Abstract
Objective
Determine if a 1-hour pad test at discharge can identify continence status within 120 days of obstetric vesicovaginal fistula (VVF) repair.
Design
Prospective cohort study.
Setting
Fistula Care Centre in Lilongwe, Malawi.
Population
Women with VVF who underwent repair between January 2012–December 2014.
Methods
Data on demographics, obstetric history, physical exam findings, operative management, post-operative findings, and follow-up evaluations were collected on women with VVF repair.
Main outcome measures
Sensitivity, specificity, positive and negative predictive values (PPV and NPV), and a receiver operating curve (ROC) were calculated to assess the utility of using a discharge pad test at three thresholds to identify women likely to be continent at follow-up.
Results
After VVF repair, 346 women had a 1-hour pad test performed at the time of hospital discharge and completed follow-up within 120 days of repair. Of these, 79.8% (n=276) were completely continent, while 20.2% (n=70) had some degree of incontinence. The sensitivity and specificity of a negative 1-hour pad test at predicting continence is 68.1% and 82.9%, respectively. With this prevalence, a negative pad test at a 1.5-gram threshold demonstrates a high predictive value (PPV=94.0%, 95% CI 90.0, 96.9) in detecting women with continence after repair.
Conclusions
At the 1.5-gram threshold, a negative pad test at discharge identifies 94% of women who will remain continent after VVF repair. Adding the pad test to fistula care can identify women who are likely to remain continent and may not need further therapies in settings where resources are limited and follow-up after repair is difficult.
Tweetable abstract
A negative pad test after repair is associated with continued continence at follow-up.
Keywords: obstetric fistula, pad test, residual incontinence, Africa, Malawi
Introduction
Obstetric fistula (OF) affects an estimated 2 million women worldwide,1 primarily in sub-Saharan Africa and south Asia. It is a serious complication of childbirth that is associated with prolonged, obstructed labor. In these situations, pressure from the fetal head against vaginal wall tissue leads to necrosis, causing an abnormal communication between the vagina and the bladder (vesicovaginal fistula; VVF) and/or between the vagina and the rectum (rectovaginal fistula; RVF). This results in constant leaking of urine or feces from the vagina. In Malawi, the prevalence of OF is estimated to be 1.6 per 1000 women,2 with VVF representing the majority of the fistula cases identified by hospital records.
Although surgical interventions have been shown to be effective for VVF, not all women undergoing these procedures regain continence. Rates of fistula closure reported in the literature vary widely between 41–100%,3, 4 with an average of 85%.5 However, even women with a successful OF closure may continue to be incontinent due to residual stress urinary incontinence, small bladder size, neurologic damage, or damage to the sphincter or urethra.6 After obstetric fistula repair, it is difficult to predict which women will have residual incontinence and need close follow-up and additional therapy. In many areas where fistula repair is performed, limited clinical personnel, funding, and infrastructure are available to follow women after repair. A diagnostic tool to identify women who should be prioritized for follow-up after repair would be helpful to optimally utilize scant resources.
The International Continence Society states that pad weight testing can be used as an optional non-invasive test of continence.7 One-hour pad tests have been used both pre-operatively as a measure of severity of incontinence and post-operatively8 as a measure of surgical success of procedures aimed at improving incontinence. Women who are still suffering from urinary incontinence 3 months after repair are unlikely to have significant improvement in their leaking and can benefit from additional surgical and non-surgical therapies. Our objective was to assess the utility of using a discharge pad test at three thresholds to identify continence status at follow-up.
