KEY TEACHING POINTS.
|
Introduction
Heart perforation after pacemaker implantation is a rare but life-threatening complication.1 The number of pacemaker and defibrillator implantations is increasing annually2; thus, the rate of heart perforation–related complications will become more frequent in the future.3 We report a case of totally thoracoscopic management of a superior vena cava perforation with a pacemaker lead.
Case report
An 83-year-old man was an emergency referral to our institute from the heart rhythm department of another clinic. Fifteen days prior, he underwent atrioventricular pacemaker implantation (Medtronic Sensia DR; Medtronic Inc, Minneapolis, MN) because of sick sinus syndrome with active fixation of an atrial lead (Flextend 2, Model 4096; Boston Scientific, St Paul, MN) and passive fixation of a ventricular lead (Fineline II, Model 4457; Boston Scientific). The following day, the pacemaker control presented abnormal sensing and pacing parameters of the atrial lead; thus, repositioning of the lead was performed. Four days later, repositioning of both leads was required. Subsequently, the patient’s condition became stable, but he had a subfebrile temperature. Antibiotic therapy was performed without effect. Chest x-ray and transthoracic echocardiography showed right-side hemothorax. Pleural puncture was performed and 1000 mL of hemorrhagic liquid was removed. On the same day, the patient was emergently transferred to our clinic. On admission, the patient was hemodynamically stable. The pacemaker control presented normal sensing and pacing parameters of the ventricular lead and loss of atrium capture during maximum output pacing and diaphragm stimulation. Transthoracic echocardiography revealed insignificant pericardial effusion and right hemothorax up to 10.0 cm. Computed tomography revealed atrial lead migration into the right pleural cavity with right hemothorax (Figure 1). During the pleural puncture, an additional 600 mL of hemorrhagic liquid was removed. The case was discussed by a multidisciplinary team that included a cardiac surgeon, an electrophysiologist, and an anesthetist. Considering the signs of continued bleeding, the patient was taken to the hybrid operating room. The right thoracoscopiс approach with single-lung ventilation was performed. The 10-mm port for the camera was inserted in the fourth intercostal space on the anterior axillary line. Furthermore, 2 5-mm ports for the endoscopic instruments were used (in the third and fifth intercostal spaces anterior to the anterior axillary line). Carbon dioxide was insufflated into the pleural cavity during the operation. Simultaneously, the electrophysiology team opened the pacemaker pocket in the left subclavian region.
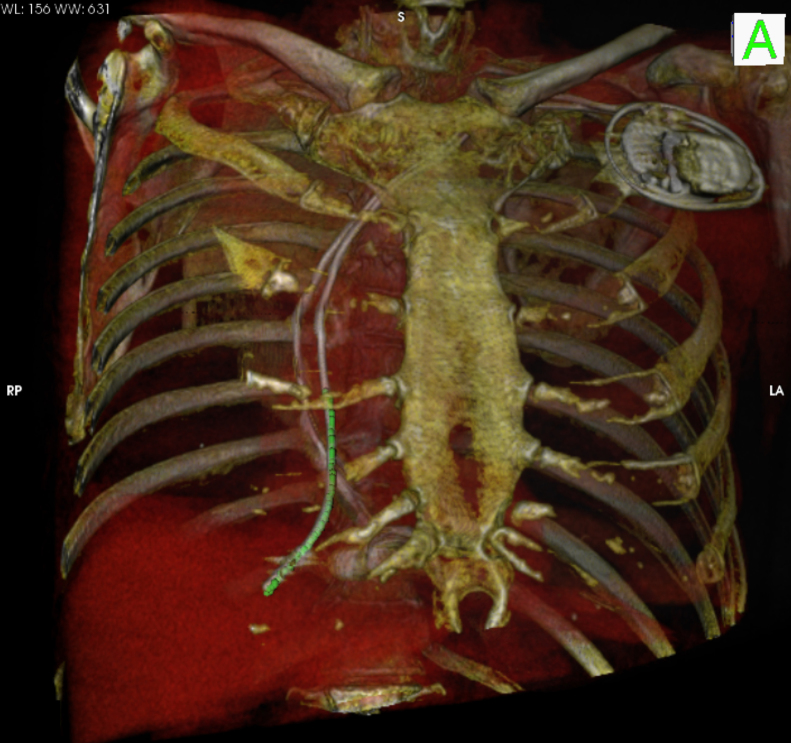
Figure 1.
Computed tomographic 3-dimensional reconstruction scan showing the atrial lead migration into the right pleural cavity. LA = left anterior; RP = right posterior.
