaeochromocytomas.
The aim of the present study was to report a single-centre experience with simultaneous bilateral adrenalectomy and to evaluate its safety, surgical outcomes and potential indications of the procedure.
Materials and Methods
Patients who underwent adrenal surgery in a tertiary referral centre between 2005 and 2015 were identified from hospital records and a departmental database. Demographic details, clinical and operative data were analysed only for patients who underwent SBA. Postoperative complications were graded according to the Clavien–Dindo classification.8
Data were collected retrospectively and analyzed using a specifically designed spreadsheet (Microsoft Excel, Microsoft Corporation, Redmond, WA). Statistical analysis was performed on parametric data using the student’s t-test. A P value of < 0.05 was considered significant.
Results
Between November 2005 and January 2016, among 238 consecutive patients who had surgery for adrenal disease, 23 (10.1%) underwent SBA (Fig 1); 6 male and 17 female. Mean age was 43 ± 4 years (range 12–74 years). The indication for surgery is summarized in Table 1.
Figure 1.
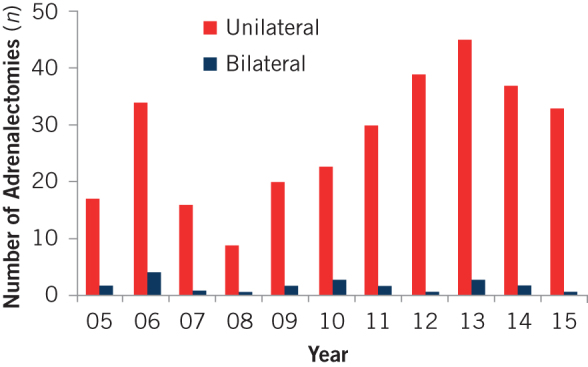
Patients who underwent adrenalectomy between 2005 and 2015 (n = 238)
Table 1.
Clinical and operative data
| Incidence | ||
|---|---|---|
| (n) | (%) | |
| Preoperative diagnosis | ||
| Cushing’s disease | 13 | 56.5 |
| Pheochromocytomaa | 6 | 26.1 |
| Adrenocortical carcinoma | 2 | 8.7 |
| Adrenocortical adenomas (MEN 1) | 1 | 4.3 |
| Metastatic colonic adenocarcinoma | 1 | 4.3 |
| Surgical approach | ||
| Open | 4 | 17.4 |
| Transperitoneal laparoscopic | 16 | 69.6 |
| Posterior retroperitoneoscopic | 3 | 13.0 |
MEN = multiple endocrine neoplasia
a3 patients with MEN 2A, 3 patients with VHL syndrome
Three patients had open bilateral adrenalectomy after being diagnosed with adrenocortical cancer with bilateral adrenal tumours (n = 2) and in a 12-year-old boy with Von Hippel-Lindau (VHL) syndrome with simultaneous bilateral phaeochromocytomas and pancreatic neuroendocrine tumours. Transperitoneal laparoscopic bilateral adrenalectomy (TL-BA) was performed in 17 patients; 3 patients had a posterior retroperitoneoscopic bilateral adrenalectomy (PR-BA).
Mean operating time was shortest for the retroperitoneal operations (151 ± 12 minutes) and longest for the open operations (243 ± 44 minutes) but statistical analysis was deemed inappropriate, as the selection of patients for each approach was biased; the mean operating time for TL-BA was 192 ± 15 minutes. Operating time for patients with Cushing’s syndrome was significantly shorter than for those with phaeochromocytoma (162 ± 8 minutes vs. 257 ± 39 minutes, P < 0.01). In the TL-BA group, conversion to an open procedure was required in one case (4.5%) because of bleeding from inferior vena cava during dissection of the right adrenal (left laparoscopic adrenalectomy was performed initially in the same patient and the laparoscopic operation was converted to open on the right side).
The average length of hospital stay was 8.8 days and the median length was 5.0 days (interquartile range, IQR, 4–6.5 days). Postoperative complications, categorised according to Clavien-Dindo, included chest infection, postoperative haemorrhage and chest drains for pneumothorax, postoperative cardiac arrests and one late cancer death on postoperative day 37 from complications related to uncontrolled hypercortisolism due to multiple liver metastases (Table 2). The morbidity rate was 26.1% and the mortality was 4.3%.
