Abstract
In 2013 Indonesia, the world's fourth most populous country, declared that it would provide affordable health care for all its citizens within seven years. This crystallised an ambition first enshrined in law over five decades earlier, but never previously realised. This paper explores Indonesia's journey towards universal health coverage (UHC) from independence to the launch of a comprehensive health insurance scheme in January 2014. We find that Indonesia's path has been determined largely by domestic political concerns – different groups obtained access to healthcare as their socio-political importance grew.
A major inflection point occurred following the Asian financial crisis of 1997. To stave off social unrest, the government provided health coverage for the poor for the first time, creating a path dependency that influenced later policy choices. The end of this programme coincided with decentralisation, leading to experimentation with several different models of health provision at the local level. When direct elections for local leaders were introduced in 2005, popular health schemes led to success at the polls. UHC became an electoral asset, moving up the political agenda. It also became contested, with national policy-makers appropriating health insurance programmes that were first developed locally, and taking credit for them.
The Indonesian experience underlines the value of policy experimentation, and of a close understanding of the contextual and political factors that drive successful UHC models at the local level. Specific drivers of success and failure should be taken into account when scaling UHC to the national level. In the Indonesian example, UHC became possible when the interests of politically and economically influential groups were either satisfied or neutralised. While technical considerations took a back seat to political priorities in developing the structures for health coverage nationally, they will have to be addressed going forward to achieve sustainable UHC in Indonesia.
Keywords: Decentralisation, experimentalist governance, health financing, health insurance, Indonesia, Universal Health Coverage, social protection, path dependence
Key Messages
Progress towards universal health coverage in Indonesia has been uneven and iterative, but consistently driven by domestic political interests.
Political commitments have generally preceded planning based on technical evidence or analysis. In some cases, these commitments created precedents that constrained future policy choices.
Decentralisation opened up a space for policy experimentation which allowed for the development of multiple models of health coverage at the district level.
Media attention and politicians who sought to be elected helped to spread the more successful models, which were imitated or adapted by other districts, and eventually appropriated at the national level. However, formal learning was poorly captured and shared.
Introduction
Over the last decade, >30 middle-income countries and a handful of low income countries have launched ambitious plans to ensure that all of their citizens can get the health care they need without undue financial pain. This push for what has become known as ‘universal health coverage’ is being promoted by development agencies such as the World Health Organisation (WHO) and the World Bank (Rodin and de Ferranti 2012). In most cases, the impetus for more inclusive health coverage has been domestic, and implementation has been nationally driven. However the international organisations that retrospectively imposed the umbrella label of ‘UHC’ on these efforts have now joined scholars in seeking common threads across the experience of different countries. Their papers focus largely on technical issues of implementation such as financing models, inclusion criteria, benefits provided and monitoring systems (Lagomarsino et al. 2012; Boerma et al. 2014; Cotlear et al. 2015). Other scholars underline the importance of local political and other institutional circumstances in determining how far individual countries get in realising their ambitions in attaining universal health coverage (Agyepong and Adjei 2008; Rosser et al. 2011; Savedoff et al. 2012; Harris 2015; Reich et al. 2015).
Of the nations now working to provide all their citizens with affordable health services, few are more ambitious than Indonesia. The geographic, human and economic diversity of the world's fourth most populous nation present particular challenges. Some 150 million people are squeezed into Java – an island with the same land area as England1 – the other 100 million Indonesians are scattered across some 7,000 other inhabited islands over a distance equivalent to that from London to Tehran. In the capital Jakarta, 4% lived below the local poverty line in 2014. In Papua province, the figure was 28%. Official data show that income inequalities, measured by the GINI coefficient, increased in 30 out of 33 provinces with comparable data between 2007 and 2014 (Badan Pusat Statistik 2015). The nationally-determined poverty rate, 11%, understates the proportion who would be desperately hard hit by major health spending: at last count, some 43% of Indonesians were living on less than US$2.00 a day.2 Variation in income is reflected in health status: in Maluku, with a provincial GDP of US$170 per person per year, fully 52% of children under 5 were stunted in 2013, twice the fraction that suffered from stunting in Riau Islands province, where per capita GDP was US$870 a year. Access to services is also widely uneven. Just 27% of pregnant women in North Sumatra gave birth in a health facility in 2014, compared with 97% in Bali (Kementerian Kesehatan Republik Indonesia 2015). A 2008 analysis underlined the disparity in access to hospital services. The richest tenth of the population occupied four times as many hospital bed nights per capita compared with the poorest tenth (Thabrany 2008).
Since 1998, Indonesia has undergone cataclysmic political change. For the first five and a half decades of its existence, virtually all policy decisions were taken by the central government in Jakarta. Service delivery at provincial and district levels was often overseen by bureaucrats appointed by the centre. In 2001, just three years after General Suharto stepped down after 32 years in power, responsibility for health, education, infrastructural investment and much else was handed to district governments. At the time there were fewer than 300 districts. By 2014, there were 514. Since 2005, the leaders of these districts have been directly elected. This has led to changes in the relationship between citizen and state that have had profound implications for health financing and service provision (Pisani 2013; Aspinall 2014).
It was against this background that Indonesia in 2012 declared that it would achieve universal health coverage by 2019 (Republic of Indonesia 2012). Indonesia has a flair for setting politically ambitious targets, and working out the details later. The first example was the nation's declaration of independence, which read: “We the people declare the independence of the Republic of Indonesia. Details of the transfer of power etc. will be worked out carefully and as soon as possible”. Many other grand ambitions were enshrined in the constitution that was adopted the day after independence was declared (Republic of Indonesia 1945).
Though the 1945 constitution did not mention health explicitly, the Basic Health Law of 1960 stated that all citizens had a right to be physically, mentally and spiritually healthy. In Article 8, the state assumed responsibility for ensuring that Indonesians had equal access to health services. It made special mention of civil servants and blue-collar workers, and referred without elaboration to the provision of “health funds”. Yet it was to take more than five decades for there to be any significant shift towards providing pooled health insurance that would allow a majority of Indonesians to access affordable health services.