Methods
Study Setting
This study took place at the Freedom from Fistula Foundation Fistula Care Centre at Bwaila Hospital in Lilongwe, Malawi. The Fistula Centre receives referrals from all regions of Malawi as well as western Mozambique and eastern Zambia. Referred patients undergo a comprehensive history and physical examination prior to fistula repair surgery. A majority of surgeries were performed or overseen by the same surgeon during this study period. Patients are kept as inpatients until urethral catheter removal (on average, post-operative day 14). After the urethral catheter is removed, a dye test is performed. If the dye test is positive, the patient is assumed to have a residual fistula and advised to return for follow-up for counseling on subsequent surgical and non-surgical management options. If the dye test is negative, the patient undergoes a cough stress test and a 1-hour pad weight test. To conduct the 1-hour pad test, an extra-long maxi pad is pre-weighed. The patient then wears the pad doing various activities for one hour and then the pad removed and is weighed again. The 1-hour pad weight is calculated as the difference between the two pad weights. All patients are advised to return to the Fistula Care Centre for clinical follow-up 30 days after discharge. As the exact timing of discharge after surgery and return for the first follow-up varies from woman to woman, we set a minimum threshold for completing the first follow-up at 21 days after surgery and a maximum threshold at 120 days after surgery and only considered the continence status from the first clinical follow-up completed in this time period (if more than one were completed)
Study Population
We analyzed data from a prospective cohort study of women who had VVF fistula repair at the Fistula Care Centre between January 2012 and December 2014. Women were included in this analysis if they had a confirmed OF, were undergoing an initial VVF repair at the Fistula Care Centre (prior repairs at other centres were not excluded), and completed a post-operative 1-hour pad test prior to discharge. Women were excluded from the analysis of predictors of a positive pad test if they died prior to discharge, had a residual fistula (determined with a positive dye test), or had only a ureteral re-anastamosis or urinary diversion as their initial surgery. Women who did not have clinical follow-up at the Fistula Care Centre within 120 days of repair with a documented continence grade were excluded from the analysis on the ability of pad weight to predict continence status.
Data Collection
Staff trained in data collection recruited, consented, and enrolled eligible participants in either English or the local language (Chichewa). Eligible women provided informed consent for collection of demographic data, physical exam findings, surgical procedures, post-operative findings, and follow-up visits. Ethical approval was obtained from the National Health Sciences Research Committee of Malawi and the University of North Carolina School of Medicine Institutional Review Board. Women over 18 gave informed consent, while those under 18 underwent parental consent and pediatric assent. Trained research assistants double-entered and compared the data using REDCap (Research Electronic Data Capture, NC).9
Variables
The primary outcome is the ability of a 1-hour pad test to predict continence status within 120 days of VVF repair. Only women with closed fistulas were included in this analysis. We considered 3 different pad test thresholds in evaluating this outcome. The upper limit of continence for 1-hour pad testing is recommended by the International Continence Society as 1.4 grams.10 In our initial analysis, we considered pad weights ≥1.5 grams as positive and <1.5 grams as negative. As this test has not been previously validated in women with VVF repair, we also examined the performance of the 1-hour pad weight using thresholds of 1.0 grams and 2.0 grams. Women were considered to be continent at their follow-up visit if they had Grade 1 continence (“no incontinence”) and to have residual incontinence if they had Grade 2–5 continence (grade 2: incontinent with cough, strain, or exertion; grade 3: incontinent on walking; grade 4: incontinent on walking, sitting, and/or lying but still voiding some urine; grade 5: incontinent on walking, sitting, and/or lying but not voiding any urine) utilizing a common grading system for residual incontinence11 as determined by a trained clinician. We considered participant self-reported demographic information and HIV status as predictors of residual incontinence. HIV status was determined through testing of all participants prior to their VVF repair. Bladder capacity was estimated using a measurement of bladder depth (in cm) intra-operatively. Patients were examined under anesthesia to confirm the stage of their vesicovaginal fistula via the revised Goh classification system, which classifies fisulae by the distance of the distal edge of the fistula from the external urinary meatus, the size of the fistula, and the extent of the associated scarring.12
Statistical Analysis
Baseline characteristics were compared at baseline for all women with closed fistulas and a pad test at discharge. For women who returned for follow-up within 120 days of repair, we evaluated whether the pad test predicted continence. For all three thresholds, differences in the baseline and surgical characteristics between women with positive and negative pad tests at discharge were calculated using Pearson’s χ2 tests. Sensitivity, specificity, positive and negative predictive values with 95% confidence intervals (CIs) were calculated at thresholds of 1.0 grams, 1.5 grams, and 2.0 grams to assess the utility of using discharge pad weight to predict continence at follow-up. A priori goals of 60% sensitivity and 80% specificity to predict continence were determined. Specificity was prioritized to capture a high proportion of women with residual incontinence. A receiver operator characteristic (ROC) curve was used to estimate area under the curve (AUC) and the 95% CI. We did a sensitivity analysis with two scenarios: one assuming that among all women lost to follow-up those with a positive pad test had residual incontinence and those with a negative pad test were continent, and a second assuming among women lost to follow-up, all women with a positive pad test were continent and those with a negative pad test had residual incontinence. Statistical analysis was performed using STATA version 13.0 (StataCorp 2013, College Station, TX).
