Supplemental Digital Content is available in the text
Keywords: meditation, motor control exercise, movement-related fear, neuromatrix, pain catastrophizing
Abstract
People with chronic musculoskeletal pain often experience pain-related fear of movement and avoidance behavior. The Fear-Avoidance model proposes a possible mechanism at least partly explaining the development and maintenance of chronic pain. People who interpret pain during movement as being potentially harmful to the organism may initiate a vicious behavioral cycle by generating pain-related fear of movement accompanied by avoidance behavior and hyper-vigilance.
This study investigates whether an individually adapted multifactorial approach comprised of biopsychosocial elements, with a focus on physical exercise, mindfulness, and education on pain and behavior, can decrease work-related fear-avoidance beliefs.
As part of a large scale 10-week worksite randomized controlled intervention trial focusing on company initiatives to combat work-related musculoskeletal pain and stress, we evaluated fear-avoidance behavior in 112 female laboratory technicians with chronic neck, shoulder, upper back, lower back, elbow, and hand/wrist pain using the Fear-Avoidance Beliefs Questionnaire at baseline, before group allocation, and again at the post intervention follow-up 10 weeks later.
A significant group by time interaction was observed (P < 0.05) for work-related fear-avoidance beliefs. The between-group difference at follow-up was –2.2 (–4.0 to –0.5), corresponding to a small to medium effect size (Cohen's d = 0.30).
Our study shows that work-related, but not leisure time activity-related, fear-avoidance beliefs, as assessed by the Fear-avoidance Beliefs Questionnaire, can be significantly reduced by 10 weeks of physical-cognitive-mindfulness training in female laboratory technicians with chronic pain.
1. Introduction
The influencing factors of health plasticity encompass determinants across a wide spectrum of elements. These elements range from social and mental resources and resilience to biomedical research and regarding physical health, from musculoskeletal pain and longevity affected by the environmental setting to the behavioral response to these elements.[1–3] Chronic musculoskeletal pain is not only a major socioeconomic burden [4] but is also affected by social inequalities and available resources.[5,6] In the working environment, there are often differences in both physiological measures of fitness, muscle strength, and cardiovascular and metabolic risk factors that contribute to overall health and mortality risk.[7–10] However, a common trait across blue- and white-collar workers in Denmark is that pain is experienced regardless of job occupation, age, and gender.[11] It is well known that occupationally derived musculoskeletal pain is often present in job tasks involving low-force, static, or quasi-static repetitive and monotonous movements (such as the work of laboratory technicians),[12] but a single factor model of structure and biomechanics cannot sufficiently explain why some people who experience pain develop severe chronicity whereas others do not. Thus, a behavioral/psychological aspect cannot be ignored when explaining pain on a broader scale in relation to health and mortality.
Currently, chronic pain is explained as a multifactorial experience comprised of biological, psychological, and social elements that affect the perception of nociceptive stimuli and ultimately produce the final outcome of pain/no pain.[13] The neuromatrix theory of pain [14–17] and the cognitive detection of movements possibly threatening and harmful to tissue have led to the current definition of pain by the International Study of Pain (IASP) as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.[18] This definition has brought attention to fear as a psychological factor greatly influencing chronic pain.[19–22] The literature shows a multitude of physiological mechanisms by which injuries lead to nociceptive responses and ultimately to pain, but the brain does not always perceive nociceptive signals as pain, and not every painful sensation begins with nociception.[23] This points toward a centrally governed control mechanism that ultimately determines whether a stimulus is perceived as painful.[23–27]
Almost everyone will experience acute pain during the course of their lifetime, but only a fraction of those who experience acute pain develop chronic pain. People suffering from persistent chronic pain may also experience pain-related fear (PRF) of movement. PRF can best be defined as the fear that emerges when stimuli related to pain are perceived as a threat.[19] The fear response exhibited comprises psycho-physiological (e.g., increased muscle tension, altered muscle metabolites, and sympathetic nervous system activity), behavioral (e.g., escape and avoidance behavior), and cognitive (e.g., catastrophizing thoughts) elements. Thus, the fear of experiencing pain, fear of performing work-related activities, fear of general movement, and fear of sustaining injury have been described as often occurring in patients suffering from chronic pain.[20,19,28]
The Fear-Avoidance model proposed by Vlaeyen et al, assessed by a questionnaire on fear-avoidance beliefs (FAB), proposes a possible mechanism at least partly explaining the development of chronic pain.[29] The basic tenet of pain perception is that the way in which pain is processed and interpreted leads to the activation of different pathways that ultimately determine whether the pain felt is harmful and subsequently becomes chronic. People who interpret pain as nonthreatening to the organism will likely remain actively engaged in normal day activities (work, sports, recreational activities), which may promote functional recovery via cognitive mechanisms, such as pain-decatastrophizing behavior, as well as physiological mechanisms mediated by muscular activity and overall body movement. Conversely, patients who display an inappropriate response to pain and perceive movement as potentially harmful to the organism may initiate a vicious behavioral cycle, as the misinterpretation generates PRF of movement accompanied by escape/avoidance behavior and hypervigilance.
