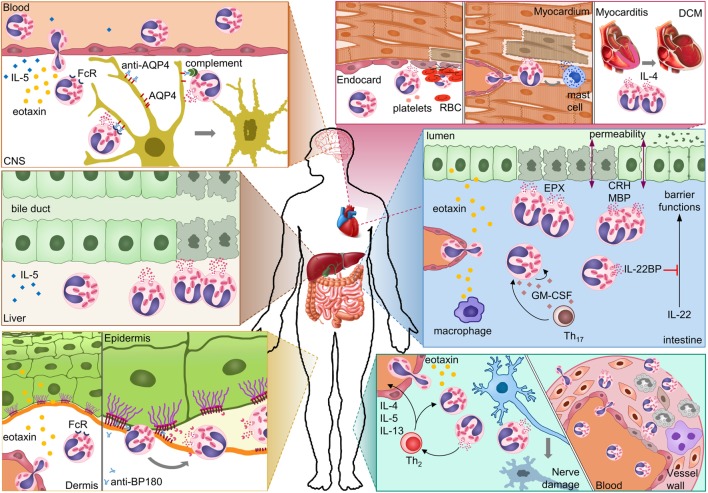
Figure 2.
Possible mechanisms of eosinophil-mediated damage in different autoimmune diseases. In neuromyelitis optica, eosinophils damage astrocytes through antibody-dependent and complement-dependent cell-mediated cytotoxicity. Eosinophil degranulation in damaged bile ducts was shown for primary biliary cirrhosis. In bullous pemphigoid, eosinophils release proteases that degrade the dermal–epidermal anchoring complex. Eosinophil infiltration in the heart results in damage to the endocardium and myocardium either directly or indirectly through mast cells. Eosinophil-derived IL-4 can drive progression from autoimmune myocarditis to DCM. In inflammatory bowel diseases, eosinophils can damage the mucosa through multiple mechanisms. Eosinophil granule proteins damage epithelial cells and increase epithelial barrier permeability. Eosinophil-derived IL-22BP blocks the protective effects of IL-22 on epithelial cells. GM-CSF may prolong survival and activation of eosinophils in the intestine. In eosinophilic granulomatosis with polyangiitis, eosinophils damage nerves and blood vessels. Abbreviations: CNS, central nervous system; AQP4, aquaporin 4; FcR, Fc receptor; BP180, bullous pemphigoid 180; RBC, red blood cell; DCM, dilated cardiomyopathy; EPX, eosinophil peroxidase; CRH, corticotropin-releasing hormone; MBP, major basic protein; IL-22BP, IL-22-binding protein; GM-CSF, granulocyte-macrophage colony-stimulating factor; Th17, T-helper 17 cell; Th2, T-helper 2 cell.