Results
Study Population
In the study period, 572 women had a baseline surgery at the Fistula Care Centre. Of these, 488 women underwent a VVF repair and were discharged (2 women died prior to discharge; Figure 1). Four hundred and forty-three of these women had a closed fistula, giving a fistula closure rate of 90.8%. Of these 443 women without residual fistula, 431 (97.2%) completed a 1-hour pad test. The weights from the pad test ranged from 0 to 107.5 grams with a median of 1.1 grams (Figure S1). Of these 431 women, 194 (45.0%) had a positive pad test (≥1.5 grams) and 237 (55.0%) had a negative pad test (<1.5 grams) at discharge. Women with a positive pad test were older, had fistulas closer to the external urinary meatus (by Goh type classification), had larger fistulas, had more vaginal scarring, were catheterized longer, and were more likely to have a positive post-operative cough stress test or low bladder capacity (Table 1). The proportion of women with a closed fistula who were continent at discharge was 68.7%.
Figure 1.
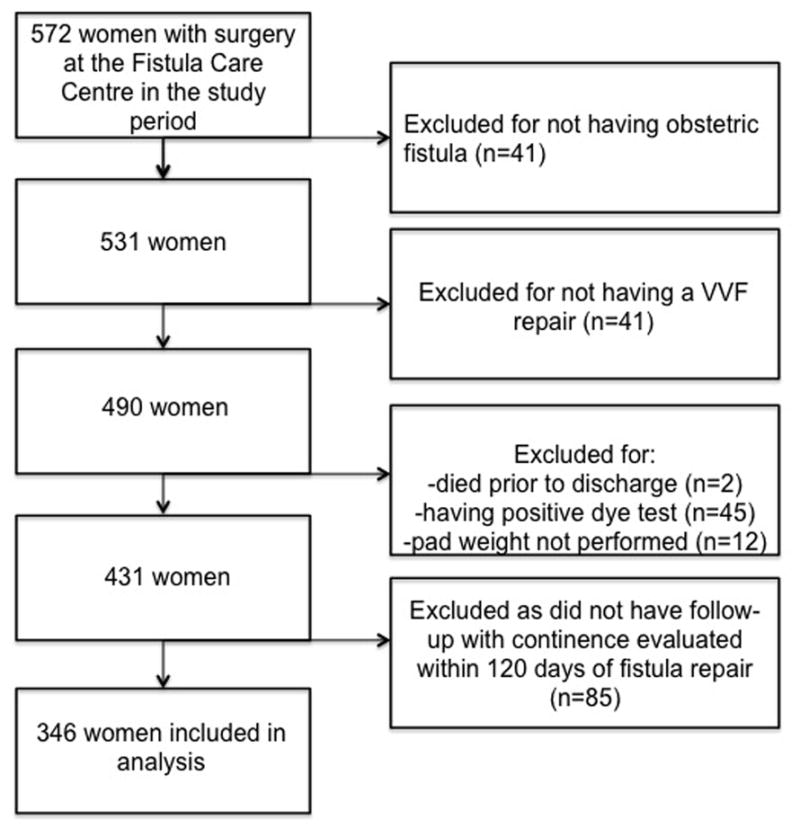
Flow diagram of women included in this analysis
Table 1.