George and colleagues investigated the effect of a fear-avoidance-based physical therapy intervention in 66 patients with acute low back pain, lasting <8 weeks, and compared it to standard care physical therapy. The measured parameters were disability, pain intensity, and FAB. After a 4-week intervention and a 6-month email-based follow-up, the results showed that the patients with heightened FAB at baseline had less disability and lower FAB after receiving fear-avoidance-based physical therapy compared to standard care physical therapy. Intriguingly, patients exhibiting less FAB appeared to have more disability after receiving fear-avoidance-based physical therapy when compared to the standard care.[30] In another recent study, the influence of FAB on disability in patients with subacromial shoulder pain was analyzed by Kromer and colleagues.[31] They found through a correlation analysis of FAB that catastrophizing behavior and shoulder disability were present in 90 patients and that FAB are a significant contributor to baseline disability but interestingly not to disability change scores after 3 months of follow-up.[31] A qualitative review of the literature concerning the occurrence of fear-avoidance- versus endurance-related pain responses by Hasenbring and Hasenbring and Verbunt[32] showed that patients with an inappropriate response to pain will develop more pain prospectively and show higher levels of specific strain postures, quantified by accelerometry, than patients showing adaptive pain responses. This could indicate that there is a physical manifestation of the hyper-vigilance associated with fear-avoidance. In another recent systematic review, Wertli and colleagues concluded that FAB are a prognostic indicator for poor outcomes in subacute low back pain and that early intervention-based treatments to reduce FAB may support recovery.[33] Based on the current literature on FAB, it is evident that only a few randomized controlled trials with novel intervention-based treatments targeted at work-related FAB (in an occupational setting) to assist in chronic musculoskeletal pain rehabilitation of the neck, shoulders, upper and lower back, elbow, and hand have been conducted.
The aim of this study is therefore to investigate the effects of a physical-cognitive-mindfulness intervention on work-related FAB in a group of female laboratory technicians suffering from chronic musculoskeletal pain in the neck, shoulders, upper and lower back, elbows, and hands. Based on the multifaceted theory of chronic musculoskeletal pain and its associated disability, we hypothesize that an individually adapted multifactorial approach comprised of biopsychosocial elements that focuses on physical exercise, mindfulness and education on pain, fear-avoidance, and catastrophizing behavior can decrease work-related FAB but not leisure time FAB compared to ongoing company initiatives, as we theorize a context-specificity of FAB, and the intervention is limited to the occupational setting.
2. Materials and methods
This study reports on the secondary outcome of FAB from the trial Implementation of physical exercise at the Workplace (IRMA09)—Laboratory technicians. Data were obtained during a larger scale worksite intervention trial previously described by our research team.[34] Briefly, we performed a single-blind randomized controlled trial with allocation concealment in a 2-armed parallel group design among female laboratory technicians at a single worksite with multiple departments in Denmark during the spring/summer of 2014. The participants were parallel-assigned to receive either physical-cognitive-mindfulness training or to follow ongoing company initiatives aimed at reducing musculoskeletal pain for 10 weeks at the worksite. Ethical approval was obtained from The Danish National Committee on Biomedical Research Ethics (The local ethical committee of Frederiksberg and Copenhagen; H-3-2010-062) as part of the research program “Implementation of physical exercise at the workplace (IRMA).” The trial Implementation of physical exercise at the Workplace (IRMA09)—Laboratory technicians was registered in the ClinicalTrials.gov register (NCT02047669) prior to participant enrollment. The criteria of the revised Consolidated Standards of Reporting Trials (CONSORT) 2010 statement for reporting randomized trials have been followed.[35] All experimental conditions conformed to The Declaration of Helsinki, and all participants signed an informed consent form prior to the commencement of the intervention.
2.1. Participant recruitment and group allocation
At the time of enrollment, the participants (n = 112) had to be suffering from chronic musculoskeletal pain in 1 or more of the following regions to participate in the study: (i) upper back, (ii) lower back (iii) neck, (iv) shoulders, (v) elbows, or (vi) hands/wrists. To fulfill the definition of chronic pain, all following criteria were met for at least one of these body regions: (i) pain intensity ≥3 (on a 0–10 Visual Analog Scale) during the last week, (ii) pain frequency of ≥3 days during the last week, and (iii) pain lasting at least 3 months. The participants meeting the typical exclusion criteria, for example, severe hypertension, were allowed to participate in the less strenuous part of the training intervention if their general practitioner provided consent. We excluded participants with life-threatening diseases, and pregnancy was considered a contraindication to the training.
By generating a random numbers table in SAS software, the participants were allocated to either the physical-cognitive-mindfulness training intervention (PCMT) or the reference group (REF). All the participants were informed about their particular group allocation by email after the baseline questionnaire data were acquired. The participants were informed that it was unknown which treatment model works best for reducing pain, and they were instructed not to reveal their particular group to colleagues or to the study assessors; hence, all assessors, including the statisticians, remained blinded. Due to the nature of the intervention, it was not possible to keep the participants blinded. Table 1 shows the baseline demographics after group allocation, and Fig. 1 shows the flow through the study.
Table 1.
Baseline demographics after allocation to physical-cognitive-mindfulness training (PCMT) (N = 56) or reference group (REF) (N = 56).