The aim of this historically-rooted study is to trace the Indonesia's progress towards universal health coverage, setting it in its political and economic context. We cover the period from independence in 1945 to the start of 2014, when a health insurance programme expected to encompass all citizens was formally launched. We believe a clear understanding of this evolution, and the forces that shaped it, may help to inform future policy choices both in Indonesia and in other countries journeying towards a similar goal.
Some of the technical decisions made along this journey have been described elsewhere (Rokx et al. 2009; Dwicaksono et al. 2012; Pigazzini et al. 2013; Simmonds and Hort 2013; Marzoeki et al. 2014; Mboi 2015). In this study of the social, political and economic events which shaped the path to affordable health services in Indonesia, we build on earlier analyses of the interaction between health policy and national governance, in particular two important and linked developments in Indonesia: democratisation and decentralisation (Rosser et al. 2011; Aspinall 2014).
To frame our analysis of developments in these two areas, we draw on two bodies of theory: historical institutionalism and experimentalist governance.
A core concept within historical institutionalism is path dependence, which asserts that the range of possible policy choices at any given moment is constrained (and in some cases is determined) by the institutions that have emerged in the past, and the choices those institutions have shaped (Steinmo 2008). In the democratic arena, promises made to the electorate and services delivered by previous governments both contribute to voter expectations, limiting policy choices in the present, and foreclosing different pathways in the future (Mahoney 2000).
Experimentalist governance is an approach to governance which capitalises on the differences that emerge in a decentralized system. Instead of trying to minimize diversity by imposing blue prints, a central authority provides local governments with the space to experiment and encourages systematic learning and the sharing of lessons from these experiments in developing optimal policies (Sabel and Zeitlin 2008).
Materials and methods
For this case study, we analysed documents in Indonesian and English and interviewed 34 purposively selected key informants. From legal databases, we collected the constitution and all its revisions and amendments, as well as every national law and statute relating substantially to the provision of health services or health insurance passed between 1945 and 2013. We collected minutes of every meeting on constitutional revisions relating to health from Indonesia's upper chamber of parliament and the constitutional court. We reviewed all documents in a database of documentation about health insurance going back to 2003, maintained by the institution that currently manages health insurance nationally. We read all technical reports by the major international organisations supporting Indonesia's move towards UHC, notably the World Bank, Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ), the United States Agency for International Development (USAID) and the Australian Agency for International Development (AusAID). We further reviewed background papers produced by Indonesian academics and lobbyists to inform government policy choices; press reports of discussions, deliberations and contestations; masters and doctoral theses; and publications in peer reviewed journals.
We interviewed people who were involved in, and/or had knowledge about how the processes, institutions and decisions relevant to Indonesia’s progress towards achieving UHC have emerged and evolved and how specific policies were made and implemented; their backgrounds are shown in Table 1. Interviews were conducted in Indonesian (or where requested by the interviewee in English) by three interviewers, using a topic list that was adapted to the specific participant. Interviews were recorded and transcribed, or detailed notes were made during and after the interviews. We triangulated information given by interviewees with the minutes from parliamentary and other meetings which they attended.
Table 1.
Participants interviewed, by employment
| Politician | Researcher | Official | |
|---|---|---|---|
| National government | 3 | 3 | |
| District/provincial government | 3 | 7 | |
| Academic | 11 | ||
| NGO | 2 | 2 | |
| Insurance Industry | 1 | 2 |
Data were analysed iteratively. Documents, interview notes and transcripts were coded manually, jointly discussed by the authors and used to develop a detailed ‘thick’ process narrative, which was checked with the collected data, using the constant comparative method of analysis (Pope et al. 2000).
This study did not require ethical approval according to the appropriate university authorities in Indonesia and the Netherlands. Free and informed consent was obtained from all participants and care has been taken that no comments can be traced back to an individual.
Results
The constitution drafted by Indonesia's founding fathers at independence in 1945 was socialist in tone. Though replaced between 1949 and 1959 by constitutions more palatable to the United States and their allies, it set the agenda for national development. It obliged the state to manage all natural resources, as well as all important sectors of the economy “for the greatest benefit of the people”. Practically, though, the state was not able to provide basic welfare even to the two groups it claimed responsibility for in the constitution: orphans and the destitute. Hyperinflation was the norm and food shortages common. Several provinces were in open revolt against the centre and by the time the aspirational Basic Health Law was passed in 1960, anyone able was grabbing for a civil service job just to get the rations it offered. The ranks of government workers had ballooned to 807 000 by that year, from just 145 000 in the late Dutch period. Civil servants were the only Indonesians with any social security: a pension scheme was carried over from Dutch times, while an “insurance” scheme paid hospital bills for state workers; when they used in or outpatient health services, the cost was docked from their salaries at a rate of 3%.
The Suharto years: meeting immediate political needs
Army general Suharto was inaugurated as Indonesia's second president in 1968, three years after quashing an alleged coup attempt against his predecessor. That same year, his government began to invest significantly in providing the nation-wide health services promised by the 1960 law through primary health centres, known as Puskesmas. The goal was to provide a puskesmas staffed by at least one doctor for every 50 000 people (later reduced to 30 000). Though services were not free, charges were kept low. This provided “access to health” at the most basic level. However, most people had no way of protecting themselves from catastrophically high out-of-pocket spending at higher level facilities such as hospitals in case of serious injury or disease.