Characteristics of women with negative and positive 1-hour pad tests after VVF repair (n=431) Pearson’s χ2 test utilized; EUM: External urethral meatus
| Characteristic | Positive Pad Weight (n=194) | Negative Pad Weight (n=237) | p value |
|---|---|---|---|
| Age category | 0.039 | ||
| 18–24 | 33 (17.0) | 47 (19.8) | |
| 25–44 | 100 (51.6) | 144 (60.8) | |
| ≥45 | 61 (31.4) | 46 (19.4) | |
| HIV Status | 0.738 | ||
| HIV-infected | 14 (7.2) | 15 (6.3) | |
| Missing | 3 (1.6) | 2 (0.8) | |
| History of prior fistula surgery at outside facility | 0.265 | ||
| Yes | 48 (24.7) | 48 (20.3) | |
| Revised Goh Classification | <0.001 | ||
| Type 1 (distal edge of fistula >3.5 cm from EUM) | 42 (21.7) | 117 (49.4) | |
| Type 2 (distal edge of fistula 2.5–3.5 cm from EUM) | 33 (17.0) | 55 (23.2) | |
| Type 3 (distal edge of fistula 1.5–2.5 cm from EUM) | 74 (38.1) | 52 (21.9) | |
| Type 4 (distal edge of fistula <1.5 cm from EUM) | 41 (21.1) | 8 (3.4) | |
| Missing | 4 (2.1) | 5 (2.1) | |
| Goh VVF Size | 0.002 | ||
| <1.5 cm | 54 (27.8) | 102 (43.0) | |
| 1.5–3.0 cm | 70 (36.1) | 82 (34.6) | |
| >3.0 cm | 66 (34.0) | 47 (19.8) | |
| Missing | 4 (2.1) | 6 (2.5) | |
| Vaginal Scarring | 0.002 | ||
| None/Minimal | 70 (36.1) | 119 (50.2) | |
| Moderate/Severe/Obliterated | 123 (63.4) | 112 (47.3) | |
| Missing | 1 (0.5) | 6 (2.5) | |
| Days of urethral catheterization post-operatively | 0.039 | ||
| 0–14 | 95 (49.0) | 139 (58.7) | |
| 15–21 | 87 (44.9) | 78 (32.9) | |
| ≥22 | 9 (4.6) | 10 (4.2) | |
| Missing | 3 (1.6) | 10 (4.2) | |
| Post-op Cough Stress Test | <0.001 | ||
| Positive | 112 (57.7) | 41 (17.3) | |
| Missing | 10 (5.2) | 11 (4.6) | |
| Other Incontinence | |||
| Urge | 2 (1.0) | 0 (0.0) | 0.117 |
| Low bladder capacity | 18 (9.3) | 2 (0.8) | <0.001 |
The median time from surgery to first follow-up was 53 days [interquartile range 47, 61]. When compared to those with a closed fistula at discharge, women with residual fistulas were much less likely to complete their first follow-up visit within 120 days of surgery (44.4% versus 86.2%, p<0.001). Women with positive pad tests (≥1.5 grams) were also less likely to complete their first follow-up visit (80.3% with positive pad test versus 88.0% of those with negative pad test, p=0.024).
Of the 346 women with closed fistulas who completed follow-up within 120 days of repair, 276 (79.8%) were continent and 70 (20.2%) had residual incontinence. Results from the 1-hour pad test at discharge show good ability to predict continence at follow-up (AUC=0.83, 95% CI 0.77, 0.89; Figure 2). The sensitivity of the 1-hour pad test at 1.5 grams was 68.1% (95% CI 62.2, 73.6) and the specificity was 82.9% (95% CI 72.0, 90.8). In this population with a prevalence of continence of 79.8%, the positive predictive value of a negative 1-hour pad test at predicting continence at follow-up was over 90% for all thresholds and was 94.0% (95% CI 90.0, 96.9) at the 1.5-gram threshold (Figure S2). When comparing the threshold of 1.5 grams for the pad test to thresholds of 1.0 gram and 2.0 grams, the threshold of 1.5 grams was the lowest threshold that met the a priori goals of a sensitivity of 60% and a specificity of 80% (Table 2) and there was little difference between the sensitivity and specificity between the 1.5 and 2.0 gram thresholds.
Figure 2.
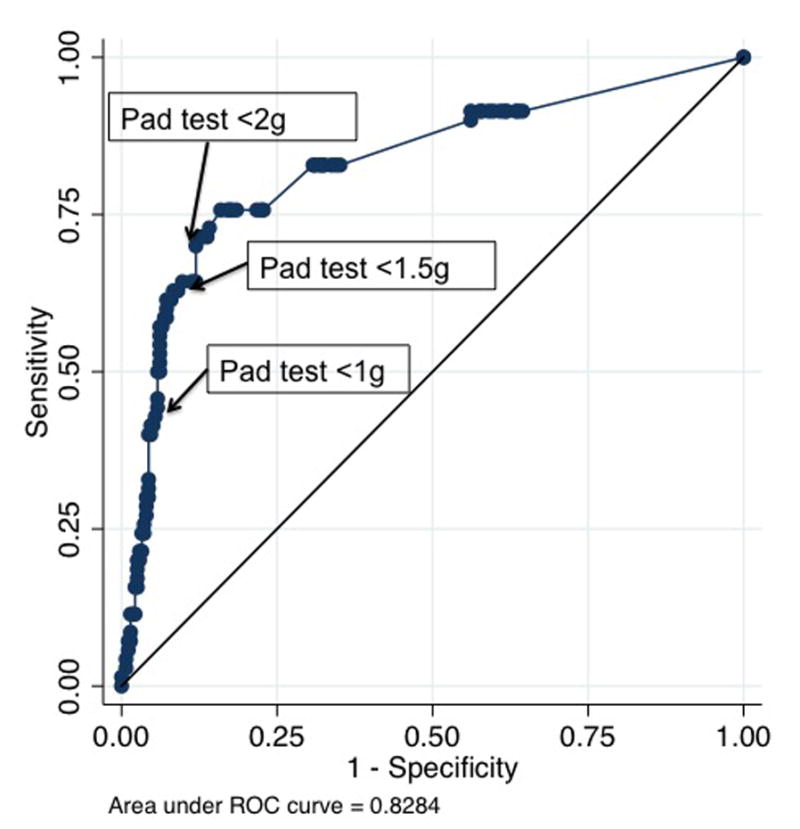
ROC curve for the use of post-operative 1-hour pad test to predict continence at follow-up
Table 2.