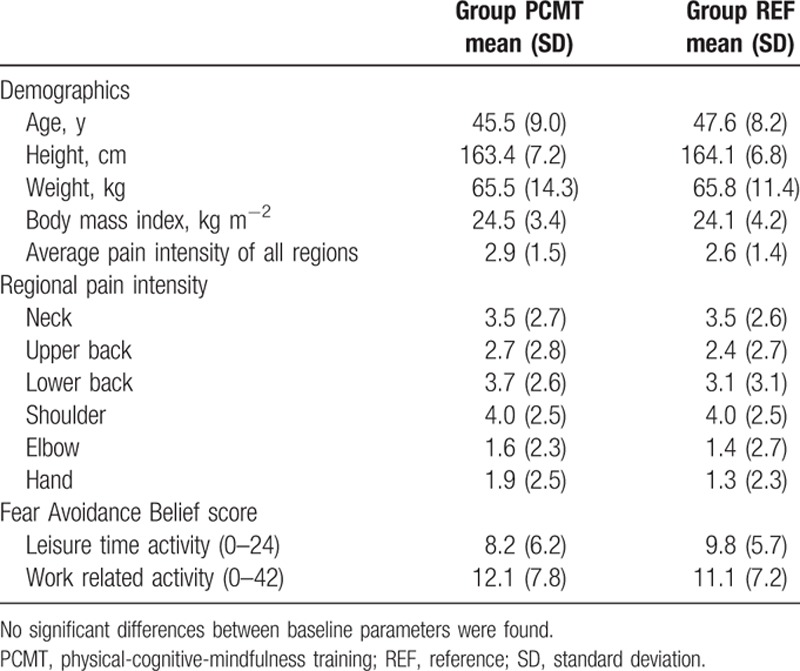
Figure 1.
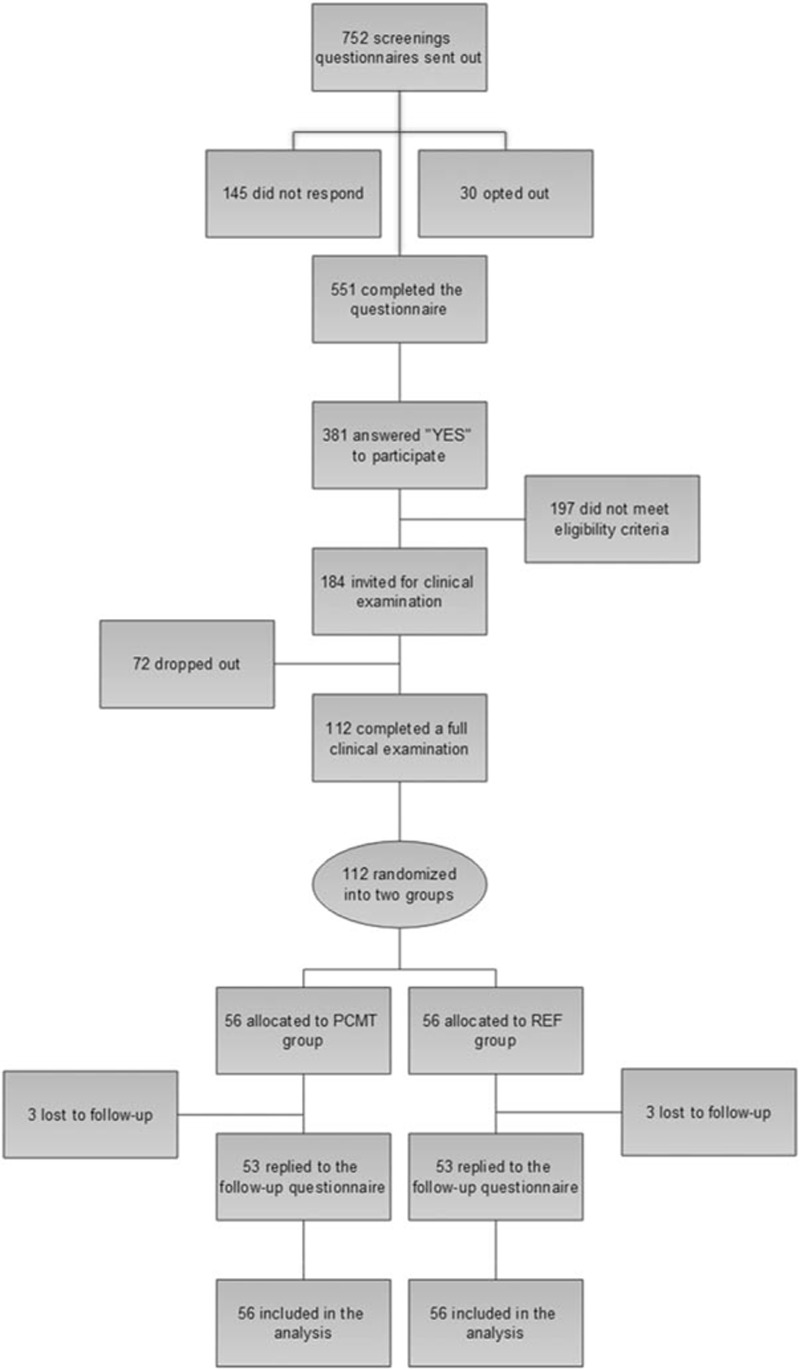
Flowchart showing participant flow through the study from initial screening to randomization and follow-up.
