Abstract
Background
One of the services that plants provide for human beings is their wider medicinal application. Although it is not fully assessed, the practice and wider use of traditional medicine is frequent in Ethiopia. Studies conducted previously are confined to the perceptions of modern and traditional health practitioners about traditional medicine. A total of 45 informants were selected purposefully from the study area. For collecting the data, semi-structured interviewees, observation and field walks were employed from August 10 to September 30/2014. To summarize the information, descriptive statistical methods were applied.
Results
Sixty species of medicinal plants distributed in 42 families were collected and identified applied locally for the treatment of 55 human disorders. The most commonly treated ones were evil eye, malaria, wound, peptic ulcer disease and rabies. According to this study, leaves were the commonly used plant parts (36.5%) and 39% of the preparations were decoctions. Oral route, 43 (44%) was the commonly used route of application whereas most (54.8%) remedies were administered only once. Fourteen percent of preparations caused vomiting in addition most (40.4%) of the formulations was contraindicated for pregnant patients. Only seventeen percent of the formulations possessed drug food interactions. Most preparations were stored within clothes, 31 (29.8%). There exists a high (ICF = 0.8) evenness of plant use among healers for treating respiratory problems. Alliumsativum (FI = 0.75) for evil eye, Phytolacca dodecandra (FI = 0.8) for rabies and Croton macrostachyus (FI = 0.78) for treating malaria were medicinal plants with highest fidelity levels showing consistency of knowledge on species best treating power. This study also documented that drought, overgrazing and firewood collection are major threats.
Conclusion
Dega Damot district is loaded in its medicinal plant diversity and indigenous knowledge though plants are highly affected by drought, overgrazing and firewood collection. Therefore awareness activities must be created among the district’s population by concerned governmental and nongovernmental organizations about the value of medicinal plants and conservation of these plants. The healing potential and associated adverse issues of the claimed medicinal plants should be assessed before proposing for a broader utilization.
Electronic supplementary material
The online version of this article (doi:10.1186/s13104-017-2482-3) contains supplementary material, which is available to authorized users.
Keywords: Medicinal plants, Traditional medical practitioner, Ethnopharmaclogy
Background
According to world health organization, traditional medicine (TM) is the sum total of the knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures and nations. It is used in the maintenance of health, prevention, diagnosis, or treatment of disorders [1, 2]. Under TM, health practices, remedies, approaches, and beliefs incorporating plant, animal and mineral products, spiritual therapies are all included [3]. Traditional medicine is popular in the developing world and its use is rapidly spreading in the developed nations. In China, traditional herbal preparations account for 30–50% of the total drug consumption. In Ghana, Mali, Nigeria and Zambia, the first choice for 60% of children with high fever resulting from malaria is the use of herbal medicines. In Ethiopia up to 80% of the population uses TM due to the cultural acceptability of healers and local pharmacopeias, the relatively low cost of TM and difficult access to modern health facilities [4].
In Ethiopia, TM plays both preventive and curative roles. Vegetables are the abundant sources of traditional remedies. Various parts of plants like leaves, flowers, seeds, bark, sap and roots are used. Honey, butter, and sheep fat are TM sources from animals. In Ethiopia, traditional medical practitioners put much emphasis on the supernatural force as a source of wisdom for healing various illnesses. Even though practitioners practically deal with tangible problems like bone setting, simple traditional surgery, historical evidence shows that there were many prayers for the prevention and cure of various ailments [1, 5–8]. Despite its continued use over many countries, its popularity and extensive use, TM has not been officially recognized in most countries. As a result, training and research in this area have not been conducted intensively on the various aspects of TM. The safety and efficacy of data on TM are not sufficient to meet the criteria required to support its worldwide use [4, 5, 9, 10].
In Dega Damot district about 90% of the population relies on traditional health products (unpublished data from the district) for primary health care aspects. There have been no studies conducted in the study area on the use and practice of TM. For policies regarding TM ultimately geared towards integration of TM into the national health service to be formed and implemented, results of this study will be able to protect the interest of those making use of this health care option.
Methods
Description of the study district
This study involved traditional medical practitioners residing in Dega Damot district, Northwestern Ethiopia. It shares borders with the districts of Bibugn in the north, Dembecha in the east, Kuarit and Hulet eju enesie in the west and Jabitehnan in the South (Fig. 1). The district’s administrative town, Feres Bet, is located at about 400 km north western of the capital, Addis Ababa. According to 2013 data, the population of the district is about 170, 575. The district is administratively divided into 32 kebeles and Amharic which belongs to the Semitic language family is the language of the population. In Ethiopia, Kebele is the smallest administrative unit. In the district, barley, maize, potato and wheat are the main crops cultivated, off which, potato is exported to neighboring towns of the Amhara region like Burie, Bahirdar and Gondar.
Fig. 1.
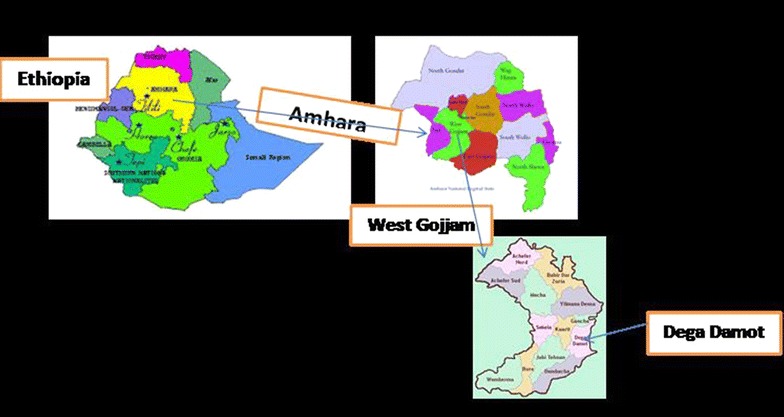
Map of the Dega Damot district (the officials who gave permission to use the respective maps were: personnel of Dega Damot district communication office, west Gojjam zonal communication office and Amhara regional state communication beau rue)
According to 2004–2013 rainfall data, the District has a high rainfall distribution between July and August and a smaller rainfall between January and May. The mean monthly rainfall and mean annual rainfall of the District are 60.24 and 708.54 mm, respectively (National Metrological Service Agency, Bahirdar Branch Office, unpublished data). According to data from the health personnel of the district, the top ten diseases in 2014 are malaria, diarrhea, helmenthiasis, pneumonia, acute upper respiratory diseases, dyspepsia, typhoid, eye infection, urinary tract infection and skin infection respectively.