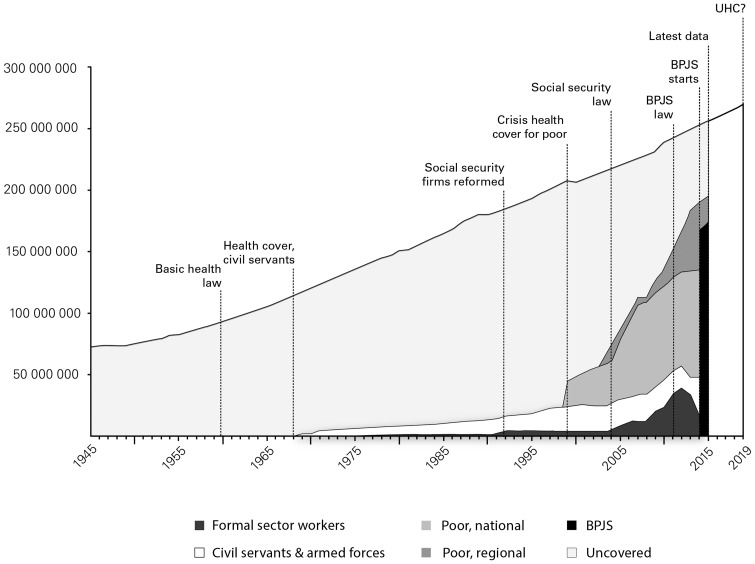
There were important exceptions. In his attempts to restore stability to the nation, Suharto relied very heavily on the military and the highly centralised, Javanese civil service. Health insurance for these two groups and their families was expanded significantly in 1968; it grew into a programme eventually named Askes that had 17.5 million members by 2003 (Figure 1). Also in the late 1960s, the Ministry of Labour had attempted to convert the promises of the Basic Health Law into a real benefit for workers in the formal sector by introducing a contributory health insurance scheme. At the time, the government's economists were trying to boost agricultural production, however; benefits for industrial workers were not a priority and the scheme never got beyond a pilot stage. Despite a revamp in the 1970s, fewer than a million industrial workers were enrolled in the state programme by the end of the decade. Then, in the mid-1980s, the government began to focus on export-led manufacturing as the key to economic growth. Workers moved up the scale in political importance. In 1984 the languishing scheme was expanded to provide health, accident and life insurance as well as pension coverage. Companies with 10 or more employees were obliged either to join the scheme, or to buy insurance from a private firm that provided at least equivalent coverage. Reports of non-compliance were frequent, and the scheme, renamed Jamsostek in 1992, never covered more than a small fraction of those eligible. According to Indonesian health insurance scholars, demand for insurance was limited because Indonesians tend to believe that their fate lies in God's hands. What's more, tales of failure to receive the promised benefits were legion, so people had limited expectations and considered insurance a poor investment.
Figure 1.
Coverage of health insurance schemes for different populations, Indonesia, 1945–2015.
The Jamsostek rebrand coincided with a change of status that affected all four state-owned social security enterprises. These companies, shown by major product and beneficiary group in Table 2, remained state-owned. However in 1992 these previously “public good” corporations became for-profit companies. Rather than reinvest interest and other benefits in their funds, they now paid considerable dividends to the state.
Table 2.
Indonesia's state-owned insurance companies until end-2014, by major product and beneficiary group
| Primary beneficiaries | Health insurance | Pension |
|---|---|---|
| Civil Servants | ASKES | TASPEN |
| Military | ASKES | ASABRI |
| Formal workers | JAMSOSTEK | JAMSOSTEK |
| Informal workers | [can buy from ASKES orJAMSOSTEK] | [can buy from JAMSOSTEK] |
The timing of this change was no co-incidence. Suharto had for many years maintained the balance of power by distributing lucrative monopolies and other business opportunities between the military (which in turn guarantees the stability of his regime) and capital-rich private corporations (whose investment and job-creation skills contributed to economic growth). In the early 1990s, however, his own family became more predatory, sucking up opportunities that would otherwise have gone to the stabilising forces. This happened just as ordinary Indonesians, many now lifted out of poverty, began to demand more opportunities and services. The re-formulated social security funds generated revenue for the government, acting as giant slush funds that were used for political purposes, including buying off potential opponents to Suharto's increasingly shaky regime (Schwarz 1999). They were also used to fund the most basic services. In 1996, the workers' insurer JAMSOSTEK paid the state 50 billion rupiah in dividends (US$22 million) 40% of its after-tax profits3 (Wisnu 2007). The for-state-profit structure and the precedent of using funds for patronage purposes created strongly entrenched interests that shaped the future development of social security in Indonesia.
Shock therapy: the beginning of large-scale social protection
In 1997, an economic meltdown spread rapidly from Thailand across Southeast Asia. The Indonesian rupiah lost three quarters of its value in just six months. Prices rocketed, consumer goods and even food became scarce or unaffordable. According to Sumarto and Bazzi (2011), the percent of Indonesians living in absolute poverty more than doubled within 18 months, hitting 33% and implying an additional 36 million people in desperate financial straits.4 Students took to the streets, protesting against the corruption and inequity of the Suharto regime. When the government announced a hike in fuel prices, other citizens joined them. For the first time in over three decades, the language of citizens' rights rang out in Indonesia's public spaces. In May 1998, Suharto stepped down.
He was succeeded by his technocratic Vice-President, who moved quickly to call elections, as well as to try to mitigate the worst effects of the crisis, supporting education, nutrition and health services for the hardest hit. It was hoped that this would quell unrest, while restoring the legitimacy of the ruling Golkar party. Using a loan from the Asian Development Bank, the government began to issue health cards which allowed poor families to seek free primary health services. Within a year, close to five million Indonesians could access services with these cards (Asian Development Bank 2006). Though some misdistribution of health cards was reported, the pro-poor policies were largely successful in ensuring that the most vulnerable could access at least outpatient services.
The social protection policies did not, however, protect the ruling party. Suharto's downfall and the subsequent elections led to the euphoric embrace of the concept of citizens' rights on the part of Indonesians who had heard about nothing other than their responsibilities for more than three decades. In 1999, in the first truly democratic elections in nearly 45 years, Indonesians favoured the PDI-P party led by Megawati Sukarnoputri, which had campaigned on a platform of increased equity.