2.2. Interventions
The intervention design has previously been described,[34] and the primary outcome results on pain and stress have also been reported.[36] In short, we introduced a multifactorial intervention to the PCMT group consisting of (i) slow joint mobility exercises focusing on precise motor control primarily for the pain-affected area, (ii) 4 different strength training exercises with elastic bands, (iii) cognitive behavioral therapy in which education and counseling about the fear of movement, the positive effects of movement and de-catastrophizing pain were the main focus areas, and (iv) mindfulness group training lasting 10 weeks. The strength training, joint mobility/precise motor control training, and cognitive behavioral therapy and education were grouped together and administered in brief 20 minutes sessions 4 times per week by a professional trainer with a relevant background. The mindfulness sessions were kept separate from the physical training and were administered once weekly by a psychologist specialized in stress. To address possible confounding factors, we tracked (i.e., asked in the questionnaire at baseline and follow-up) (1) the number of days the participants had used pain medication in the last week and (2) the number of treatment sessions (e.g., with a medical doctor, physical therapist, or other type of health personnel) the participant had received for pain in the back, neck, shoulders, elbows or hands/wrists within the last month. The REF group served as a control group and followed ongoing company initiatives as described elsewhere.[34,36] Briefly, participants in both groups were recommended to continue their usual physical activities alongside the intervention, and the company's own health and safety professionals were available upon request from each department manager to provide ergonomic education; this education consisted of individualized recommendations on changing task-specific working positions and instructions on the proper use of ergonomic aids to adhere to each department structure. The management of each individual department was responsible for prioritizing and utilizing the ergonomic support options. Available in some departments, an “exercise ambassador” organized lunch-time exercise breaks 3 times weekly, each lasting 10 minutes with voluntary participation. As this was an initiative that was already implemented, we recommended all participants not to change their participation or nonparticipation in these activities during the intervention.
2.3. Evaluation of fear-avoidance
We evaluated the participants’ fear-avoidance behavior in work-related movements by the FAB Questionnaire (FABQ) at baseline before the group allocation and again post intervention at the follow-up 10 weeks later. The FABQ designed by Waddell et al[37] in 1993 was modified to assess the specific pain-affected regions of this particular population, thereby not limiting it to only low back pain. Briefly, the FABQ is a 2-part questionnaire. The first part consists of 5 questions/statements about pain and physical activity, and the second part consists of 11 questions/statements about how work affects the participants’ perception of pain. Each question is scored from 0 to 6, ranging from completely disagree (0) to completely agree (6). Four of the 5 questions about pain and physical activity compose the leisure time physical activity score, and 7 of the 11 work-related questions compose the avoidance belief score pertaining to work; thus, the scoring range is from 0 to 24 and 0 to 42, respectively, with higher scores corresponding to higher levels of FAB. An example of one of the work-related questions on the FABQ is My work makes or would make my pain worse.[37] A Danish version of the FABQ has not been tested for validity or reliability, but a Norwegian version has and was found to have acceptable factor structure, internal consistency, test-retest reliability, and construct validity by Grotle et al in 2006.[38]
2.4. Statistical analysis
All statistical analyses were performed using SAS software for Windows (SAS Institute, Cary, NC). Changes in FAB were evaluated using a repeated measures linear mixed model (Proc Mixed) with group, time, and group by time interaction as the independent variables. Subject nested within group was entered as a random effect. The analyses were adjusted for baseline values. We performed all statistical analyses in accordance with the intention-to-treat principle using the Proc Mixed procedure of SAS, which inherently accounts for missing values. Finally, we calculated the effect sizes as Cohen's d based on the average fear-avoidance belief score (between-group differences divided by the baseline pooled standard deviation).[39] An alpha level of <0.05 was accepted as statistically significant. The outcomes are reported as between-group least mean square differences (95% confidence interval) at the 10-week follow-up. The calculation of the sample size has previously been described.[34,36] Using simple correlation analyses (Pearson's r), we also tested the association between FABQ scores and pain in the different body regions, both at baseline (N = 551) and for changes in the variables for those included in the study who completed both the baseline and follow-up questionnaires (N = 105).