Sensitivity and Specificity of a negative 1-hour pad test at predicting continence (no residual incontinence) with various thresholds (n=346)
| ≥1.0 grams | 95% CI | ≥1.5 grams | 95% CI | ≥2.0 grams | 95% CI | |
|---|---|---|---|---|---|---|
| Sensitivity | 43.8% | 37.9, 49.9 | 68.1% | 62.2, 73.6 | 69.2% | 63.4, 74.6 |
| Specificity | 90.0% | 80.5, 95.9 | 82.9 % | 72.0, 90.8 | 82.9% | 72.0, 90.8 |
| Positive Predictive Value | 94.5% | 90.1, 97.8 | 94.0% | 90.0, 96.9 | 94.1% | 89.9, 96.9 |
| Negative Predictive Value | 28.9% | 23.0, 35.4 | 39.7% | 31.7, 48.1 | 40.6% | 32.4, 49.1 |
Most women returned with the same continence grades (n=252, 75.7%) or improved continence grades (n=49, 14.7%) (Table S1). Thirty-two women returned with worse continence grades; 17 (54.8%) of these were initially discharged as completely cured with continence grade 1. Most of the women who returned continent had a negative pad test prior to discharge (68.1%), whereas only 17.1% of those with residual incontinence had a negative pad test. However, of those women with a positive discharge pad test (≥1.5 grams), 60.3% were continent at the time of their follow-up.
For the sensitivity analysis, in the worst scenario—ie, all those with a negative pad test were incontinent and all those positive pad test were incontinent among those lost to follow-up, the proportion of women who were continent decreased from 79.8% to 75.2%. In this situation, the sensitivity of the pad test at 1.5 grams is 58.0% (95% CI 52.4, 63.5) and the specificity decreases to 54.2% (95% CI 44.3, 63.9). In the best scenario—ie, all those with a positive pad test had residual incontinence and all those with a negative pad test were continent, the proportion of women with continence is 72.6%, the sensitivity is 71.9% (95% CI 66.6, 76.8) and the specificity is 89.8% (95% CI 82.9, 94.6).
Discussion
Main Findings
In this study of women after VVF repair, over 90% experienced successful fistula closure during their first repair at our centre. Most women who returned for follow-up were continent, and 20% of women with a closed fistula at discharge had residual incontinence at follow-up. Nearly all women (94%) with a negative (<1.5 gram) pad test at discharge were continent at follow-up.
Strengths and Limitations
Few studies have evaluated post-operative predictors of continence after fistula repair. Rather, much focus has been paid to pre-operative factors, which have been well documented.13 In this study, we were able to evaluate how well a pad test can predict continence at various cut offs in a large population of women followed prospectively with a high follow-up rate within 120 days of VVF repair.
However, we acknowledge several limitations. We are not able to describe the nature of the residual incontinence apart from the incontinence grading by clinicians, as urodynamic testing is not routinely performed at follow-up visits. This may have led to the low prevalence of residual incontinence. Additionally, there may have been some social desirability bias among patients to report less incontinence to providers at follow-up. Women at high risk of residual incontinence (either from a residual fistula or a 1-hour pad test over 1.5 grams) were less likely to return for a scheduled clinical evaluation within 120 days of repair than those with a close fistula or negative discharge pad test. This may have also made our prevalence of residual incontinence at follow-up lower than expected, which would affect the positive and negative predictive values of the pad testing.