The following year, the new parliament amended the 1945 constitution to include the “right to receive medical services”. Two years later, a further constitutional amendment specified that the state was responsible for ensuring health service provision, as well as for developing a social security system for all citizens. The next clause, reminiscent of the declaration of independence, stated that the details would be worked out later. PDI-P leader Megawati, then Vice-President, set about working out the details. An unwieldy working group of over 60 people drafted a social security law that, in its first version, envisaged the fusion of all four state-owned insurance firms into a single entity, which would operate as a single payer, not-for-profit trust fund. Minutes of meetings and interview accounts show that this was hotly contested, not least by the existing insurance firms and those who benefited from the profits they generated. Besides being reluctant to lose their cash cows, directors of state firms were reportedly concerned that the restructuring would open their books to public scrutiny. Employers were afraid that the plan would raise costs, partly because they could no longer opt out of the state-run scheme. They argued that the mandatory schemes violated human rights. Private sector employees and some labour unions also opposed the draft bill, because under the new structure, workers' would have to contribute to premiums formerly covered entirely by employers. What's more, they worried that premiums paid by workers and employers would be used to subsidise services for the poor and unwaged, leading to a cut in benefits for those in work. Advisors favouring private sector interests, including from the United States, objected to the fact that the state would have a virtual monopoly on provision of social insurance (Wisnu 2007; Thabrany 2008; Marzoeki et al. 2014). The bill was reportedly revised 56 times before a draft was submitted to parliament in January 2004.
Press reviews reveal very little public attention to the social security law over those years of consultation, contestation and negotiation. It was only after the draft bill was submitted to parliament that it came to wide public attention; that led to yet more contestation, not least from newly-empowered districts who felt the bill was an attempt to re-centralise power. Supporters of rival models organised demonstrations in front of the national parliament and elsewhere, prompting considerable news coverage.
Interviews as well as a comparison of proposed drafts show that this new wave of discordant debate led to a further gutting of the bill. Lobbying of parliamentarians and back-room deal-making continued to be important mechanisms, but numerous press statements backing one or other position indicate that public grand-standing was important in this phase also. In the final iteration, all four state insurers were mentioned as participants in the eventual social security system, a triumph for the status quo. Many of the more contentious issues were simply side-stepped. The 2004 law, which contained virtually no details of contribution levels, co-payment percentages, benefits packages or sanctions, stipulated that these should be established by follow-up legislation. It listed the need for 11 presidential instructions, 10 government regulations and one national law. The latter, which was to detail the structure and administrative procedures of the still only vaguely-delineated social security system, had to be passed within five years (Republic of Indonesia, Ministry of Health 2004).
Though Megawati had taken over as President when her predecessor was impeached in 2001 with social security reform very high on her list of priorities, it had taken another three years of wrangling before all the interest groups involved agreed on a final bill. She signed it into law in an unprecedented high-profile ceremony on her very last day in office. Megawati's support for a national social security system was not enough to secure her re-election by an electorate disappointed by her generally sluggish leadership; rather, it was to become her legacy. A member of the bill drafting committee, wrote about the ceremony: “By [signing the bill], she would like to tell the Indonesian people 'I produced this Act as a gift for you'.” (Thabrany 2008)
Decentralisation and local experimentation
While working groups in Jakarta thrashed out constitutional amendments and social security laws, the rest of Indonesia had undergone a quiet political revolution. In order to relieve pressure that had been building against decades of centralised rule that seemed to suck resources from other islands for the benefit of overcrowded Java, Indonesia decentralised. From 2001, responsibility for most of the functions of state devolved to the district level, which was expected to allocate funds according to local needs from unrestricted block grants provided by the centre. This gave local governments unprecedented leeway for policy experimentation. The devolution came at exactly the time that external funding for emergency health service provision for poor families dried up. Democratically elected politicians quickly found that they were not easily able to withdraw services that people had come to rely on. The pioneering district of Purbalingga in Central Java in 2001 assumed the challenge of providing health services for poor people by providing capitation funds to primary health service providers and the district hospital. The central government sought to encourage this type of experimentation by providing top-up funding (derived partly from savings on reduced fuel subsidies) to selected district governments under a programme called JPK Gakin.
The involved districts responded differently; some aimed for universal coverage, with well-off citizens paying premiums and the government picking up the tab for the poor, while others sought only to provide services for the poor. Services were paid for on a capitation basis in some areas, through fee for service in others. In rural areas, governments sometimes paid participants' transport costs to encourage service use. Many other local adaptations contributed to the perceived success of the devolved approach during an initial trial in 25 districts; locally run schemes were also found to be more responsive to the needs of users than the previous centrally-administered ‘poor card’ scheme, leading to higher uptake of services by poor people (Arifianto et al. 2005).
Probably the most celebrated of the local schemes was in the Balinese district of Jembrana, one of the island's poorest areas. There, Gede Winasa – a political outsider – came to power in 2000 through what Rosser and colleagues term “political entrepreneurship”: he quietly convinced members of the local parliament (who at that time elected the district head) that their interests would be best served by providing decent services to the local population, rather than by pandering to party elites. Himself a dentist who had worked in local health departments, he had firm ideas about how health services should be provided, and determined to put them into practice. From 2003, Jembrana district paid for outpatient services for all residents and hospitalisation for the poor at any registered provider, public or private. This was funded in part by cuts in civil service positions. Though ultimately unsustainable financially, evaluators agree that it greatly increased the quality as well as the quantity of health services for residents; infant mortality dropped by nearly half in the first year of the programme (Jakarta Post 2005). Perhaps more importantly, it contributed to Winasa's landslide victory in the first direct elections for district head – he won 90% of the popular vote – and catapulted him onto every TV station, and the front cover of Indonesia's leading news weekly, Tempo, as “Man of the Year”. A well-funded district health scheme suddenly became the must-have political programme for aspiring local politicians.
National capture: the centre appropriates local efforts
These local successes did not go unnoticed by Jakarta. Just a few days after being appointed Minister of Health in October 2004, Siti Fadilah Supari declared that the government would pay for inpatient services for all poor people in Indonesia. Insiders report that the controversial cardiologist, representing a minority party whose support the new president sought, seemed unaware of the newly-minted social security law when she made this promise. She showed no sign that she was aware that in the current decentralised set-up, the central government had no power to instruct districts who to care for, or how. Other observers suggest that her apparent naiveté was a cover for a deliberate move to re-consolidate power at the centre.5 Advisors quickly huddled to find ways to deliver on the minister's promise. They suggested using the social security law, passed just days earlier, as a legal basis, a nationwide expansion of the JPK Gakin ‘pilot programme’ as a vehicle, and the civil service health insurance provider PT ASKES as an implementing agency. The minister quickly passed a decree instituting just such a system, beginning on January 1 2005, in less than two months’ time (Witoelar 2004; Thabrany 2008). The programme, rebranded ASKESKIN, provided capitation payments to primary health centres and fee-for-service reimbursements to hospitals for inpatient care.