3. Results
As reported in the article covering the primary outcome results of this trial,[36] the adherence to the physical-cognitive training and mindfulness sessions was 70% and 47.5% of the intended sessions, respectively. Furthermore, there were no reported adverse events during the intervention. A total of 6 participants (3 from each group) were lost to follow-up. We have no information about 4 of the participants, whereas the remaining 2 dropouts changed jobs during the intervention.[36]
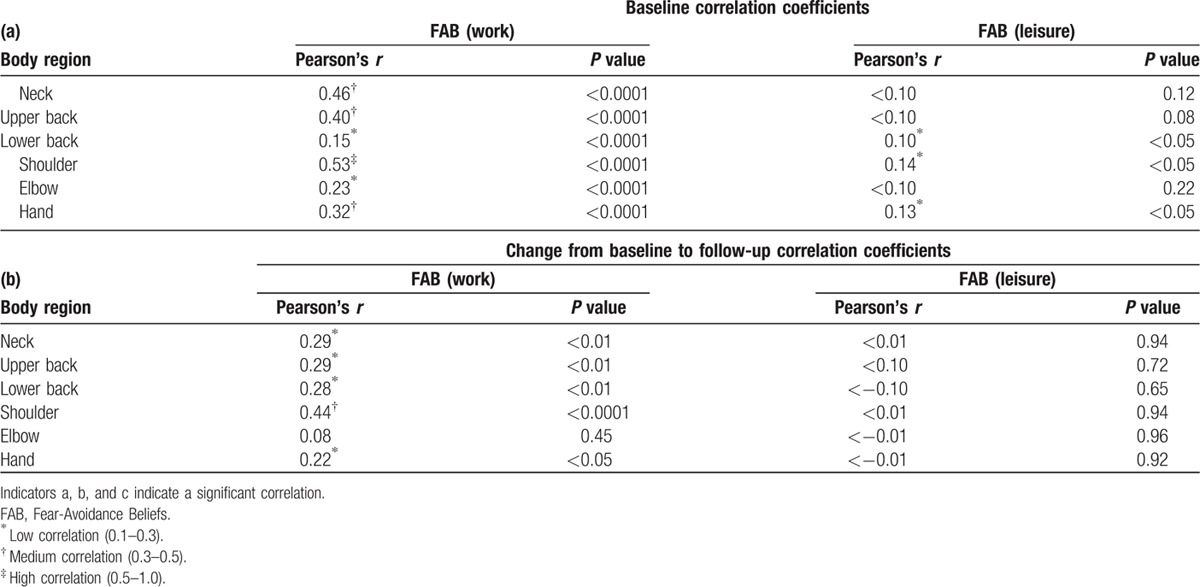
Baseline work-related FAB were significantly associated with pain in all the assessed body regions, most strongly for neck (r = 0.46) and shoulder (r = 0.53) pain. Regarding changes from baseline to follow-up, work-related FAB were significantly associated with pain in all body regions but the elbow and was most strongly related to changes in shoulder pain (r = 0.44). Leisure time FAB were only weakly associated with pain at baseline in the shoulders, lower back, and hands/wrists and was not significantly associated with changes in pain of any body region. Table 2 shows the associations of FAB with body regions.
Table 2.
Pearson's r correlation coefficients for work and leisure time Fear-Avoidance Beliefs (FAB) at baseline (N = 551) and changes from baseline to follow-up (N = 105) for each body region for those who completed the questionnaires.
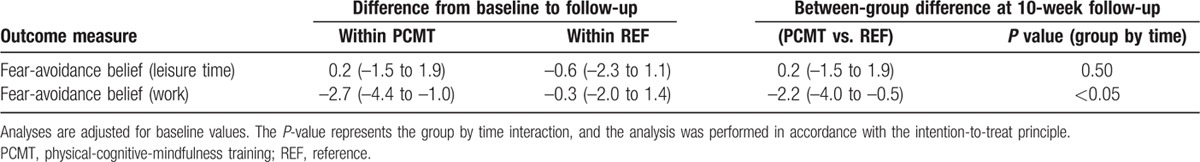
A significant group by time interaction was observed (P < 0.05) for work-related FAB. The between-group difference at the 10-week follow-up was –2.2 (–4.0 to –0.5) (scale 0–42). The within-group changes from baseline to 10-week follow-up were –2.7 (–4.4 to –1.0) and –0.3 (–2.0 to 1.4) for the PCMT and REF groups, respectively. The group by time interactions were nonsignificant for leisure time FAB between groups (P > 0.05). The effect size (Cohen's d) of the change in work-related FAB was 0.30 and thereby categorized as a small to medium (0.2–0.50) effect for the PCMT group.[19]Table 3 shows the group by time interactions for work-related and leisure time FAB.
Table 3.
Within-group differences from baseline to 10-week follow-up and between-group differences at 10-week follow-up of fear-avoidance beliefs during leisure time and work.
4. Discussion
Our results show that a 10-week targeted physical-cognitive-mindfulness intervention has significant effects on work-related FAB. As previously reported, the intervention group experienced reduced pain intensity by ∼52% across 6 body regions compared to the REF group[36], and the present analyses show that the change in work-related FAB was most strongly related to changes in shoulder pain. This suggests that a decrease in the experienced intensity of musculoskeletal pain, especially around the shoulders, may influence the cognitive-behavioral mechanisms in female laboratory technicians. The painful body region most highly correlated to work-related FAB was also the most painful body region (shoulders) at baseline (Table 1), which suggests that work-related FAB are body region specific to the degree of experienced pain. This observation is supported by the current neuromatrix of pain theory.[14,16,17,26,40–42] As described in the protocol of the study,[34] the training intervention involved targeted and individually adapted motor control mobility exercises designed in such a way that known painful movements were directly addressed and practiced. Combined with the pain education and noncatastrophizing strategies, this approach may have had a direct pain-relieving effect due to the acute closing of the pain gate in conjunction with an indirect psychological effect on the participant when suddenly experiencing a movement once perceived as painful as less threatening to the organism.[14,15,26,40,41,43]
The more nuanced treatment approach compared to the conventional treatment interventions may be why the participants experienced a decrease in work-related FAB following the intervention in the present study. The design of the intervention separates itself from more traditional treatment models of musculoskeletal pain, such as general physical exercise programs. For the fearful chronic pain patient, not receiving education about the mechanisms of pain processing and pain catastrophizing may cause heightened escape and avoidance behavior and may reinforce the pain neuromatrix. For example, Al-Obaidi et al suggested that FAB counteracted the beneficial effects of an exercise-based therapy program,[44] and Jellema et al indicated that pain catastrophizing hampered the efficacy of usual practitioner care in chronic low back pain patients.[45] The main question that remains to be answered pertains to the delivery method of the general exercise treatment model and whether pain-related fear and the associated safety/escape behaviors are adequately addressed. This is 1 factor that separates the present study and its treatment model from conventional therapies. The effects of brief educational sessions in treatment programs for chronic low back pain patients are highlighted by Burton et al, Moore et al, and Symonds et al.[46–48] For example, a straightforward educational campaign consisting of advising individuals to stay active and discouraging the use of medical interventions resulted in long-lasting reductions in FAB in the community as well as in physicians and in less workers compensation claims for low back pain.[49] Addressing the fear-pain loop with education about the pain neuromatrix in a work-related context that is specific to each individual may at least partly explain our observations of the significantly reduced work-related FAB.