Interpretation
The optimal threshold for a positive or negative 1-hour pad test in a population of women with obstetric VVF repair has not been established. The International Continence Society recognizes an upper limit of 1.4 grams for continent women. Some studies in women after stress incontinence procedures have used a threshold of <1 gram for continent women,14 while others have chosen a threshold of <2 grams.15 The climate in which the test is performed may also impact the threshold for the pad test. A study from Brazil showed that pad weights are affected by temperature and humidity, which can increase perspiration.16 Given the amount of prior incontinence experienced by fistula patients, higher thresholds for pad tests (either 1.5 or 2.0 grams) may be more appropriate.
Though we show that a negative pad test may be a useful tool at predicting continued continence after VVF repair, a positive pad test does not predict residual incontinence well since many patients’ urinary leakage improves as time from repair increases. This is demonstrated by the low sensitivity and high specificity at predicting continence after repair. We found that many women who had incontinence at the time of discharge experienced improvement. Notably, many women with a positive 1-hour pad test went on to report that they were continent and cured. This is similar to the findings of VVF patients in Ethiopia where trends for improvement in continence grades were noted for most women in the initial months after of VVF repair.11
Our patients had a fistula closure rate of over 90%, marginally higher than the 85% closure rate recommended by the World Health Organization (WHO) as a quality of care measure.17 Other fistula surgeons have reported similar fistula closure rates18, 19 or lower closure rates.4, 20 Our closed fistula residual incontinence rate of 20% at the time of follow-up is comparable to rates found in other low resource settings where obstetric fistula is common.4, 21
Clinical follow-up rates for OF patients after repair is highly variable,11, 22, 23 and few sites where follow-up is performed have capabilities to perform urodynamic testing to further characterize the type of incontinence experienced. Post-operative incontinence in obstetric fistula patients with successful fistula closure, the so-called ‘continence gap’,24 remains one of the most vexing challenges in the care of women with this condition. Even among women with residual incontinence, patient perceptions of the amount of urinary leakage and the effect of incontinence on quality of life are important to understand and are areas for further study.
Loss to follow-up is a major limiting factor in other studies of continence after fistula repair. In other settings, patients with post-operative urinary leakage are either more motivated and likely to return for follow-up11 or just as likely to return for follow-up as those without leakage.22, 23 However, this was not true in our population of fistula patients. Further studies should consider innovative ways to capture women otherwise lost to follow-up after repair to characterize actual residual incontinence rates.
The ability to predict which patients are at low risk of residual incontinence is useful as it can help focus limited clinical resources appropriately to those who may be at risk. Women with an unrepaired fistula may be able to have another repair attempt or be considered for a urinary diversion. For women with residual incontinence after a successful OF repair, continence may be achieved with non-invasive techniques such as pelvic floor strengthening,25 bladder training, or urethral plugs.26 Additionally, surgical procedures to alleviate stress urinary incontinence can be considered for these patients.27 Informing patients of these possibilities may be useful to encourage clinical follow-up. Unlike another population of fistula patients in Ethiopia,11 our patients at risk for residual incontinence, either from an unrepaired fistula or other causes were significantly less likely to return for follow-up than those who were continent. This may be secondary to incomplete knowledge of future treatment options or other economic or social barriers that may be more common among these women. Further studies are needed to understand reasons for lower follow-up rates in these groups.
Conclusion
In this study, we have shown that the use of a noninvasive 1-hour pad test prior to discharge can assist in predicting which women will remain continent after repair. In settings where resources are limited and clinical follow-up of patients after fistula repair is challenging, the addition of the pad test may help to identify women who should be prioritized for follow-up after repair.
Supplementary Material
Distribution of the weights of post-operative 1-hour pad testing
Positive predictive value and negative predictive value for 1-hour pad test at 1.5 gram threshold, by prevalence. The reference line at 79.8% indicates the prevalence of continence in the study population
Continence grade, failed repairs, and urinary retention at discharge and follow-up (n=346)
Acknowledgments
The authors thank the patients and staff at the Freedom from Fistula Care Centre in Lilongwe, Malawi, UNC Project-Malawi, the Lilongwe District Health Management Team, and the following research assistants for their contributions to the study and assistance with recruitment and data collection, entry, and cleaning: William Nundwe, Charity Chisale, Rachel Hau, Sandra Ngwira, Sella Chisanga, Julia Ryan, Laura Drew, Allison Sih, and Magdalena Zgambo.