Selection of study subjects
Data were collected from the traditional medical practitioners (TMPs) who were purposively chosen with the help of community leaders and local authorities. The informants selected were the most knowledgeable ones as recommended by community leaders and local authorities who involved in the selection process. The ages of the TMPs ranged between 22 and 80 years. A total of 45 (40 male and 5 female) TMPs were included in this study from August 10 to September 30/2014.
Data collection techniques
Semi-structured interviews, observation and field walks were used to collect the research data. To collect information about local names of plants used, their threats, part(s) used, preparations methods, routes of remedy administration and diseases treated, individual interviews were conducted (Additional file 1). Interviews were carried out in Amharic, language that is spoken by the practitioners. For claimed plant, specimen was collected, and identified and voucher was reserved at University of Gondar. Field observations were performed to document habitat of each medicinal plant. As this study has been conducted on wild plants, permission was mandatory to perform the survey. Hence, Dega Damot district agricultural office was informed and asked permission to conduct the study and collect the medicinal plants. The study was also ethically approved by the Graduate Program Evaluation Committee of the College of medicine and health sciences, University of Gondar. Prior to the initiation of the data collection, the objective of the survey was clarified to the TMPs, verbal consent was obtained from them. Letter of collaboration was sent to district officials of the study area and biology department at University of Gondar.
Data analysis
Descriptive statistic procedures like percentage and frequency distribution were applied for analyzing and summarizing the data. To check the level of homogeneity among information provided by traditional practitioners, the informants’ consensus factor, ICF [11] was computed
where, Nur = number of use reports from informants for a particular plant-use category; Nt = number of taxa or species that are used for that plant use category for all informants. ICF Values vary between 0 and 1, where ‘1’ represents the highest level of consensus. The fidelity level (FL), which shows for the percentage of informants claiming the use of a certain plant species for the same major purpose, was calculated for the commonly reported disorders as:
where: Np = number of traditional practitioners that claim a use of a plant to treat a certain disease; N = number of informants that use the plants as a remedy to treat an ailment [12].
Results
Socio-demographic data of the informants
Totally, 45 TMPs out of which 40 (88.8%) and 5 (11.2%) males and females, respectively, were involved in this study and 55.6% were illiterate. Most of them were married (86.7%) and 37.8% were older than 56 years. Thirty-one (68.9%) were farmers and all TMPs were Ethiopian orthodox tewahido Christian followers.
Forty percent of healers indicated that they acquired their healing wisdom from their family, whereas 26.6% assumed it as a gift from God. Other sources of wisdom are religious Institutions (22.2%) and preceding sickness and corresponding use (11.2%). About 67% of the practitioners had practiced their healing activities for more than 25 years.
Diseases treated and medicinal Plants used
About 55 human diseases are treated by TMPs of the district. The most commonly treated ones being evil eye, malaria, wound; peptic ulcer disease and rabies (Table 1).This study revealed that about 60 plant species find applications by the TMPs of the district. Those plants were identified and distributed in 42 families. Families, Gramineae and Solanaceae each accounts 4 (9.5%) medicinal plants followed by Fabaceae and Leguminosae, 3 (7%) each. Most of the plants collected and identified from the study area were trees (40%), followed by herbs (30%) and shrubs (25%) and (Fig. 2).
Table 1.
Medicinal plants used to treat human diseases
| Scientific name | Family name | Voucher no. | Amharic name | Habit | Part used | Used for | Preparation, dose and application |
|---|---|---|---|---|---|---|---|
| Acacia Senegal (L.) Wild. | Leguminosae | MW-053 | Grar | Tree | Resin | Stabbing pain | Powder of resin taken mixed with molten butter |
| Agrostis semiverticillata (Forssk.) Christm. | Gramineae | MW-049 | Serdo | Grass | Leaf | Tinea decalvans | Fresh pulverized leaf is applied once daily |
| Albizia gummifera (J.F.Gmel) C.A.Sm | Leguminosae | MW-039 | Sesa | Tree | Bark | Rectal prolapsed | About 80 ml of Powder of bark mixed with little water (decoction) taken once daily |
| Allium sativum L. | Alliaceae | MW-001 | Nech Shinkurt | Bulb | Seed | Evil eye | Crushing the seed with seeds of Lepidium sativum L. and Ruta chalepensis L. and inhale it |
| Fruit | Common cold | Inhale the smell of the fruit | |||||
| Fruit | Malaria | Crushing the fruit and boil it, finally drink it with much amount of milk for 1 day | |||||
| Seed | Dry cough | Crushing the seed and drink with adulterated butter | |||||
| Aloe pulcherrima Gilbert & Sebsebe | Aloaceae | MW-002 | Eret | Tree | Latex | Wound | Applying the latex to the wound for 2 days |
| Artemisia afra Jack. ex Wild. | Asteraceae | MW-003 | Chikugn | Shrub | Leaf | Common cold | Inhaling the smell of the leaf |
| Leaf | Urine retention | Powder of leaf taken once mixed with mead | |||||
| Leaf | Haematuria | Milk decoction of leaf taken once | |||||
| Avena sativa L. | Poaceae | MW-004 | Ankerdad | Grass | Seed | Wound | Drying the seed then crushing, then apply on the wound till the wound cures |
| Bersama abyssinica Fresen. | Melianthaceae | MW-005 | Azamira | Tree | Leaf | Ascariasis | Crushing the leaf and drink it |
| Brucea antidysenterica J. F. Mill. | Simaroubaceae | MW-006 | Abalo | Tree | Root | Evil eye | Crushing its root with the roots of Pterolobium stellatum (Forssk.) Brenan, Carissa spinarum L. and Clausena anisata (Wild) Benth. and inhale it |
