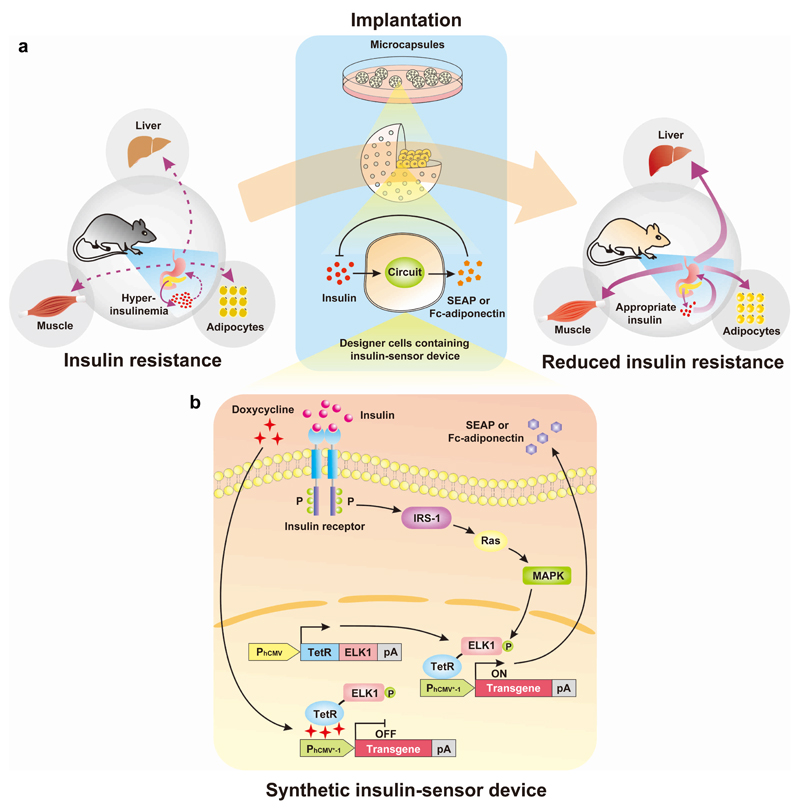
Figure 1. Synthetic insulin-sensitizing designer circuit for the treatment of insulin resistance.
(a) Functional and therapeutic features. Insulin resistance is characterized by the insensitivity of liver, muscle and adipocytes to blood insulin levels, which prevents cellular glucose uptake and leads to hyperinsulinaemia. The designer circuit quantifies blood insulin levels, detects hyperinsulinaemia and triggers dose-dependent adiponectin expression, which restores insulin sensitivity and attenuates the insulin-resistance syndrome. (b) Synthetic insulin-sensitizing designer cascade. The binding of insulin to the tyrosine kinase family human insulin receptor (IR) triggers autophosphorylation on multiple tyrosine residues in the IR, leading to the phosphorylation of cellular proteins such as insulin receptor substrate 1 (IRS-1). Upon tyrosine phosphorylation, these proteins interact with signaling molecules through their SH2 domains, resulting in subequent activation of Ras (a GTPase) and mitogen-activated protein kinase (MAPK). The activated MAPK enters the nucleus and phosphorylates the synthetic hybrid transcription factor, TetR-ELK1, consisting of the doxycycline-responsive DNA-binding Tet repressor (TetR) fused to the regulated activation domain of the transcription factor, ELK1, which is driven by the constitutive human cytomegalovirus immediate early promoter (PhCMV). In the basal state, TetR-ELK1, is able to bind to PhCMV*-1, a chimeric promoter containing a TetR-specific heptameric operator module (tetO7) linked to a minimal version of PhCMV (PhCMVmin), but the ELK1 domain remains inactive. Only the phosphorylation of TetR-ELK1’s ELK1 domain by upstream MAPK activity during cell signaling leads to PhCMV*-1-driven expression of the desired transgene. The addition of doxycycline disrupts the interaction between TetR-ELK1’s TetR domain and the tetO7 operator of PhCMV*-1, preventing the hybrid transcription factor from mediating the transgene expression, regardless of its phosphorylation state. When set to produce a therapeutic protein such as adiponectin that is secreted into the bloodstream the designer cascade turns into a closed-loop prosthetic network that increases the sensitivity of liver, adipose and muscle tissues to insulin which attenuates insulin release by pancreatic beta cells and reverses the insulin resistance syndrome.