Funding
The funding for the implementation of this research study was by the Freedom from Fistula Foundation (FfFF), the UNC Department of OB-GYN, the Doris Duke Charitable Foundation, and the University of North Carolina, Johns Hopkins, Morehouse School of Medicine, and Tulane University NIH Fogarty International Center Grant #5R25TW009340. Support for use of the REDCap database was funded by grant [1UL1TR001111] from the North Carolina Clinical and translational Science Award program of the Division of Research Resources. Dr. Kopp’s research efforts were supported by NICHD training grant 5T32 HD075731-01 to the University of North Carolina-Chapel Hill.
Footnotes
Disclosure of interests
The authors declare that they have no competing interests. The ICMJE disclosure forms are available as online supporting information.
Contribution to authorship
DK conducted the data analysis with AB. DK drafted the manuscript. JPW conceptualized the study. DK, JW, EB, JT, and MM oversaw operational aspects of the study. All authors revised the manuscript and approved the final draft.
Details of ethical approval
Ethical approval was obtained from the National Health Sciences Research Committee of Malawi (Protocol #929, dated 25 August 2015) and the University of North Carolina School of Medicine Institutional Review Board (#11-2345, dated 6 January 2016). Women over 18 gave written informed consent, while those under 18 underwent parental consent and pediatric assent.
References
- 1.Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet. 2006 Sep 30;368(9542):1201–9. doi: 10.1016/S0140-6736(06)69476-2. [DOI] [PubMed] [Google Scholar]
- 2.Kalilani-Phiri LV, Umar E, Lazaro D, Lunguzi J, Chilungo A. Prevalence of obstetric fistula in Malawi. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2010 Jun;109(3):204–8. doi: 10.1016/j.ijgo.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Murray C, Goh JT, Fynes M, Carey MP. Urinary and faecal incontinence following delayed primary repair of obstetric genital fistula. BJOG: an international journal of obstetrics and gynaecology. 2002 Jul;109(7):828–32. doi: 10.1111/j.1471-0528.2002.00124.x. [DOI] [PubMed] [Google Scholar]
- 4.Matthieu LN, Jean N, Gunter DW, Dieter O, Augustin PM, Dirk DR. Obstetric fistula in a district hospital in DR Congo: Fistula still occur despite access to caesarean section. Neurourology and urodynamics. 2014 Apr 7; doi: 10.1002/nau.22601. [DOI] [PubMed] [Google Scholar]
- 5.Arrowsmith SD, Barone MA, Ruminjo J. Outcomes in obstetric fistula care: a literature review. Current opinion in obstetrics & gynecology. 2013 Oct;25(5):399–403. doi: 10.1097/GCO.0b013e3283648d60. [DOI] [PubMed] [Google Scholar]
- 6.Nielsen HS, Lindberg L, Nygaard U, Aytenfisu H, Johnston OL, Sorensen B, et al. A community-based long-term follow up of women undergoing obstetric fistula repair in rural Ethiopia. BJOG: an international journal of obstetrics and gynaecology. 2009 Aug;116(9):1258–64. doi: 10.1111/j.1471-0528.2009.02200.x. [DOI] [PubMed] [Google Scholar]
- 7.Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourology and urodynamics. 2010;29(1):213–40. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 8.Paick JS, Ku JH, Shin JW, Park K, Son H, Oh SJ, et al. Significance of pad test loss for the evaluation of women with urinary incontinence. Neurourology and urodynamics. 2005;24(1):39–43. doi: 10.1002/nau.20078. [DOI] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009 Apr;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krhut J, Zachoval R, Smith PP, Rosier PF, Valansky L, Martan A, et al. Pad weight testing in the evaluation of urinary incontinence. Neurourology and urodynamics. 2014 Jun;33(5):507–10. doi: 10.1002/nau.22436. [DOI] [PubMed] [Google Scholar]
- 11.Browning A, Menber B. Women with obstetric fistula in Ethiopia: a 6-month follow up after surgical treatment. BJOG: an international journal of obstetrics and gynaecology. 2008 Nov;115(12):1564–9. doi: 10.1111/j.1471-0528.2008.01900.x. [DOI] [PubMed] [Google Scholar]
- 12.Goh JT. A new classification for female genital tract fistula. The Australian & New Zealand journal of obstetrics & gynaecology. 2004 Dec;44(6):502–4. doi: 10.1111/j.1479-828X.2004.00315.x. [DOI] [PubMed] [Google Scholar]