| Seed | Cutaneous leshmaniasis | Crushing the seed and apply on the infected area | |||||
| Leaf | Leprosy | Handful of fresh leaf grounded to make a paste and to it add small quantity of honey or butter and it is applied externally until cure | |||||
| Capsicum annuum L. | Solanaceae | MW-007 | Berbere | Shrub | Leaf | Anthrax | Crushing the leaf with leaves of Vernonia amygdalina Del. and eat it on empty stomach once |
| Leaf | Infertility | Small quantities of fruit chewed and swallowed once | |||||
| Carissa spinarum L. | Apocynaceae | MW-008 | Agam | Shrub | Root | Evil eye | Crushing the root with the fruit of garlic and the fruit of Ruta chalepensis L., finally inhale it |
| Root | Snake bite | Crushing the root and bandage on the site of bite for 1 day | |||||
| Citrus aurantifolia. | Rutaceae | MW-036 | Lomi | Tree | Leaf | Hypertension | Crushing the leaf and drying it, finally drinking it as tea |
| Clausena anisata (Wild) Benth. | Rutaceae | MW-059 | Limch | Tree | Stem | Bone dislocation | Stem powder boiled with butter applied daily |
| Whole plant | Mental illness/exorcism | The juice of whole plant is employed for bathing | |||||
| Clematis simensis Fresen. | Ranunculaceae | MW-009 | Azo Hareg | Climber | Leaf | Hemorrhoids | Drying the leaf then crushing it and mixing with butter finally apply to area once |
| Leaf | Skin cancer | Crushing the leaf and apply it to the area of infection | |||||
| Leaf | Eczema | Drying the leaf, crushing it and then mixing it with benzene and wood charcoal | |||||
| Cordial africana Lam. | Boraginaceae | MW-058 | Wanza | Tree | Leaf | Nightmare | Powder of the semi-parasite worn as amulet against startling dreams |
| Coriandrum sativum L. | Umbelliferae | MW-052 | Dinblal | Herb | Seed | Menorhagia | Handful of seeds from each pounded with onions and taken once mixed with milk of black cow |
| Croton macrostachyus Del. | Euphorbiaceae | MW-035 | Bisana | Tree | Leaf | Malaria | Crushing leaf and drink with either Guizotia abyssinica (L.F.) Cass. or milk |
| Root | Tuberculosis | Root powder taken pasted with honey or taken dissolved with mead | |||||
| Cussonia ostinii Chiov. | Araliaceae | MW-048 | Getem | Tree | Bark | Syphilis | An inside part of the bark is pounded into powder which is then taken once mixed with a glass of local beer |
| Cynoglossum coeruleum Hochst. A. Rich. DC. | Boraginaceae | MW-010 | Shingug | Shrub | Leaf | Acute febrile illness | Crushing the leaf with fresh water |
| Datura stramonium L. | Solanaceae | MW-054 | Astenagir | Shrub | – | Headache | Unspecified part of the plant pounded mixed with ink and placed under the skin of the head |
| Leaf | Mumps | Fresh leaf is tied on to the site of the problem | |||||
| Dovyalis abyssinica (A. Rich.) Warb. | Flacoutiaceae | MW-011 | Koshim | Tree | Seed | Decayed teeth | Brushing the decayed teeth with the yellow seed of the plant |
| Echinops kebericho Mesfin | Asteraceae | MW-012 | Kebericho | Shrub | Stem | Evil eye | Drying, crushing and adding the seed on fire to smell |
| Stem | Tape worm | Drying and crushing then drink by mixing with Capsicum annuum L. and salt | |||||
| Stem | Common cold | Burning the root and inhale it | |||||
| Stem | Acute febrile illness | Burning the root on fire and fumigate | |||||
| Embelia schimperi Vatke | Myrsinaceae | MW-013 | Enkoko | Shrub | Seed | Anthrax | Crushing the seed with the seeds of Guizotia abyssinica (L.F.) Cass. and eat with honey |
| Seed | Tape worm | Crushing the seed and drink with alcohol | |||||
| Englerina woodfordioides (Schweinf.) M. Gilbert | Loranthaceae | MW-014 | Teketsila | Shrub | Leaf | Cutaneous leshmaniasis | Crushing the leaf and apply it topically |
| Eragrostis tef (Zucc.)Trotter | Gramineae | MW-045 | Nech teff | Herb | Seed | Diarrhea | Porridge of the floor eaten three times daily |
| Erytbrina brucei Schweinf. | Fabaceae | MW-015 | Korch | Tree | Leaf | Wound | Crushing its leaf with the leaves of Solanum incanum L. and Phytolacca dodecandra L’Hérit, finally apply it to the wound once for 3 days |
| Eucalyptus globulus Labill. | Myrtaceae | MW-016 | Nech Bahirzaf | Tree | Leaf | Common cold | Burning the leaf on fire and inhale it |
| Euphorbia abyssinica J.F.Gmel. | Euphorbiaceae | MW-034 | Kulkual | Tree | Latex | Jaundice | Mixing the latex with teff powder and putting it in fire till it becomes semidry |
| Root | Rabies | Crushing the root and mixing with powder of wheat or teff, finally drying it on fire | |||||
| Leaf | Cutaneous leshmaniasis | Crushing the leaf and mixing it with butter | |||||
| Latex | Skin cancer | Applying the latex to the affected area | |||||
| Root | Malaria | Crushing the root and drink with milk | |||||
| Ficus vasta Forssk. | Moraceae | MW-038 | Shola | Tree | Bark | Epilepsy | Fumigate the patient once daily with the smoke of the powder of bark |
| Root | Frequent miscarriage | Root and leaf powder taken once mixed with milk | |||||
| Grewia ferruginea Hochst. ex A. Rich. | Tiliaceae | MW-017 | Lenquata | Shrub | Bark | Hair fungus | Washing hair with the latex of the bark |
|
Guizotia abyssinica (L.F.) Cass. |
Compositae | MW-040 | Nug | Herb | Fruit | Rabies | A cup of oil is given in morning in empty stomach for 3 days |
| Seed | Dry cough | A cup of seed powder decoction is given orally in the morning and evening for a week | |||||
| Seed | Retained placenta | Boil the oil of the seed together with onions and egg and allow the steam to get into the vagina cavity | |||||
| Hagenia abyssinica (Brace.) J. F. Gmel. | Rosaceae | MW-018 | Koso | Tree | Leaf | Tape worm | Crushing the fresh leaves and mix with water and drink it once |
| Hordeum vulgare | Gramineae a | MW-033 | Gebs | Grass | Seed | Peptic ulcer disease | Drying the seed on fire and eat |
| Hypericum revolutum (Forssk.) Vahl | Guttiferae | MW-056 | Amja | Shrub | Fruit | Earache | Fruit juice applied as ear drops |
| Juniperus procera Hochst. | Cupressaceae | MW-057 | Tsid | Tree | Resin | Congestive heart failure | Powder of fried resin taken orally mixed with water |