The intervention also included supervised mindfulness sessions on a weekly basis. Because the perception of the body-self neuromatrix of pain is influenced by perceived distress, it is relevant to consider the effects of mindfulness as a possible mechanism to decrease pain-related fear of movement. However, as the level of self-reported stress did not significantly decrease in the PCMT group compared to the REF group[36], it is less likely that the level of experienced distress would have a direct effect on FAB.[34] Furthermore, as reported by Jay et al. in 2015, an exploratory analysis of the dose–response relationship between physical training and mindfulness sessions and musculoskeletal pain perception showed that, on average, there was a 0.6-point decrease in pain per average weekly training session attended, whereas there was a 0.15-point increase in pain per mindfulness session attended.[36] This indicates that not only did the mindfulness sessions not reduce the perception of distress, but they also seem to have countered the positive effect of the physical training sessions. This is in contrast to what has previously been found regarding the effects of meditation and mindfulness on the mechanisms of pain perception. For example, Zeidan and colleagues found that meditation alters brain activation patterns by reframing the contextual processing of painful sensory inputs and ultimately leads to a decrease in the nociceptive interpretation of afferent signals in the pain neuromatrix.[50] In another study, Zeidan et al also report that a brief 3-day mindfulness meditation intervention was effective in reducing pain ratings and anxiety scores when compared with baseline testing of experimentally induced pain.[51] Other research groups have also concluded that mindfulness meditation has a role in pain management and psychological health.[50,51–55] A recent study by van Berkel et al showed no effect of a long-term comprehensive multicomponent worksite mindfulness intervention on various lifestyle behaviors. The researchers concluded that the effectiveness of such an intervention could not be established.[56] Based on the results of the present study, as well as the lack of efficacy of the mindfulness sessions implemented at the work site, it is therefore unlikely that the mindfulness component of the intervention had a significant effect on the observed reduction in fear-avoidance behavior in the PCMT group.
Our study has several strengths and limitations. An important strength of the present study included the single-blinded randomized controlled design. Furthermore, the instructors ensured that only participants who were randomized to training and mindfulness participated in these sessions, thereby eliminating between-group contamination. The limitations of behavioral interventions include the inability to blind participants to which intervention they receive. Self-reported outcomes are a limitation, as they may be influenced by placebo effects and outcome expectations. Nevertheless, PRF of movement is a subjective experience, and the reference group was not a pure control group, as they were encouraged to participate in the ongoing activities at the company.[34] Furthermore, the intervention comprised several different components, which makes it difficult to determine which part(s) of the intervention had the primary effect on the observed reduction in work-related FAB. However, it is most likely that the part of the intervention that had the primary effect on pain reduction also had the primary effect on work-related FAB reduction, as the previously mentioned dose–response analysis showed increases in pain with each mindfulness session attended and decreases in pain with each physical-cognitive session attended.[36] The lack of ability to distinguish between the effect of precise joint mobility training and that of strength training on FAB is a limitation of the present study that makes it difficult to draw conclusions about which part of the physical intervention had the greatest impact on work-related FAB. Questionnaires that assess PRF of movement and kinesiophobia are used as screening tools for clinicians to identify cases with excessive PRF. According to Vlaeyen and Linton,[29] this seems to be a relevant approach. Unfortunately, norm data are lacking, and therefore there are no cut-off points to identify clinically relevant reductions in FAB and kinesiophobia; this makes it impossible to determine whether the observed reduction in the present study has significant clinical relevance.[29] This is an important limitation but applies to all questionnaire-based methods of evaluating FAB. A valid alternative could have been to use observational or psychophysiological methods of evaluation, but the application of such methods in the field of chronic pain is scarce, and knowledge is therefore lacking.[29] Finally, most studies on FAB involve chronic low back pain patients, which differs from the present study, although at least 2 studies have used it to evaluate upper extremity pain.[57,58] One may argue that low back pain imposes a great threat to the organism when compared to pain in upper extremities and that the outcomes of fear-avoidance treatment models thus differ.
In conclusion, our study shows that work-related FAB, as assessed by the FABQ, can be significantly reduced by 10 weeks of physical-cognitive-mindfulness training in female laboratory technicians. However, leisure time FAB was unaffected by the PCMT intervention when compared with the REF group, indicating that FAB is context specific. We propose that the observed effect on work-related FAB was primarily derived from the physical-cognitive portion of the intervention and, to a lesser extent, the mindfulness portion. Further investigations should examine if an improved perception of PRF of work-related activity causes subconscious alterations in work-specific movement patterns, thus improving work environment ergonomics and contributing to the extent that reductions in FAB can be considered clinically relevant.
Supplementary Material
Footnotes
Abbreviations: FAB = Fear-avoidance beliefs, FABQ = Fear-avoidance beliefs questionnaire, PCMT = hysical-cognitive-mindfulness training, PRF = Pain-related fear, REF = Reference.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is Available for this Article.