Table 2.
Complications (Clavien-Dindo classification)
| Grade | Description | Complication | Incidence | |
|---|---|---|---|---|
| (n) | (%) | |||
| I | Any deviation from normal postoperative course without need for pharmacological treatment or other intervention | – | – | |
| II | Requiring pharmacological treatment | Chest infection | 1 | 4.5 |
| III | Requiring surgical, endoscopic or radiological intervention | Postoperative haemorrhagePneumothorax (chest drain) | 32 | 4.59.1 |
| IV | Life-threatening complication requiring intensive care | Postoperative cardiac arrest (asystole from heart block) | 2 | 9.1 |
| V | Death of patient | Death 40 days postoperatively | 1 | 4.5 |
Discussion
We report a good outcome in a group of 23 patients who had synchronous bilateral total adrenalectomy and reinforce the reassurance provided by previous papers describing favourable outcomes and improved quality of life after bilateral adrenalectomy.9–11 In the past, some investigators questioned whether partial adrenalectomy should be performed for patients with bilateral disease. This was because of concerns related to the management of patients rendered ‘adrenal free’ and the fear of severe hypoadrenalism encouraged some to propose partial bilateral adrenalectomy. Currently, subtotal adrenalectomy is considered a reasonable option only for bilateral phaeochromocytomas in familial syndromes,12 but it is contraindicated for patients with ACTH-dependent hypercortisolism because of the high risk of disease recurrence. For these reasons, all patients in this series underwent total adrenalectomy.
Over the past two decades, the surgical technique for SBA has shifted from open to laparoscopic to retroperitoneoscopic adrenalectomy. Historically, open bilateral adrenalectomy was largely associated with a high rate of surgical complications, including intraoperative and postoperative bleeding (22%), incisional hernia (10%) and wound healing impairment (13.5%) in addition to general complications.13 Laparoscopic adrenalectomy was initiated by Michel Gagner in 199214 and it was soon established as the standard procedure for the surgical treatment of patients with unilateral adrenal diseases. The experience with laparoscopic SBA was slower to be reported and was found to have higher rate of complications compared with unilateral laparoscopic adrenalectomy,15,16 but the overall benefits became easily apparent. Several large series of laparoscopic SBA included 30 patients17 and 68 patients18 reported positive outcomes and found that the procedure was safe and effective. In this context, laparoscopic SBA was initiated in our centre in early 2000 and the outcomes reported in this paper compare well with data published to date.
As an alternative to the laparoscopic transperitoneal approach, in 1996 Martin Walz proposed the retroperitoneal approach for adrenalectomy as a potentially better option for patients with smaller tumours, lower body mass index and previous abdominal surgery.19 Although he remains the surgeon with by far the largest experience in adrenalectomy, even in his practice, bilateral cases remain a small minority, with only 19 of 560 patients presenting with bilateral disease.20 Despite the disadvantage of having a limited working area, which makes this procedure technically more demanding, the retroperitoneal approach is now widely accepted as a fast and safe operation, with the additional benefit for bilateral operations of avoiding the need for repositioning during the procedure. Mentoring from Martin Walz has encouraged many surgeons to adopt this technique and, in the past few years, three centres in the UK have started to offer retroperitoneoscopic adrenalectomy.
Few recent studies have compared the laparoscopic and retroperitoneoscopic approaches for unilateral adrenalectomy through comparative studies and meta-analysis has failed to demonstrate any significant advantage of one technique over the other.21–23 Two case series compared SBA and found no significant advantages or disadvantages for either technique: Miccoli et al.21 compared the lateral transperitoneal and the retroperitoneal technique, while Raffaelli et al.22 compared transabdominal laparoscopic, simultaneous posterior retroperitoneoscopic and robot-assisted approach. It is likely therefore that the choice between laparoscopic lateral transabdominal versus posterior retroperitoneal approach will be based on individual surgeon’s preference,23 and the small number of cases will make it impossible to compare the two techniques through a randomized trial.