This move struck at the very core of the power relationships that were newly emerging since decentralisation began. Districts which had been running their own health schemes successfully were angered by what they saw as a reverse take-over by the central government; they felt that they would lose the very flexibility that allowed them to meet local needs, and in some cases would see services reduced to a nationally standardised package (Arifianto et al. 2005). Political opportunists may also have been disappointed that the selection of beneficiaries and administration of pooled insurance funds was being taken out of their hands. Certainly, some local politicians resented seeing a programme that was considered an important electoral asset in district polls hijacked by the national government. The East Java province and Rembang district governments went so far as to challenge the social security law in the Constitutional Court, saying that it violated districts' constitutional right to choose their own service providers. Though the Constitutional Court upheld the 2004 law, they also ruled that district governments could run local health schemes to supplement the national scheme, expanding coverage or benefits, for example (Mahakam Konstitutsi, Republik Indonesia 2005).
The national scheme managed by ASKES immediately ran into trouble. Registration was chaotic, and people complained that participants selected on the basis of data held at the national level were often not the poorest.6 The scheme, which for the first time covered hospitalisation for the poor, undoubtedly increased demand for services, and the country's health system, already strained, struggled to cope. Poor administration delayed reimbursements, leading hospitals to turn away patients enrolled in the scheme. The health minister's cell phone overflowed with text messages from dissatisfied customers. Instead of reaping the political benefits of expanded insurance, the central government was being demonised (Thabrany 2008). In 2008, one year to the next general election, Siti Fadilah restricted ASKES's role to managing recruitment, and the Ministry of Health took over provider payment for the scheme, now renamed JAMKESMAS. Jakarta began once again actively to encourage local governments to provide health insurance schemes for the poor and near-poor not reached by the national programme. The number of district programmes, known as JAMKESDA, swelled from around 60 in 2008 to at least 245 in 2012.7 Some far exceeded the national standards in the benefits they provided. In Aceh province, for example, every citizen was entitled to free in-patient care; the local scheme even covered treatment overseas in some cases.
At the national level, progress in implementing the 2004 social security law was sluggish. Controversial from the start, and seen as very much an initiative of Megawati and the PDI-P party, the law was not prioritised by her successor as president, Susilo Bambang Yudhoyono. Though he did issue a decree in 2008 appointing members to the national social security council (DSJN) envisaged by the 2004 law, advisors to politicians involved in the process told us in interviews that the powerful position of chair was contested, operational funds were short and little progress was made. As the 2009 deadline for the passage of a further implementing law approached and it seemed as though Indonesia's social security ambitions might never be implemented, parliamentarians and civil society groups both became more active. Rather than wait for the DSJN to propose a new law, PDI-P parliamentarians started drafting a version of the bill. Meanwhile, influential academics, research organisations and think tanks began to scrutinise existing social insurance efforts and make their findings public. By this time, UHC was already something of a buzzword among international development organisations; several of them (including AusAID, USAID and GIZ) provided funding for these studies, though no interviewees reported that the views of foreign development agencies significantly influenced the shape or outcome of domestic discussions. An umbrella group of labour and citizens' organisations called KAJS (the Action Committee on Social Security) lobbied parliament and the executive for action (Wisnu 2007).
Forced march: civil society pushes forward action
After the 2009 deadline for the passage of a new law passed, KAJS filed a lawsuit against the president and several ministers, accusing them of breaching the constitution and the 2004 social security law by failing to implement mandated reforms (Wisnu 2011). The court sided with the activists, ruling in June 2011 that the government must act immediately to pass necessary legislation to implement the law.
Discussions about the bill became more heated, according to those who participated and the minutes of the meetings. Though dozens of studies had examined actuarial needs, the burden of disease, the fiscal implications of financing models and other technical aspects of policy options, these were barely considered in the negotiation process; this was a source of considerable frustration to some of our interviewees. Instead, the focus was on institutional arrangements (Aspinall 2014). Existing insurers (and the politicians and bureaucrats who benefited from the funds they controlled) continued to lobby against the mandated reforms, arguing that they would disrupt a system that was currently working well. The employers argued against mandatory participation, while labour groups objected to the contributory nature of the scheme, which they said transformed social security from a right into an obligation. The former health minister Siti Fadilah Supari weighed in, saying mandatory health insurance would be unfair to the poor, who couldn't pay the premium. All these groups wanted to maintain the status quo, restricting changes to new participants, and they expressed their opinions not just in parliamentary discussions but also in the press and public fora (Abimanyu 2011; Damanik 2011; Gresnews 2011; Sijabat 2011). Parliamentarians, on the other hand, newly responsive to an electorate ever more aware of its rights, pushed for a more radical bill that maintained the non-profit principles of the 2004 law and that laid out in detail the rights and obligations of all parties (Abimanyu 2011). Eventually, in November 2011, a new law was passed mandating BPJS, the ‘Social Security Administering Body’. Instead of the single social security body favoured by parliament, it created two. Essentially, the health insurance corporation ASKES would be transformed into a non-profit trust fund called BPJS Health, while the workplace insurer JAMSOSTEK would administer pensions, life and workplace insurance in its new guise, BPJS Workforce. Assets, liabilities, participants and staff of the corporations were automatically transferred to the new bodies. BPJS Health would from the time of its initiation in January 2014 take on participants from the existing health insurance schemes for workers, the military and the nationally-determined poor. The premiums for the latter group would continue to be paid by the state. The status of clients of private providers, district/provincial health insurance schemes and informal workers was not clear, but the law implied that they would be subsumed into BPJS Health over time (Republic of Indonesia 2011).