References
- 1.Leischik R, Dworrak B, Strauss M, et al. Plasticity of health. GJOM 2016; 1:1–17. [Google Scholar]
- 2.Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ 1997; 314:591–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soler-Vila H, García-Esquinas E, León-Muñoz LM, et al. Contribution of health behaviours and clinical factors to socioeconomic differences in frailty among older adults. J Epidemiol Community Health 2015; jech – 2015–206406. [DOI] [PubMed] [Google Scholar]
- 4.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol Off J Int Soc Electrophysiol Kinesiol 2004; 14:13–23. [DOI] [PubMed] [Google Scholar]
- 5.Santosa A, Schröders J, Vaezghasemi M. Inequality in disability-free life expectancies among older men and women in six countries with developing economies. J Epidemiol Community Health 2016; jech-2015-206640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008; 358:2468–2481. [DOI] [PubMed] [Google Scholar]
- 7.Bircher J, Kuruvilla S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy 2014; 35:363–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leischik R, Foshag P, Strauß M, et al. Aerobic capacity, physical activity and metabolic risk factors in firefighters compared with police officers and sedentary clerks. PloS One 2015; 10:e0133113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leischik R, Foshag P, Strauß M, et al. Correction: Aerobic capacity, physical activity and metabolic risk factors in firefighters compared with police officers and sedentary clerks. PloS One 2015; 10:e0136224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez Chaparro MA, Calvo Bonacho E, Gonzalez Quintela A, et al. High cardiovascular risk in Spanish workers. Nutr Metab Cardiovasc Dis 2011; 21:231–236. [DOI] [PubMed] [Google Scholar]
- 11.NFA: Arbejdsmiljø i Danmark: Arbejdsmiljø og Helbred i Danmark 2012-20 [Internet]. [cited 2016 May 18]. Available from: http://www.arbejdsmiljoforskning.dk/da/arbejdsmiljoedata/arbejdsmiljoe-og-helbred-20.
- 12.Jay K, Friborg MK, Sjøgaard G, Jakobsen MD, et al. The consequence of combined pain and stress on work ability in female laboratory technicians: a cross-sectional study. Int J Environ Res Public Health 2015; 12:15834–15842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reneman MF, Schiphorts Preuper HR, Kleen M, et al. Are pain intensity and pain related fear related to functional capacity evaluation performances of patients with chronic low back pain? J Occup Rehabil 2007; 17:247–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derbyshire SW. Exploring the pain “neuromatrix”. Curr Rev Pain 2000; 4:467–477. [DOI] [PubMed] [Google Scholar]
- 15.Melzack R. Pain and the neuromatrix in the brain. J Dent Educ 2001; 65 12:1378–1382. [PubMed] [Google Scholar]
- 16.Loeser JD, Melzack R. Pain—an overview. Lancet 1999; 353:1607–1609. [DOI] [PubMed] [Google Scholar]
- 17.Visser EJ, Davies S. Expanding Melzack's Pain Neuromatrix. the Threat Matrix: A Super-System for Managing Polymodal Threats. Pain Pract 2010; 10:163–1163. [DOI] [PubMed] [Google Scholar]
- 18.Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 1986; 3:S1–S226. [PubMed] [Google Scholar]
- 19.Meulders A, Vansteenwegen D, Vlaeyen JWS. The acquisition of fear of movement-related pain and associative learning: a novel pain-relevant human fear conditioning paradigm. Pain Int Assoc Study Pain 2011; 152:2460–2469. [DOI] [PubMed] [Google Scholar]
- 20.Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. International Association for the Study of Pain 2012; 153:1144–1147. [DOI] [PubMed] [Google Scholar]
- 21.Moseley G. A new direction for the fear avoidance model? Pain 2011; 152:2447–2448. [DOI] [PubMed] [Google Scholar]
- 22.Barke A, Baudewig J, Schmidt-samoa C, et al. Neural correlates of fear of movement in high and low fear-avoidant chronic low back pain patients: an event-related fMRI study. Pain 2012; 153:540–552. [DOI] [PubMed] [Google Scholar]
- 23.Meeus M, Nijs J. Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin Rheumatol 2007; 26:465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lethem J, Slade PD, Troup JDG, et al. Outline of a fear-avoidance model of exaggerated pain perception—I. Behav Res Ther 1983; 21:401–408. [DOI] [PubMed] [Google Scholar]
- 25.Pollatos O, Füstös J, Critchley HD. On the generalised embodiment of pain: how interoceptive sensitivity modulates cutaneous pain perception. Pain International Association for the Study of Pain 2012; 153 8:1680–1686. [DOI] [PubMed] [Google Scholar]
- 26.Khalsa PS. Biomechanics of musculoskeletal pain: dynamics of the neuromatrix. J Electromyogr Kinesiol Off J Int Soc Electrophysiol Kinesiol 2004; 14:109–120. [DOI] [PubMed] [Google Scholar]
- 27.Moulton e A, Schmahmann JD, Becerra L, et al. The cerebellum and pain: passive integrator or active participator? Brain Res Rev Elsevier BV 2010; 65:14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain International Association for the Study of Pain 2000; 85:317–332. [DOI] [PubMed] [Google Scholar]
- 29.Vlaeyen JW, Kole-Snijders AM, Rotteveel AM, et al. The role of fear of movement/(re)injury in pain disability. J Occup Rehabil 1995; 5:235–252. [DOI] [PubMed] [Google Scholar]