In our experience, the lateral transperitoneal approach was used in the majority of patients (77%), an open approach was chosen for patients with large adrenocortical cancers and the posterior retroperitoneoscopic approach was used only for the most recent three patients in this series during 2015. This pattern reflects the changes in surgical technique described above.
Irrespective of the surgical approach, SBA remains an operation with potential morbidity related to the metabolic effect of hypercortisolism, the main presenting problem for most patients who need SBA. Historically, SBA performed by open laparotomy was associated with a high morbidity of 40% and a mortality rate of 5.6%.24 Takata et al.15 reported a 2.4% mortality rate and 13% complications rate after laparoscopic SBA, with infectious and thromboembolic events comprising 41% and 18% of the complications, respectively. A recent review by Ritzel et al.25 analyzed the outcome of 23 studies (739 patients) who underwent SBA, including 426 open and 313 laparoscopic approaches. Surgical outcome was similar between the procedures, as surgery-related 30-day mortality ranged from 0% to 15% and from 0% to 8% for open and laparoscopic procedures, respectively. The laparoscopic approach resulted in lower morbidity (internal and incisional complications), blood loss, anaesthesia exposure and inpatient hospital days, compared with the open approach. Hence, a laparoscopic approach was used for the majority of patients, with conversion to an open procedure necessary in a small subset of cases.
The latest published BAETS report showed that the overall average postoperative stay for 600 patients who underwent adrenal surgery was 5.5 days. In view of the small number of bilateral operations recorded in the audit, there was no figures provided for such cases.3 In this context, the postoperative stay of the group of patients reported in our series was favourable (the average was 8.8 days and the median was 5.0 days). The main reason for delay was to ensure that patients returned to normal oral intake and were able to tolerate oral steroid replacement before being discharged home. In our cohort of patients, the rate of complications was comparatively lower (Table 1). The overall morbidity rate compares favourably with some other reports.
There are some limitations to the present study. First, this is non-randomized study of consecutive, unselected patients. A randomized trial in this field is deemed unreasonable as the surgical approach is determined based on clinical characteristics of each patient and the heterogeneity of the group makes it impossible to randomise. Second, the present study comprised a relatively small number of patients. Until a complete restructuring of the service provision for adrenalectomy in the NHS is established, there is no mechanism to increase significantly the workload of established surgical centres.
Conclusions
In conclusion, a minimally invasive approach to bilateral adrenalectomy is safe and effective for the treatment of a subset of patients at high risk of perioperative complications. The present study confirms that SBA using the different surgical approaches is feasible and safe and that the retroperitoneoscopic approach will be increasingly considered the most convenient approach for patients needing bilateral adrenalectomy for Cushing’s disease.
References
- 1.Park HS, Roman SA, Sosa JA. Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch Surg 2009; : 1,060–1,067. [DOI] [PubMed] [Google Scholar]
- 2.Hauch A, Al-Qurayshi Z, Kandil E. Factors associated with higher risk of complications after adrenal surgery. Ann Surg Oncol 2015; : 103–110. [DOI] [PubMed] [Google Scholar]
- 3.British Association of Endocrine and Thyroid Surgeons. Fourth National Audit Report 2012. Henley-on-Thames: Dendrite Clinical Systems Ltd. [Google Scholar]
- 4.Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing s syndrome and pheochromocytoma. N Engl J Med 1992; : 1003. [DOI] [PubMed] [Google Scholar]
- 5.Walz MK, Peitgen K, Hoermann R et al. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg 1996; : 769–774. [DOI] [PubMed] [Google Scholar]