Within just over two years of the passage of this highly contested law, BPJS Health came into being. Details continued to be worked out; in the first 18 months of its operation, 29 presidential, ministerial or government regulations were issued governing the details of the fund's operation (BPJS database). An analysis of the current functioning of the scheme is beyond the scope of this paper, but many challenges clearly remain. They include the need to develop an affordable and appropriate benefits package, expand service provision and encourage the regular payment of premiums by the non-poor, around half of whom do not currently contribute as the law requires. Further, the pool of funds that BPJS is generating (12 trillion rupiah in assets at the end of 2014, or just less than US$1 billion for BPJS Health alone) is a magnet for contestation. In 2015, for example, the influential Moslem organisation MUI declared BPJS “haram” because it does not comply with Islamic banking principles. The move was widely seen as a bid to channel funds into financial institutions with links to MUI (Jakarta Globe 2015). Meanwhile, politicians at all levels of government – beginning with President Joko Widodo who came to power after BPJS was in operation – are now trying to claim credit for the expansion of health coverage8 (Asril 2014; Sari 2014; Tarigan 2014).
Discussion
While much attention has been paid to the technical challenges of achieving universal health coverage in low and middle income countries, those challenges cannot be divorced from the particular social, political and institutional circumstances of each country that faces them. The vast and diverse nation of Indonesia established the legal underpinnings for providing health services to its people as early as 1960, but it was not until over half a century later that the goal was transformed from Quixotic aspiration to real possibility.
Observers of other Southeast Asian countries have noted the importance of bureaucrats in pushing the health reform agenda; their findings mirror similar histories in Latin America (Nunn 2009; Wisnu 2011; Gómez 2012; Harris 2015). Harris speaks of “developmental capture”, a process through which technocrats mobilise social and political networks at home and abroad to achieve reform in the face of conservative opposition. In China, technocrats partnered with academics to develop an evidence base which could be used to drive health reform when a political opportunity arose (Sun et al. 2010). The pathway towards affordable health care for all Indonesians has been more haphazard than is suggested by the experience of these other countries. Progress has been marked by political opportunism, experimentation, compromise and sheer coincidence.
The health insurance and wider social security system has developed iteratively to meet the political priorities of the day. In the 1960s and 1970s, civil servants and the military were key to national stability, and were provided for. As manufacturing became economically important in the 1980s, health insurance for workers rose up the agenda. Insurance bodies were restructured to provide slush funds for an embattled leadership in the early 1990s. The need to stave off social unrest following the financial and political meltdown at the end of that decade led to the first provision of health cover for the poor, at first using a social protection model.
During the long years of military rule, when decisions were dictated from the top and enforced by armies of soldiers and bureaucrats, citizens had virtually no influence on policy pathways. After Suharto stepped down and truly democratic elections were introduced, however, the relationship between citizen and state changed and a new form of path dependency emerged. For the first time in over four decades, actions taken by the state could affect voter behaviour in ways that might affect future policy choices. Indonesians enthusiastically adopted the rhetoric of human rights and welfare; in an atmosphere coloured by the notion that it was time for former elites to pay their debts to society, they began to demand that the state guarantee both. When the state provided free basic healthcare for the poorest Indonesians in the crisis years of the late 1990s, it set a precedent that was hard to step back from, even though uptake of those early services was not high. This early step, followed by the local experimentation discussed below, foreclosed the option of ‘business as usual’ in the provision of health coverage. Once Indonesians saw that the state could assure affordable health, the path was set: citizens began to demand health cover age, and politicians increasingly delivered. It is notable that the national parliament, regularly cited in opinion polls as among the most corrupt institutions in Indonesia, responded to pressure from civil society, pushing through social security reforms that undermined the entrenched interests of the bureaucracy (Ronoduwu 2013).
In terms of experimentalist governance, the Indonesian case provides an interesting perspective. Descriptions of experimentalist governance in Europe speak of a process in which technocrats propose policy options which are implemented flexibly in different political situations, then collectively evaluated to develop shared lessons (Sabel and Zeitlin 2008). In Indonesia, the limited technical input that did exist at the design stage, was largely commissioned to justify or validate local initiatives. Most early district schemes were developed at the initiative of individual ‘democratic entrepreneurs’ who had been appointed to the powerful position of district head by local parliaments. Controlling their own health budgets and provided with virtually no guidance by the central government, these innovative district heads tried out various models to increase access to health care. Several of these schemes were substantially implemented just as direct elections for district head were introduced: another critical juncture in citizen-state relations. Successful models drew the attention of the press, and political candidates around the country began promising similar programmes in their election campaigns.
In setting up local and indeed national schemes, winning candidates sometimes drew on advice from researchers in academic institutions to help them implement their promises. But because the earliest experiments in health coverage were largely unforeseen, there was little central guidance of the experimentation, and no pre-planned systems through which learning was to be captured and exchanged. Remarkably few of the ‘lessons learned’ have been based on rigorous evaluation of service use. The use of technical analysis has remained rather limited even as local models were adapted and expanded for use at the national level. The Indonesian case, similar to that described by Agyepong and Adjei in Ghana, suggests that political priorities trump technical considerations in the ongoing implementation of health financing models as well as in their design (Agyepong and Adjei 2008).
The recentralisation of health financing under BPJS and the provision of standard service packages will reduce local politicians’ room for manoeuvre in using health coverage as part of their electoral arsenal. Though participants in local health schemes are supposed to be integrated into the national scheme by the end of 2016, local governments are still responsible for service provision. The more active district ‘democratic entrepreneurs’ will doubtless find ways to appeal to voters by improving service quality. However other politicians may be content to deflect discontent with health services on to the national BPJS brand that will be foremost in consumers' minds. In these cases, local accountability may be reduced and progress towards better service delivery may falter. Central involvement also has positive effects, however. For example, large-scale national programmes for previously un-insured populations have allowed the government to set new parameters with insurers and service providers (such as a move away from fee-for-service payment in favour of capitation and/or diagnostic groups) that would have been hard to negotiate for existing clients or in smaller schemes.
Many financial, technical and political hurdles still stand between Indonesia and its goal of affordable health care for all. The rapid expansion of insurance coverage has created demand which cannot be met by the current health system (Bredenkamp et al. 2015). Service quality is already extremely poor in many areas and citizens are increasingly expressing their discontent with services that they were until recently not even able to contemplate using. A nationally standardised contribution system and putative benefits package effectively creates inequity, because service availability is so very unequal, and there will certainly be more push-back from local governments against excessive centralisation of decision-making. Besides the service provision, cost containment will be a major challenge, and with so many funds concentrated in one pot, corruption scandals are likely.