| Justicia schimperiana (Hochst.ex Nees) T. Anders. | Acanthaceae | MW-019 | Simeza | Tree | Leaf | Anthrax | Crushing the leaf and mix with fresh water drink it once on empty stomach |
| Kalanchoe petitiana A.Rich. | Crassulaceae | MW-020 | Andahula | Herb | Stem | Hemorrhoids | Putting the stem on fire till it becomes hot then putting it on the area of infection |
| Leaf | Abdominal cramp | Crushing the leaf and eat it | |||||
| Root | Sexual dysfunction | Milk decoction of the fresh pulverized roots and leaves | |||||
| Lathyrus sativus L. | Leguminosae | MW-044 | Guaya | Herb | Seed | Constipation | Seeds eaten cooked at least once daily to overcome evacuation problem |
| Lepidium sativum L. | Cruciferae | MW-050 | Feto | Herb | Seed | Wound | Powder of seed mixed with latex of Euphorbia abyssinica and bandaged once daily every other day |
| Linum usitatissimum L. | Linaceae | MW-021 | Telba | Shrub | Seed | Anthrax | Crushing the seed with the seeds of Lepidium sativum L. or Guizotia abyssinica (L.F.) Cass. Then eating with honey on empty stomach |
| Seed | Peptic ulcer disease | Boil the seed with water and after cooling drink it | |||||
| Seed | Pain during delivery | Putting the seed in water till it becomes semisolid and drink it | |||||
| Lupinus albus L. | Fabaceae | MW-041 | Gibto | Herb | Seed | Hypertension | Small quantity of seed and fruit is grounded with water, filtered. The resultant juice is given orally in the morning for 1 month |
| Myrica salicifolia Hochst. ex A.Rich | Myricaceae | MW-060 | Shinet | Tree | Root | Headache | Butter paste of the root powder placed in the nostril |
| Olinia rochetiana A. Juss. | Oliniaceae | MW-023 | Chife | Tree | Leaf | Teeth ache | Chewing the leaf within the mouth for about a minute and spit it |
| Root | Goiter | Powder of root and leaf mixed with latex of euphorbia abyssinica and bandaged on the goiter once every other day | |||||
| Osyris quadripartite Decn. | Santalaceae | MW-042 | Keret | Tree | Leaf | Jaundice | A handful of fresh leaf is grinded and cup of this juice given orally for 15 days |
| Phytolacca dodecandra L’Hérit | Phytolaccacee | MW-024 | Mekan Endod | Climber | Leaf | Anthrax | Crushing the leaf with fresh water and drink one glass of it once |
| Leaf | Scabies | Crushing the leaf and washing the area of infection with the crushed leaf | |||||
| Bark | Jaundice | Powder of bark taken once mixed with diluted local beer | |||||
| Root | Rabies | Crushing the root and drink with honey | |||||
| Rhamnus prinoides L’Herit | Rhamnaceae | MW-026 | Gesho | Shrub | Leaf | Wound | Crushing the leaf and apply it to the wound till the wound cures |
| Leaf | Epitaxis | Leaf powder taken mixed with once own urine | |||||
| Ricinus communis L. | Euphorbiaceae | MW-047 | Chakma | Shrub | Leaf | Appendicitis | Fresh pulverized leaf infused in water solution of safflower powder and one glass taken only once |
| Rumex nepalensis Spreng. | Polygonaceae | MW-027 | Yewusha Milas | Herb | Leaf | Acute febrile illness | Crushing leaf with fresh water and wash with it |
| Rumex nervosus Vahl | Polygonaceae | MW-028 | Ambacho | Shrub | Leaf | Wound | Crushing the leaf and mixing with benzene, then boil it, finally washing the wound with it |
| Ruta chalepensis L. | Rutaceae | MW-029 | Tiladam | Shrub | Seed | Evil eye | Crushing the seed with the seeds of garlic and apply it on the nostril |
| Leaf | Epitaxis | Fresh pulverized leaves are placed in the nostril | |||||
| Root | Headache | Powder of root and garlic mixed with water | |||||
| Root | Recurrent seasonal illness | Decoction of fresh pulverized root applied externally | |||||
| Skebergia capensis Sparrm. | Meliaceae | MW-046 | Lol | Tree | Bark | Malaria | Infusion of fresh pulverized bark |
| Snowdenia polystachya (Fresen.)Pilg. | Graminaceae | MW-051 | Muja | Herb | Whole plant | Menorhagia | Juice or infusion of whole plant taken once |
| Solanum incanum L. | Solanaceae | MW-055 | Embuay | Climber | Seed | Attention deficient disorder | Powder of seed given in small amount through the nose to help a child to be a fast learner and intelligent |
| Syzygium guineense (Wild.) Dc. | Myrtaceae | MW-043 | Dokma | Tree | Root and leaf | Syphilis | A decoction is made from each one teaspoon of root and leaf powder and a cup of this decoction is given orally three times a day for 7 days |
| Trigonella foenum-graecu | Fabaceae | MW-037 | Absh | Herb | Seed | Peptic ulcer disease | Putting in water, drying it, crushing and the eating by mixing with water and sugar |
| Seed | Dry cough | Crushing the seed and boil with milk | |||||
| Seed | Weight loss | Putting in water, drying it, crushing and the eating by mixing with water and sugar | |||||
| Descopodium penninervum Hochst. | Solanaceae | MW-022 | Aluma | Tree | Seed | Wound | Crush the dried seed and apply the powder to the affected area for 3 days |
| Urtica simensis | Urticaceae | MW-025 | Sama | Herb | Leaf | Peptic ulcer disease | Boil the semi-crushed leaf and eat it for 2 or 3 days |
| Root | Malaria | The root will be crushed and dried the mixed with fresh water, drink one glass of it and drink much amount of milk | |||||
| Vernonia amygdalina Del. | Asteraceae | MW-030 | Girawa | Tree | Leaf | Bladder distention | Crushing the leaf with water and drink about one glass once |
| Zehneria scabra (Linn. f.) Sond. | Cucurbitaceae | MW-031 | Haregresa | Climber | Leaf | Diarrhea | Crushing the leaf and mix with some fresh water, finally drink one cup of it |
| Leaf | Acute febrile illness | Boil the leaf in water till it evaporates and then fumigate with it | |||||
| Leaf and root | Sexual dysfunction | Bathe in the infusion of leaf and root for 7 days | |||||
| Root, bark and leaf | Gout | Decoction of root, bark and leaf and excrement of hyena employed for bathing | |||||
| Zingiber officinale Roscoe. | Zingiberaceae | MW-032 | Zingibl | Bulb | Root | Bladder distention | Crushing the root with fresh water and drink about one glass once |
| Root | Abdominal cramp | Crushing the root and mixing with some water then drink the filtrate |
Fig. 2.
