Figure 2.
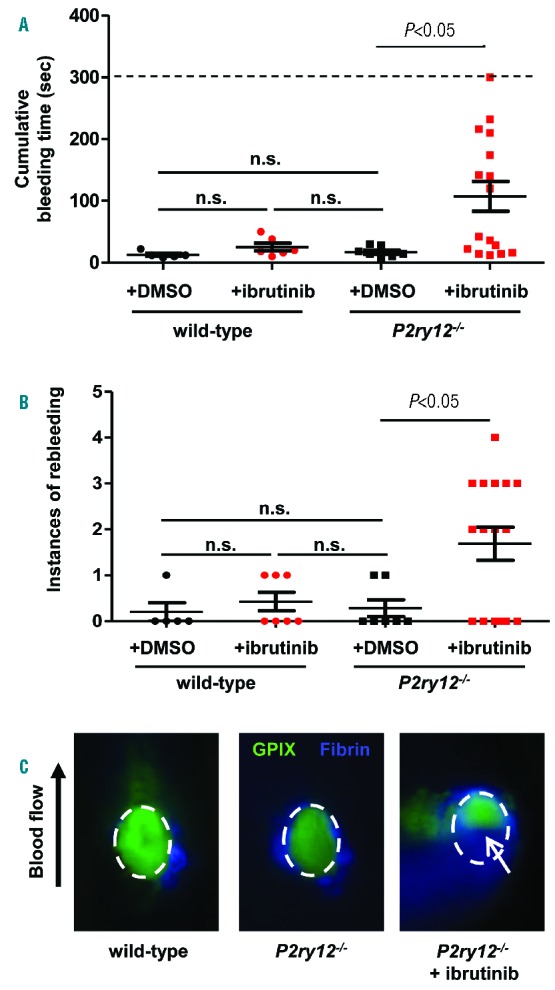
Ibrutinib impairs primary hemostasis in the presence of additional platelet defects. To assess hemostasis, bleeding time was determined using the saphenous vein laser injury model developed in our lab.11 Mice were anesthetized and the saphenous vein exposed. Before injury, mice received an injection of anti-GPIX-AlexaFluor488 and anti-fibrin-AlexaFluor647 antibodies. The saphenous vein was then injured and the injury site was recorded for 5 minutes. A) Cumulative bleeding time was determined by the amount of time blood could be seen flowing from the injury site, including both the bleeding time following initial injury and during injury rebleeding. The dashed line indicates the maximum bleeding time, which was only achieved in one injury site in a P2ry12−/− mouse treated with ibrutinib. n.s. = not statistically significant. B) The number of rebleeds, or injury re-openings, per injury site following occlusion of the initial injury. n.s. = not statistically significant. C) Platelet and fibrin accumulation was observed at the site of laser injury. Wild-type mice quickly occluded the injury site and robust platelet accumulation was observed within the first minute, after which loosely-adhered platelets began to embolize and the platelet plug stabilized. In P2ry12−/− mice, the vascular lesion occluded in a time frame comparable to wild-type mice. However, the peak of platelet accumulation was lost, and rebleeding occurred in several mice. In P2ry12−/− mice treated with ibrutinib, the cumulative bleeding time was significantly increased (Fig 2A), and a significant number of rebleedings occurred (Fig 2B), which were visually observed by blood flowing from the injury site (white arrow). In this study, P2ry12−/− mice were used as their own control; mice were injured at 1–2 sites, followed by ibrutinib administration, and then subjected to 2–3 more injuries at upstream sites along the saphenous vein.