As Indonesia consolidates its democracy, the demands that citizens make of their service providers and their capacity to press effectively for improvement are both likely to increase. The habit of passing imprecisely-worded laws that allow for iterative policy making and on-the-job learning has served the country well so far, eventually resulting in solid and probably irreversible political backing for universal health coverage. However to meet the many challenges inherent in actually delivering affordable health care to all Indonesians by 2019, the country needs to strengthen its capacity for rigorous evaluation and policy learning at national and local levels, and draw more deeply on technical evidence to guide implementation of its ambitious plans.
Conclusion
Indonesia's journey towards universal health coverage has been determined largely by domestic political concerns – different groups obtained access to healthcare as their socio-political importance grew. A major inflection point occurred following the Asian financial crisis of 1997. To stave off social unrest, the government provided health coverage for the poor for the first time, creating path dependency that influenced later policy choices. The end of this programme coincided with decentralisation, leading to experimentation with several different models of health provision at the local level. When direct elections for local leaders were introduced in 2005, popular health schemes led to success at the polls. UHC became an electoral asset, moving up the political agenda. The Indonesian experience underlines the value of policy experimentation, and of a close understanding of the specific contextual and political factors that drive successful UHC models at the local level. While technical considerations took a back seat to political priorities in developing the structures for health coverage nationally, they will have to be addressed going forward to achieve sustainable health coverage for all Indonesians.
Acknowledgements
The authors would like to thank all those who were interviewed and contributed their views to this paper. Thanks to Agung Nugroho and other Migunani staff for their assistance in data collection. Roland Bal, Ward Berenschot, Menno Pradhan, Marcus Mietzner, Laksono Trisnantoro and Eddy van Doorslaer provided helpful comments on a draft of this paper.
Funding
This work was supported by Research Excellence and Innovation Grant of Erasmus University Rotterdam.
Notes
England (without Scotland or Wales). measures 130,000 km2, to Java's 129,000.
Calculated by the World Bank using purchasing power parity. The most recently reported figure is for 2011.
Indonesian's National Audit Agency has frequently reported irregularities at JAMSOSTEK. In 2006, Achmad Djunaedi, finance director of the state insurer from 1983 to 1994 and Director General from 1999-2004, was sentenced to eight years in prison for illegally investing JAMSOSTEK money in private companies.
These data are calculated using consistent measures over time. They differ from official figures; in 1998, the Indonesian statistics bureau BPS changed the way poverty was measured.
We thank an anonymous reviewer for this observation.
An extreme case was Melinda Dee, a banker who was jailed for embezzling 17 billion rupiah from her clients at Citibank. She argued that Jamkesmas should pay for an operation to reverse a botched breast implant, because she was a ward of the state. Though she ultimately did not prevail, high profile stories like this undermined public confidence in the programme.
Out of close to 500 districts, some 262 responded to a 2012 survey by the SMERU research institute; 245 of them reported running a local health scheme for the poor. (Aspinall 2014).
As governor of Jakarta, Joko Widodo rebranded his predecessor's health insurance scheme, issuing "Healthy Jakarta Cards" in the colours of the national flag to poor families who could then use public health facilities in the capital for free. In his 2014 presidential campaign, he promised to extend this programme nationwide by issuing "Healthy Indonesia Cards". These can be used nationwide, but are otherwise identical to BPJS cards, and indeed are issued by BPJS.
References
- Abimanyu A. 2011. Pro-kontra Keberadaan BPJS. Kompas.
- Agyepong IA, Adjei S. 2008. Public social policy development and implementation: a case study of the Ghana National Health Insurance scheme. Health Policy and Planning 23: 150–60. [DOI] [PubMed] [Google Scholar]
- Arifianto A. et al. 2005. Making Services Work for the Poor in Indonesia: A Report on Health Financing Mechanisms (JPK-Gakin) Scheme in Kabupaten Purbalingga, East Sumba, and Tabanan, Jakarta: SMERU. [Google Scholar]
- Asian Development Bank. 2006. Social Protection Sector Development Program in Indonesia (Loans 1622/1623-INO), Manila: ADB Independent Evaluation Department. [Google Scholar]
- Aspinall E. 2014. Health care and democratization in Indonesia. Democratization 21: 803–23. [Google Scholar]
- Asril S. 2014. Jokowi Lebih Baik Integrasikan Kartu Indonesia Sehat dengan BPJS. Kompas [Google Scholar]
- Pusat Statistik B. 2015. Statistik Indonesia 2015, Jakarta: BPS. [Google Scholar]
- Boerma T. et al. 2014. Monitoring progress towards universal health coverage at country and global levels. PLoS Medicine 11: e1001731.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredenkamp C. et al. 2015. Emerging challenges in implementing universal health coverage in Asia. Social Science & Medicine 145: 243–48. p [DOI] [PubMed] [Google Scholar]
- Cotlear D. et al. 2015. Going Universal: How 24 Developing Countries are Implementing Universal Health Coverage from the Bottom Up, The World Bank. [Google Scholar]
- Damanik C. 2011. Siti Fadilah: Tolak RUU BPJS. KOMPAScom.
- Dwicaksono A, Nurman A, Prasetya PY. 2012. Jamkesmas and district health care insurance schemes: assesment reports from 8 districts/municipalities and 2 provinces Cetakan pertama., Bandung: Perkumpulan Inisiatif. [Google Scholar]
- Gómez EJ. 2012. Pursuing centralization amidst decentralization: The politics of Brazil’s innovative response to HIV/AIDS. Journal of Politics in Latin America 3: 95–126. p [Google Scholar]
- Gresnews, 2011. Pemerintah setengah hati transformasi 4 BUMN asuransi. gresnews.com Available at: http://www.gresnews.com/berita/sosial/93197-pemerintah-setengah-hati-transformasi-4-bumn-asuransi/, accessed 18 October 2015.