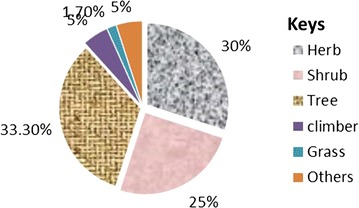
Frequency distribution of growth form of medicinal plants
Plant parts used
According to this survey, the commonly used plant part was leaf (36.5%), followed by seed (21.2%) (Fig. 3).
Fig. 3.
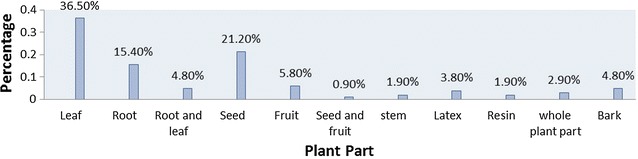
Frequency distribution of plant parts used to prepare remedies
Method of preparation, routes of administration and dose
Traditional medical practitioners used simpler techniques like crushing and powdering with the help of easily available materials like water, honey and milk for preparation of remedies to treat various human ailments as shown in Table 1. This survey also documented that most of the remedies were given orally, (44%). Topical (26.5%), nasal (25.5%), rectal (2%), vaginal (1%) and subcutaneous (1%) routes are also used. This study showed that TMPs in the district were not aware of the exact dose of remedies to be administered. They easily determined the dose depending on mainly age. The doses of 24 preparations were not determined. Healers expressed doses as a glass of, half a cup of or a teaspoon full of.
Dosage forms and frequency of administration
The documented 60 species of medicinal plants were reported to be formulated in various forms. Majority of dosage forms were decoctions 35 (38.9%) followed by liquid preparations 18 (20%) as shown in Fig. 4. Most of the preparations were given only once (Fig. 5).
Fig. 4.
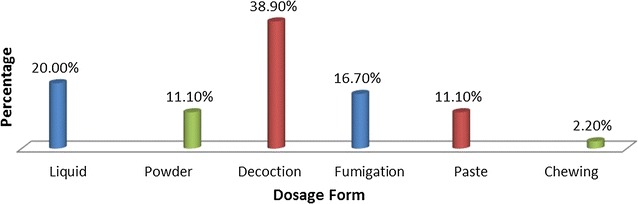
Frequency distribution of dosage forms of plant remedies
Fig. 5.
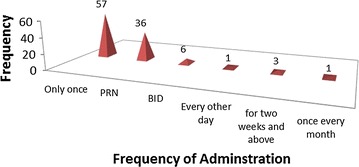
Distribution of frequency of administration of plant remedies
Solvents and additives
Forty-three percent of the formulations did not require any additive or solvent. Of the formulations that involve the use of solvents, water accounted 25 (42.4%) followed by milk 8 (13.6). Different additives like butter, honey, sugar and others were also incorporated (Table 2).
Table 2.
Solvents and additives used
| Solvents and additives | Number (%) of formulations |
|---|---|
| Water | 25 (42.4) |
| Alcohol | 5 (8.5) |
| Milk | 8 (13.6) |
| Benzene | 2 (3.4) |
| Honey | 4 (6.8) |
| Salt | 1 (1.7) |
| Sugar | 4 (6.8) |
| Charcoal | 1 (1.7) |
| Butter | 5 (8.5) |
| Ink | 1 (1.7) |
| Urine | 1 (1.7) |
| Teff | 2 (3.4) |
Contraindications and side effects
According to TMPs of the area, 42 (40.4%) of the formulations were contraindicated for pregnant patients. No contraindication was indicated for 35 (33.6% of the formulations (Table 3). Twelve (11.5%) of the preparations were free from any side effect (Table 4).
Table 3.
Distribution of contraindication to remedies
| Category | Frequency | % Age |
|---|---|---|
| Contraindicated to | ||
| Children | 19 | 18.3 |
| Pregnant women | 42 | 40.4 |
| Elderly | 8 | 7.7 |
| No contraindication | 35 | 33.6 |
Table 4.
Frequency distribution of side effects of remedies
| Category | Frequency | % Age |
|---|---|---|
| Those with known side effects | ||
| Nausea | 15 | 14.4 |
| Vomiting | 15 | 14.4 |
| Diarrhea | 8 | 7.7 |
| Loss of consciousness | 8 | 7.7 |
| Local pain | 12 | 11.5 |
| Headache | 6 | 5.8 |
| Nasal stiffness | 10 | 9.6 |
| PUD | 4 | 3.8 |
| Constipation | 3 | 2.9 |
| Abdominal cramp | 9 | 8.7 |
| Free from any side effect | 12 | 11.5 |
Drug food interactions
According to this study, only 17% of the formulations possessed drug food interactions, of which 12 (66.7%) were exhibited by preparations for gastrointestinal problems. Synergistic reactions were observed in poly herbal preparations like in the case of remedies for evil eye.