- 30.George SZ, Fritz JM, Bialosky JE, et al. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine (Philadelphia) 2003; 28:2551–2560. [DOI] [PubMed] [Google Scholar]
- 31.Kromer TO, Sieben JM, de Bie RA, et al. Influence of fear-avoidance beliefs on disability in patients with subacromial shoulder pain in primary care: a secondary analysis. Phys Ther 2014; 94:1775–1784. [DOI] [PubMed] [Google Scholar]
- 32.Hasenbring MI, Verbunt JA. Fear-avoidance and endurance-related responses to pain: new models of behavior and their consequences for clinical practice. Clin J Pain 2010; 26:747–753. [DOI] [PubMed] [Google Scholar]
- 33.Wertli MM, Rasmussen-Barr E, Weiser S, et al. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. Spine J 2014; 14:816–836.e4. [DOI] [PubMed] [Google Scholar]
- 34.Jay K, Brandt M, Sundstrup E, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain, stress and work ability among laboratory technicians: randomized controlled trial protocol. BMC Musculoskelet Disord 2014; 15:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010; 63:e1–e37. [DOI] [PubMed] [Google Scholar]
- 36.Jay K, Brandt M, Hansen K, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain and stress among laboratory technicians: randomized controlled trial. Pain Physician 2015; 18:459–471. [PubMed] [Google Scholar]
- 37.Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993; 52:157–168. [DOI] [PubMed] [Google Scholar]
- 38.Grotle M, Brox JI, Vøllestad NK. Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: methodological aspects of the Norwegian version. J Rehabil Med 2006; 38:346–353. [DOI] [PubMed] [Google Scholar]
- 39.Cohen J. CHAPTER 2 - The t Test for Means. In: Statistical Power Analysis for the Behavioral Sciences (Revised Edition) [Internet]. Academic Press; 1977. [cited 2016 Jun 15]. p. 19–74. Available from: http://www.sciencedirect.com/science/article/pii/B9780121790608500074. [Google Scholar]
- 40.Moseley G. A pain neuromatrix approach to patients with chronic pain. Man Ther 2003; 8:130–140. [DOI] [PubMed] [Google Scholar]
- 41.Melzack R. Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: presented at the third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract 2005; 5:85–94. [DOI] [PubMed] [Google Scholar]
- 42.Iannetti GD, Mouraux A. From the neuromatrix to the pain matrix (and back). Exp Brain Res 2010; 205:1–12. [DOI] [PubMed] [Google Scholar]
- 43.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007; 133:581–624. [DOI] [PubMed] [Google Scholar]
- 44.Al-Obaidi SM, Beattie P, Al-Zoabi B, et al. The relationship of anticipated pain and fear avoidance beliefs to outcome in patients with chronic low back pain who are not receiving workers’ compensation. Spine (Philadelphia) 2005; 30:1051–1057. [DOI] [PubMed] [Google Scholar]
- 45.Jellema P, van der Horst HE, Vlaeyen JWS, et al. Predictors of outcome in patients with (sub)acute low back pain differ across treatment groups. Spine (Philadelphia) 2006; 31:1699–1705. [DOI] [PubMed] [Google Scholar]
- 46.Burton AK, Waddell G, Tillotson KM, et al. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine (Philadelphia) 1999; 24:2484–2491. [DOI] [PubMed] [Google Scholar]
- 47.Moore JE, Von Korff M, Cherkin D, et al. A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain 2000; 88:145–153. [DOI] [PubMed] [Google Scholar]
- 48.Symonds TL, Burton AK, Tillotson KM, et al. Absence resulting from low back trouble can be reduced by psychosocial intervention at the work place. Spine (Philadelphia) 1995; 20:2738–2745. [DOI] [PubMed] [Google Scholar]
- 49.Buchbinder R, Jolley D. Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine (Philadelphia) 2005; 30:1323–1330. [DOI] [PubMed] [Google Scholar]
- 50.Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci 2011; 31:5540–5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zeidan F, Gordon NS, Merchant J, et al. The effects of brief mindfulness meditation training on experimentally induced pain. J Pain 2010; 11:199–209. [DOI] [PubMed] [Google Scholar]
- 52.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985; 8:163–190. [DOI] [PubMed] [Google Scholar]
- 53.Cramer H, Haller H, Lauche R, et al. Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complement Altern Med 2012; 12:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fjorback LO, Walach H. Meditation based therapies—a systematic review and some critical observations. Religions 2012; 3:1–18. [Google Scholar]
- 55.Marchand WR. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. J Psychiatr Pract 2012; 18:233–252. [DOI] [PubMed] [Google Scholar]
- 56.Van Berkel J, Boot CRL, Proper KI, et al. Effectiveness of a worksite mindfulness-based multi-component intervention on lifestyle behaviors. Int J Behav Nutr Phys Act 2014; 11:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mintken PE, Cleland JA, Whitman JM, et al. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with shoulder pain. Arch Phys Med Rehabil 2010; 91:1128–1136. [DOI] [PubMed] [Google Scholar]
- 58.Inrig T, Amey B, Borthwick C, et al. Validity and reliability of the Fear-Avoidance Beliefs Questionnaire (FABQ) in workers with upper extremity injuries. J Occup Rehabil 2012; 22:59–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