- Harris J. 2015. “Developmental Capture” of the state: explaining Thailand’s universal coverage. Journal of Health Politics, Policy and Law 40: 165–93. [DOI] [PubMed] [Google Scholar]
- Globe J. 2015. MUI Declares National Health Insurance Program Haram. The Jakarta Globe [Google Scholar]
- Post J. 2005. Jembrana seeks to improve people’s living standard. Jakarta Post [Google Scholar]
- Kementerian Kesehatan Republik Indonesia , 2015. Profil Kesehatan Indonesia Tahun 2014, Jakarta: Ministry of Health, Republic of Indonesia.
- Lagomarsino G. et al. 2012. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. The Lancet 380: 933–43. p [DOI] [PubMed] [Google Scholar]
- Mahakam Konstitutsi, Republik Indonesia 2005. Putusan Perkara Nomor 007/PUU-III/2005, Jakarta.
- Mahoney J. 2000. Path dependence in historical sociology. Theory and Society 29: 507–48. [Google Scholar]
- Marzoeki P. et al. 2014. Universal Health Coverage for Inclusive and Sustainable Development Universal Health Coverage for Inclusive and Sustainable Development, Jakarta: World Bank. [Google Scholar]
- Mboi N. 2015. Indonesia: on the way to universal health care. Health Systems & Reform 1: 91–97. [DOI] [PubMed] [Google Scholar]
- Kesehatan Republic of Indonesia 2004. Keputusan Menteri Kesehatan Republik Indonesia nomor 1241/MENKES/SK/XI/2004 tentang Penugasan PT Askes (Pesero) dalam pengelolaan program pemeliharaan kesehatan bagi masyarakat miskin.
- Nunn A. 2009. The Politics and History of AIDS Treatment in Brazil, Springer Science & Business Media. [Google Scholar]
- Pigazzini A. et al. 2013. The nuts and bolts of Jamkesmas - Indonesia’s government-financed health coverage program for the poor and near-poor, The World Bank. [Google Scholar]
- Pisani E. 2013. Medicine for a sick system. Inside Indonesia 111. [Google Scholar]
- Pope C, Ziebland S, Mays N. 2000. Analysing qualitative data. BMJ 320: 114–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich MR. et al. 2015. Moving towards universal health coverage: lessons from 11 country studies. The Lancet 387: 811–16. [DOI] [PubMed] [Google Scholar]
- Republic of Indonesia, 2012. Peta Jalan Menunju Jaminan Kesehatan Nasional 2012 - 2019, Jakarta.
- Republic of Indonesia, 1945. The 1945 Constitution of the Republic of Indonesia.
- Republic of Indonesia, 2011. Undang-Undang No. 24 Tahun 2011 tentang Badan Penyelenggara Jaminan Sosial.
- Republic of Indonesia, 2004. Undang-undang Republik Indonesia Nomor 40 Tahun 2004 Tentang Sistem Jaminan Sosial Nasional.
- Republic of Indonesia, Ministry of Health , 2004. Profil Kesehatan Indonesia Tahun 2004. [Google Scholar]
- Rodin J, de Ferranti D. 2012. Universal health coverage: the third global health transition? The Lancet 380: 861–62. p [DOI] [PubMed] [Google Scholar]
- Rokx C. et al. 2009. Health financing in Indonesia : a reform road map, The World Bank. [Google Scholar]
- Ronoduwu O. 2013. Erratic Indonesian Legislature Stirs Anger, Mockery. Reuters Available at: http://www.thejakartaglobe.com/home/erratic-indonesian-legislature-stirs-anger-mockery/436760, accessed 14 March 2013.
- Rosser A, Wilson I, Sulistiyanto P. 2011. Leaders, Elites and Coalitions: The Politics of Free Public Services in Decentralised Indonesia, The Developmental Leadership Program. [Google Scholar]
- Sabel CF, Zeitlin J. 2008. Learning from difference: the new architecture of experimentalist governance in the EU. European Law Journal 14: 271–327. p [Google Scholar]
- Sari K. 2014. Ahok: KIS dan BPJS Kesehatan Mirip, Hanya KIS Itu Bahasa Politiknya Saja - Kompas.com Megapolitan. Kompas.
- Savedoff WD. et al. 2012. Political and economic aspects of the transition to universal health coverage. The Lancet 380: 924–32. p [DOI] [PubMed] [Google Scholar]
- Schwarz A. 1999. A Nation in Waiting : Indonesia’s Search for Stability 2 edition., Westview Press. [Google Scholar]
- Sijabat RM. 2011. House slams govt for stalling BPJS bill talks. The Jakarta Post [Google Scholar]
- Simmonds A, Hort K. 2013. Institutional analysis of Indonesia’s proposed road map to universal health coverage’. Health Policy and Health Finance Knowledge Hub Working Paper, 33.
- Steinmo S. 2008. Historical institutionalism In Della Porta D., Keating M., eds. Approaches and methodologies in the social sciences. Cambridge: Cambridge University Press, p. 118. [Google Scholar]
- Sumarto S., Bazzi S. 2011. Social protection in Indonesia: Past experiences and lessons for the future. MPRA Paper No. 57893. Available at: https://mpra.ub.uni-muenchen.de/id/eprint/57893, accessed 18 October 2015. [Google Scholar]
- Sun X. et al. 2010. Evolution of information-driven HIV/AIDS policies in China. International Journal of Epidemiology 39(Supplement 2): 4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarigan M. 2014. BPJS : Kartu Indonesia Sehat Hanya Brand Baru | Tempo Nasional. Tempo [Google Scholar]
- Thabrany H. 2008. Politics of National Health Insurance of Indonesia: A New Era of Universal Coverage. In 7th European Conference on Health Economics. Rome.
- Wisnu D. 2011. Governing Insecurity in Indonesia and Philippines: The Politics of Social Protection Reform. Available at: http://portal.kopertis3.or.id/handle/123456789/1951, accessed 16 October 2015.
- Wisnu D. 2007. Governing Social Security: economic crisis and reform in Indonesia, the Philippines and Singapore. The Ohio State University. [Google Scholar]
- Witoelar W. 2004. Rakyat Miskin Gratis Berobat. Perspektif Baru 457. [Google Scholar]