Storage
Asked on how they store plant remedies, healers responded that they don’t normally store plant preparations; rather they collect fresh material and formulate remedies. For those medicinal plants which are not easily available and which are seasonal, they collect and store in papers, horns or and with in bottles. Only three percent of the total preparations were stored in cool and dry places (Fig. 6).
Fig. 6.
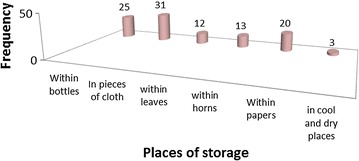
Frequency of storage of remedies
Informant’s consensus
Depending on the data obtained, seven use-categories (Table 5) were set in which 127 use reports were documented. As depicted below, informant consensus factor values and the mean ICF are close to 1. There is high uniformity in plant consumption for respiratory diseases.
Table 5.
Informants’ consensus score
| Use category | Species (#) (nt) | Use-reports (Ur) | ICF (nur − nt/nur − 1) |
|---|---|---|---|
| Gastrointestinal problems | 7 | 15 | 0.57 |
| Central nervous system disorders | 9 | 18 | 0.53 |
| Respiratory problems | 2 | 6 | 0.8 |
| Urinary tract problems | 7 | 15 | 0.57 |
| Skin problems | 8 | 13 | 0.42 |
| Cardiovascular disorders | 13 | 28 | 0.55 |
| Other organ problems | 14 | 32 | 0.58 |
| Mean ICF | 0.57 | ||
Fidelity level
In the survey, the FL values were analyzed for seven plants in treating three medical conditions (Table 6). Croton macrostachyus (FL = 0.78) is reported by high number of informants (36%) in treating malaria. Allium sativum (FL = 0.75) is more preferable than Echinops kebericho (FL = 0.64) in treating evil eye.
Table 6.
FI for plant species used to treat evil eye, malaria and rabies
| Ailments | Percentage of informants | Species | Np | N | FI (Np/N) |
|---|---|---|---|---|---|
| Evil eye | 30 | Allium sativum | 6 | 8 | 0.75 |
| 34 | Echinops kebericho | 7 | 11 | 0.64 | |
| Rabies | 9 | Guizotia abyssinica | 4 | 5 | 0.8 |
| 34 | Phytolacca dodecandra | 8 | 9 | 0.89 | |
| Malaria | 19 | Urtica simensis | 10 | 15 | 0.67 |
| 36 | Croton macrostachyus | 7 | 9 | 0.78 | |
| 5 | Euphorbia abyssinica | 5 | 12 | 0.42 |
Np number of TMPs who used the medicinal plant for the same purpose, N number of TMPs who used the medicinal plant for various purposes
Threats to medicinal plants
As shown in Table 7 below, drought, overgrazing and firewood collection are the major threats of medicinal plants. Practitioners leveled drought as the most serious threat.
Table 7.
Threats to medicinal plants
| Threats to medicinal plants | % of TMPs |
|---|---|
| Drought | 55.6 |
| Overgrazing | 22.2 |
| Firewood collection | 15.6 |
| Agricultural expansion | 4.4 |
| Soil erosion | 2.2 |
Discussion
This study revealed that about 60 plant species find applications by the TMPs of the woreda. Those plants were identified and distributed in 42 families. Families, Graminae and Solanaceae each accounts 4 (9.5%) medicinal plants followed by Fabaceae and Leguminosae, 3 (7%). But Fabaceae was the dominant family according to the conducted in Hawasa [13], Wayu Tuka District of Oromiya region [14] and Benshangul-Gumuz [15]. In addition a study done in Spain [16], Korea [17] and Loma and Gena Bosa Districts [18] showed that Asteraceae has the highest number of medicinal plants. Caesalpiniaceae was the family with higher number of plants according to the study in Nigeria [19].
The ailments reported to be handled by the TMPs of the district are those disorders most prevalent in the district. According to the result of this study, the majority of plants were reported to treat wound followed by malaria, evil eye and anthrax. However, a study done in Hawasa [13] showed that stomach ache is the disease treated by large number of medicinal plants. In addition a study done in Sheko ethinic group of Ethiopia [8] showed that skin and gastrointestinal problems were the commonly treated diseases. According to a study in Lebanon [20], most medicinal plants were used to treat gastrointestinal disorders, kidney and urinary diseases as well as blood and cardiovascular diseases. Diarrhea was the commonly treated disease in Benshangul-Gumuz [15].This discrepancy may be the result of the difference in the climatic, ethnic, and hygienic conditions the areas. The current study is also unlike the one done in Israel [21]. Mental illnesses were commonly treated according to the study in Kenya [22].
The most commonly used plant part was leaf in this study area which is in agreement with other studies. [8, 13, 15, 18, 19, 21, 23–26]. Considerable threat to the mother plant radiates to the various parts of the plant. However, root was the commonly used plant part according to a study done in Benshangul-Gumuz [15]. Medicinal plants were formulated in various forms using various solvents and additives. They were formulated as decoctions, liquid preparations and pastes. This is supported by a study done in Korea [17], Israel [21], Gondar zuria woreda [24] and Hawasa [13]. However, in a study done in Chencha [18] and Tewledere districts [27], the majority of remedies were formulated as concoctions. Practitioners prepare remedies in such a simple manner without further processing which may be due to lack of education and processing instruments. TMPs of the current study area used butter, charcoal, sugar, milk and salt as additives to increase the efficacy and potency of the remedies. The rationale behind the use of honey and sugar is just to make the formulation palatable. This is supported by a study done in Israel [17] and Hawasa [13].
This study showed that there was no harmony in measurement or unit used among practitioners. Most informants stated measuring units like cup, spoon, bottle and handful which lack accuracy. This problem was also observed in studies done elsewhere which may be due to lack of education [13, 14, 19, 28].