- 13.Barone MA, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, Bello A, et al. Determinants of postoperative outcomes of female genital fistula repair surgery. Obstetrics and gynecology. 2012 Sep;120(3):524–31. doi: 10.1097/AOG.0b013e31826579e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brennand EA, Tang S, Williamson T, Birch C, Murphy M, Robert M, et al. Twelve-month outcomes following midurethral sling procedures for stress incontinence: impact of obesity. BJOG: an international journal of obstetrics and gynaecology. 2015 Nov;122(12):1705–12. doi: 10.1111/1471-0528.13132. [DOI] [PubMed] [Google Scholar]
- 15.Lo TS, Jaili S, Tan YL, Wu PY. Five-year follow-up study of Monarc transobturator tape for surgical treatment of primary stress urinary incontinence. Int Urogynecol J. 2016 Apr 16; doi: 10.1007/s00192-016-3019-3. [DOI] [PubMed] [Google Scholar]
- 16.Figueiredo EM, Gontijo R, Vaz CT, Baracho E, da Fonseca AM, Monteiro MV, et al. The results of a 24-h pad test in Brazilian women. Int Urogynecol J. 2012 Jun;23(6):785–9. doi: 10.1007/s00192-011-1645-3. [DOI] [PubMed] [Google Scholar]
- 17.Organization WH. Obstetric fistula: guiding principles for clinical management and programme development. Geneva, Switzerland: WHO; 2006. [DOI] [PubMed] [Google Scholar]
- 18.Tayler-Smith K, Zachariah R, Manzi M, van den Boogaard W, Vandeborne A, Bishinga A, et al. Obstetric fistula in Burundi: a comprehensive approach to managing women with this neglected disease. BMC pregnancy and childbirth. 2013;13:164. doi: 10.1186/1471-2393-13-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nardos R, Browning A, Chen CC. Risk factors that predict failure after vaginal repair of obstetric vesicovaginal fistulae. American journal of obstetrics and gynecology. 2009 May;200(5):578e1–4. doi: 10.1016/j.ajog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Kayondo M, Wasswa S, Kabakyenga J, Mukiibi N, Senkungu J, Stenson A, et al. Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urol. 2011;11:23. doi: 10.1186/1471-2490-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siddle K, Vieren L, Fiander A. Characterising women with obstetric fistula and urogenital tract injuries in Tanzania. Int Urogynecol J. 2014 Feb;25(2):249–55. doi: 10.1007/s00192-013-2185-9. [DOI] [PubMed] [Google Scholar]
- 22.McFadden E, Taleski SJ, Bocking A, Spitzer RF, Mabeya H. Retrospective review of predisposing factors and surgical outcomes in obstetric fistula patients at a single teaching hospital in Western Kenya. J Obstet Gynaecol Can. 2011 Jan;33(1):30–5. doi: 10.1016/S1701-2163(16)34769-7. [DOI] [PubMed] [Google Scholar]
- 23.Delamou A, Diallo M, Beavogui AH, Delvaux T, Millimono S, Kourouma M, et al. Good clinical outcomes from a 7-year holistic programme of fistula repair in Guinea. Trop Med Int Health. 2015 Jun;20(6):813–9. doi: 10.1111/tmi.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wall LL, Arrowsmith SD. The “continence gap”: a critical concept in obstetric fistula repair. Int Urogynecol J Pelvic Floor Dysfunct. 2007 Aug;18(8):843–4. doi: 10.1007/s00192-007-0367-z. [DOI] [PubMed] [Google Scholar]
- 25.Castille YJ, Avocetien C, Zaongo D, Colas JM, Peabody JO, Rochat CH. Impact of a program of physiotherapy and health education on the outcome of obstetric fistula surgery. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2014 Jan;124(1):77–80. doi: 10.1016/j.ijgo.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 26.Brook G, Tessema AB. Obstetric fistula: the use of urethral plugs for the management of persistent urinary incontinence following successful repair. Int Urogynecol J. 2013 Mar;24(3):479–84. doi: 10.1007/s00192-012-1887-8. [DOI] [PubMed] [Google Scholar]
- 27.Browning A. Prevention of residual urinary incontinence following successful repair of obstetric vesico-vaginal fistula using a fibro-muscular sling. BJOG: an international journal of obstetrics and gynaecology. 2004 Apr;111(4):357–61. doi: 10.1111/j.1471-0528.2004.00080.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distribution of the weights of post-operative 1-hour pad testing
Positive predictive value and negative predictive value for 1-hour pad test at 1.5 gram threshold, by prevalence. The reference line at 79.8% indicates the prevalence of continence in the study population
Continence grade, failed repairs, and urinary retention at discharge and follow-up (n=346)