- 6.Constantinides VA, Christakis I, Touska P et al. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg 2012; : 1,639–1,648. [DOI] [PubMed] [Google Scholar]
- 7.Dindo D, Demartines N, Clavien PA. Classification of surgical complications. A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; : 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong A, Eloy JA, Liu JK. The role of bilateral adrenalectomy in the treatment of refractory Cushing s disease. Neurosurg Focus 2015; : E9. [DOI] [PubMed] [Google Scholar]
- 9.Reincke M, Ritzel K, Oßwald A et al. A critical reappraisal of bilateral adrenalectomy for ACTH-dependent Cushing s syndrome. Eur J Endocrinol 2015; : M23–M32. [DOI] [PubMed] [Google Scholar]
- 10.Kawasaki Y, Ishidoya S, Kaiho Y et al. qLaparoscopic simultaneous bilateral adrenalectomy: assessment of feasibility and potential indications. Int J Urol 2011; : 762–767. [DOI] [PubMed] [Google Scholar]
- 11.Castinetti F, Taieb D, Henry JF et al. Management of endocrine disease: outcome of adrenal sparing surgery in heritable pheochromocytoma. Eur J Endocrinol 2016; : R9–R18. [DOI] [PubMed] [Google Scholar]
- 12.Shen WT, Grogan R, Vriens M et al. One hundred two patients with pheochromocytoma treated at a single institution since the introduction of laparoscopic adrenalectomy. Arch Surg 2010; : 893–897. [DOI] [PubMed] [Google Scholar]
- 13.O Riordain DS, Farley DR, Young WF et al. Long term out-come of bilateral adrenalectomy in patients with Cushing s syndrome. Surgery 1994; : 1,088–1,093. [PubMed] [Google Scholar]
- 14.Yadav K, Bakshi G, Prakash G et al. Simultaneous bilateral laparoscopic adrenalectomy for pheochromocytoma in multiple endocrine neoplasia (MEN) syndrome: case report with review literature. Int J Surg Case Rep 2014; : 487–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takata MC, Kebebew E, Clark OH et al. Laparoscopic bilateral adrenalectomy: results for 30 consecutive cases. Surg Endosc 2008; : 202–207. [DOI] [PubMed] [Google Scholar]
- 16.Chow JT, Thompson GB, Grant CS et al. Bilateral laparoscopic adrenalectomy for corticotrophin-dependent Cushing s syndrome: a review of the Mayo clinic experience. Clin Endocrinol 2007; : 513x2013;519. [DOI] [PubMed] [Google Scholar]
- 17.Walz MK, Alesina PF, Wenger FA et al. Posterior retroperitoneoscopic adrenalectomy: results of 560 procedures in 520 patients. Surgery 2006; : 943–948. [DOI] [PubMed] [Google Scholar]
- 18.Lombardi CP, Raffaelli M, De Crea C et al. Endoscopic adrenalectomy: is there an optimal operative approach? Results of a single-center case–control study. Surgery 2008; : 1,008–1,014. [DOI] [PubMed] [Google Scholar]
- 19.Constantinides VA, Christakis I, Touska P et al. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg 2012; : 1,639–1,648. [DOI] [PubMed] [Google Scholar]
- 20.Nigri G, Rosman AS, Petrucciani N et al. Meta-analysis of trials comparing laparoscopic transperitoneal and retroperitoneal adrenalectomy. Surgery 2013; : 111–119. [DOI] [PubMed] [Google Scholar]
- 21.Miccoli P, Materazzi G, Brauckhoff M et al. No outcome differences between a laparoscopic and retroperitoneoscopic approach in synchronous bilateral adrenal surgery. World J Surg 2011; : 2,698–2,702. [DOI] [PubMed] [Google Scholar]
- 22.Raffaelli M, Brunaud L, De Crea C et al. Synchronous bilateral adrenalectomy for Cushing s syndrome: laparoscopic versus posterior retroperitoneoscopic versus robotic approach. World J Surg 2014; : 709–715. [DOI] [PubMed] [Google Scholar]
- 23.Ramacciato G, Nigri GR, Petrucciani N et al. Minimally invasive adrenalectomy: a multicenter comparison of transperitoneal and retroperitoneal approaches. Am Surg 2011; : 409–416. [PubMed] [Google Scholar]
- 24.Gumbs AA, Gagner M. Laparoscopic adrenalectomy. Best Pract Res Clin Endocrinol Metab 2006; : 483–499. [DOI] [PubMed] [Google Scholar]
- 25.Ritzel K, Beuschlein F, Mickisch A et al. Clinical review: outcome of bilateral adrenalectomy in Cushing s syndrome: a systematic review. J Clin Endocrinol Metab 2013; : 3,939–3,948. [DOI] [PubMed] [Google Scholar]