This study revealed that higher sizes of preparations were given orally which agrees with results of other studies [11–13, 15, 17, 22–25, 27–29]. Practitioners prefer simple routes like topical and oral due to their inability to administer remedies in other routes like intravenous. Oral administration allows relatively fast physiological action of remedies on pathogens and enhance its efficacy. However, studies conducted in Sheko ethnic group in Southwest Ethiopia [8] revealed that most preparations were prescribed for administration to the cutaneous route. According to the result of the current study, most formulations were given only once. This may be due to the fact that most practitioners do not know the actual dose to be given and fear the risk that comes at the end of the treatment due to over dose and continuous administration.
One-third of the medicinal plants recorded were trees. However, other research works indicate the abundant use of herbs [8, 22, 24, 25, 27, 30]. The availability of most woody plants in the area might have enforced the local inhabitants to rely on tress.
Most of the formulations were contraindicated for pregnant patients. This is due to the healers’ belief that it may harm the fetus. No contraindication is indicated for one-third of the formulations. Most preparations taken orally cause nausea, vomiting and abdominal cramp whereas, some of the preparations are free from any side effect which may be due to the lack of follow up of patients by healers once they gave remedies and due to illiteracy of the patients.
This study revealed that, only some of the formulations possessed drug food and drug–drug interactions, this may be because most practitioners are illiterate, they do not know about the interaction of their remedies with modern medicines. In addition practitioners do not follow the progress of their patients, hence have little information on drug food interaction. Synergistic reactions were observed in poly herbal preparations like in the case of remedies for evil eye.
According to this study, practitioners do not normally store remedies which is in contrast to the study done in Addis Ababa [28]. For those medicinal plants which are not easily available and which are seasonal, practitioners collect and store in papers, horns and with in bottles. Only three percent of the total preparations are stored in cool and dry places. This may be due to the lack of modern education about drug storage and other health related issues.
A total of 127 URs from 60 species of plants were recorded which were assigned to seven use categories. Analysis of ICF shows that there exists a high evenness of plant consumption among the population which is in harmony with the study in Chencha [18]. The low ICF for skin problems may because of a multifaceted preparation of plants required to treat disease. Majority of plant species have a number of medicinal values, which result in higher variety of use reports.
Croton macrostachyus (FL = 0.78) is reported by high number of informants (36%), hence more preferable than Euphorbia abyssinica (0.42) and Urtica simensis (0.67) in treating malaria. However, despite Allium sativum (FL = 0.75) is reported by less figures of informants (30%), than Echinops kebericho (FL = 0.64) which is mentionedd by relatively higher percentage of practitioners (34%), it seems that Allium sativum is more preferable than Echinops kebericho in treating evil eye. But a study done in Sheko [8] indicated that Ocimum lamiifolium, Phytolacca dodecandra, Amaranthus dubius and Amaranthus graecizans were the medicinal plants assigned with the highest FL values. This discrepancy may be the result of the differences in the type of diseases dominating the areas, and the level of availability of the medicinal plants.
According to the results of this study, drought is the most serious threat to medicinal plants followed by overgrazing. This is in conformity with the survey conducted in Gemad district [25] and Kilte Awulalo [27], but according to a study done in Loma and Gena Bosa [26], agricultural expansion was the major threat followed by timber and other demands. This is probably due to the increasing number of population. However, study done in Hawasa city [13] indicated urbanization as the most serious threat for medicinal plants.
Conclusion
Dega Damot district is loaded in its medicinal plant diversity and indigenous knowledge though plants are highly affected by drought, overgrazing and firewood collection. Therefore awareness activities must be created among the district’s population by concerned governmental and nongovernmental organizations about the value of medicinal plants and conservation of these plants. The healing potential and associated adverse issues of the claimed medicinal plants should be assessed before proposing for a broader utilization.
Authors’ contributions
All of the authors had magnificent contribution in the design of the study, data collection and analysis and preparation of the manuscript. MW and TA played a pivotal role in writing the proposal and designing the study. MW was instrumental during the data collection, analysis and manuscript preparation. GD involved in the discussion as well as manuscript preparation of this paper. All authors read and approved the final manuscript.
Acknowledgements
We are indebted to the people of Dega Damot district for their unreserved collaboration and hospitality. We have appreciated the Dega Damot district offices of Rural Agricultural Development, Health, Administration and Plan and Finance for their provision of information during data collection. We thank university of Gondar and Debre Markos University for their support to conduct our study and biology department, university of Gondar for the provision of some facilities during identification of plants. Our gratitude also goes to Mr. Abyu Eniyew, a botanist at University of Gondar, who identified the plants. The role of the west Gojjam zone communication office and Amhara region communication beaurue was also instrumental.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Data and materials will be available on request at any time.
Ethical approval and consent to participate
The study was ethically approved by the Graduate Program Evaluation Committee of the College of medicine and health sciences, University of Gondar. Prior to the initiation of the data collection, the objective of the survey was clarified to the TMPs, verbal consent was obtained from them. Letter of collaboration was sent to district officials of the study area and biology department at University of Gondar.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- HIV
human immunodeficiency virus
- ICF
informant’s consensus factor
- PUD
peptic ulcer disease
- TM
traditional medicine
- TMPs
traditional medical practitioners
- UR
use-report
Additional file
Additional file 1. Semi-structured interview questions.
Contributor Information
Muluken Wubetu, Email: mulukenwubetu1986@gmail.com.
Tefera Abula, Email: abula_tefera@yahoo.com.
Getye Dejenu, Email: dgetiye@gmail.com.
References
- 1.Dejene T. An overview of the role of traditional medicine in Ethiopia. J Res Arts Educ. 2011;2(4):34–40. [Google Scholar]
- 2.Dawn M. Traditional medicine in contemporary context protecting and respecting indigenous knowledge and medicine. J Aborig Health. 2003;3(1):22–50. [Google Scholar]
- 3.Teferi D, Sundara R. Demand for traditional health care services in rural Ethiopia. Middle East J Sci Res. 2013;13:01–10. [Google Scholar]
- 4.Kebede D, Alemayehu A, Binyam G, Yunis M. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Health Dev. 2006;20(2):128–134. [Google Scholar]
- 5.Abebe D, Ayehu A. Medicinal plants and enigmatic health practices of northern Ethiopia. Addis Ababa, Ethiopia: B.S.P.E; 1993 [Original from the University of California].
- 6.Arnold N. Modernity in traditional medicine: women’s experiences and perceptions in the Kumba health district, SW region, Cameroon. UMEA Univ. 2011;4(2):15–42. [Google Scholar]
- 7.Wondwosen T. Impacts of urbanisation on the traditional medicine of Ethiopia. Anthropologist. 2005;8(1):43–52. [Google Scholar]
- 8.Mirutse G, Zemede A, Zerihun W. Ethnomedicinal study of plants used by Sheko ethnic group of Ethiopia. J Ethnopharmacol. 2010;132:75–85. doi: 10.1016/j.jep.2010.07.046. [DOI] [PubMed] [Google Scholar]
- 9.Elias A, Tesfaye G, Bizatu M. Aspects of common traditional medical practices applied for under-five children in Ethiopia, Oromia region, eastern-Harargie district, Dadar Woreda. Commun Med Health Educ. 2013;3(6):1–8. [Google Scholar]
- 10.Sara A, et al. Traditional healing practices among American muslims: perceptions of community leaders in southeast Michigan. J Immigrant Minor Health. 2011;3(5):17–28. doi: 10.1007/s10903-011-9495-0. [DOI] [PubMed] [Google Scholar]
- 11.Bhat JA, Kumar M, Negi A, Todaria N. Informants’ consensus on ethnomedicinal plants in Kedarnath Wildlife Sanctuary of Indian Himalayas. J Med Plants Res. 2013;7(4):148–154. [Google Scholar]
- 12.Alexiades MN. Collecting ethnobotanical data: an introduction to basic concepts and techniques. Adv Econ Bot. 1996;10:53–96. [Google Scholar]
- 13.Reta R. Assessment of indigenous knowledge of medicinal plant practice and mode of service delivery in Hawassa city, southern Ethiopia. J Med Plants. 2013;7(9):517–535. [Google Scholar]
- 14.Moa M, et al. An ethnobotanical study of medicinal plants in Wayu Tuka district, East Welega zone of Oromia regional State, West Ethiopia. J Ethnobil Ethnomed. 2013;9:68. doi: 10.1186/1746-4269-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teferi F, Teferi G, Kaleab A. Ethnomedical survey of Berta ethnic group Assosa Zone, Benishangul-Gumuz regional state, mid-west Ethiopia. J Ethnobiol Ethnomed. 2009;5:14. doi: 10.1186/1746-4269-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorka M, et al. Medicinal plants traditionally used in the Northwest Spain. J Ethnopharmacol. 2013;4(9):01–22. [Google Scholar]
- 17.Mi-Jang S. Ethnopharmacological survey of medicinal plants in Jeju Island, Korea. J Ethnobiol Ethnomed. 2013;9:48. doi: 10.1186/1746-4269-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammed A, Seyoum G. Medicinal plants biodiversity and local healthcare management system in Chencha district; Gamo Gofa, Ethiopia. J Pharmacogn Phytochem. 2013;2(1):284–293. [Google Scholar]
- 19.Abubakar M, Musab A, Ahmeda M. The perception and practice of traditional medicine in the treatment of cancers and inflammations by the Hausa and Fulani tribes of Northern Nigeria. J Ethnopharmacol. 2007;111:625–629. doi: 10.1016/j.jep.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Taha D, et al. Survey of medicinal plants currently used by herbalists in Lebanon. Pak J Bot. 2013;45(2):543–555. [Google Scholar]
- 21.Said O, et al. Ethnopharmacological survey of medicinal herbs in Israel, the Golan Heights and the West Bank region. J Ethnopharmacol. 2002;83:251–265. doi: 10.1016/S0378-8741(02)00253-2. [DOI] [PubMed] [Google Scholar]
- 22.David M, et al. Traditional healers and their provision of mental health services in cosmopolitan informal settlements in Nairobi, Kenya. Afr Technol Policy Stud Netw. 2013;67:228–257. doi: 10.4314/ajpsy.v16i2.17. [DOI] [PubMed] [Google Scholar]
- 23.Gidey Y, Samuel Z. Ethnobotanical study of traditional medicinal plants in Gindeberet district, western Ethiopia. Mediterr J Soc Sci. 2011;2(4):49–54. [Google Scholar]
- 24.Muthuswamy R, Mequente S. The study of spiritual remedies in orthodox rural churches and traditional medicinal practice in Gondar Zuria district, Northwestern Ethiopia. PHCOG J. 2009;1(3):178–183. [Google Scholar]
- 25.Kalayu M, Gebru T, Teklemichael T. Ethnobotanical study of traditional medicinal plants used by indigenous people of Gemad district, Northern Ethiopia. J Med Plants Stud. 2013;1(4):32–37. [Google Scholar]
- 26.Mathewos A, Sebsebe D, Zemede A. Ethnobotany of medicinal plants in Loma and Gena Bosa districts of Dawro Zone, southern Ethiopia. Top Cl J Herb Med. 2013;2(9):194–212. [Google Scholar]
- 27.Abraha T, Balcha A, Mirutse G. An ethnobotanical study of medicinal plants used in Kilte Awulaelo district, Tigray region of Ethiopia. J Ethnobiol Ethnomed. 2013;9:65. doi: 10.1186/1746-4269-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wubet B, Mirutse G, Tilahun T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomed. 2011;7:39. doi: 10.1186/1746-4269-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roy L. The effect of Russian traditional medicine on the health care of Russian immigrants to America. An honors thesis, Submitted to University Honors College, Texas Tech University. 2011.
- 30.Mohammed A, Berhanu A. Ethnobotanical survey of traditional medicinal plants in Tehuledere district, South Wollo, Ethiopia. J Med Plants Res. 2011;5(26):6233–6242. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials will be available on request at any time.