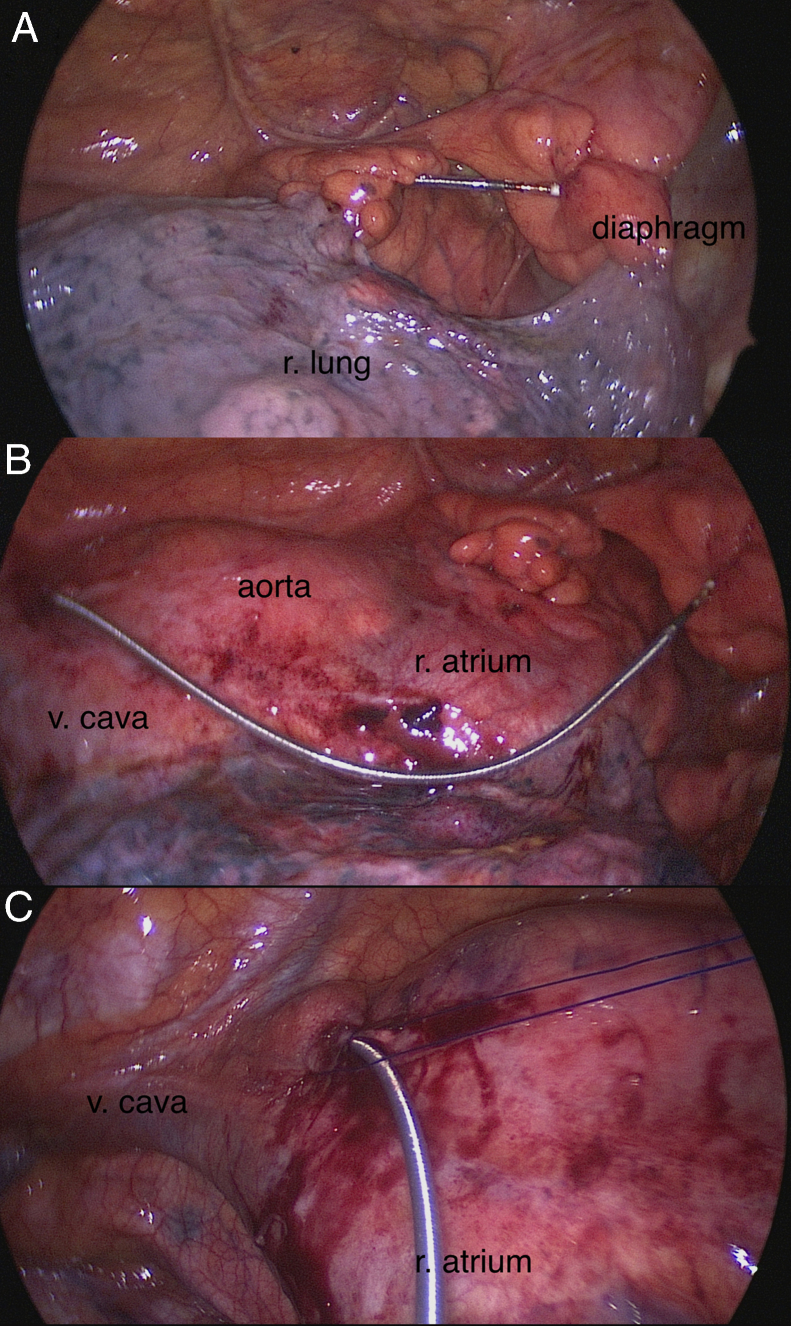
The perforation was found to be located in the extrapericardial part of the superior vena cava (site of connection with the innominate vein), along with pacemaker lead migration into the right pleural cavity but without active bleeding (Figure 2A and B). The pericardium was opened, and no evidence of hemopericardium was found. A purse-string suture was placed around the vena cava perforation using 4/0 polypropylene (Premilene; B. Braun Melsungen AG, Melsungen, Germany; Figure 2C). The lead was removed under visual control, and the suture was tied. Then, a new atrial lead (Medtronic CapSureFix Novus, 5076; Medtronic Inc) was implanted, under fluoroscopic control, to the lateral wall of the right atrium with active fixation. Normal sensing and pacing parameters were achieved. The atrial pacing threshold and impedance were 0.6 V/0.5 ms and 450 ohms, respectively. The ventricular lead pacing threshold was 0.9 V/0.5 ms, and pacing impedance was 520 ohms. The control revision showed complete hemostasis. One drainage tube was placed into the pleural cavity. The patient was transported to the intensive care unit. He was extubated 3 hours later and transferred to the general ward 12 hours postoperatively. The postoperative course was uneventful. The patient was discharged 4 days after surgery in good condition and with normal functioning of the pacemaker.
Figure 2.
Intraoperative photographs. A, B: Perforation of the extrapericardial part of the superior vena cava with pacemaker lead migration into the right pleural cavity. C: The suture placed around the vena cava perforation.
Discussion
Cardiac perforation by pacemaker leads is a rare complication, with an incidence of 0.3%–1%.1, 4 Perforations of the right atrium and ventricle are more common than that of the superior vena cava.5 These perforations frequently occur at the time of pacemaker implantation or during the first days after procedure.1, 6, 7 However, cases of delayed lead perforations have also been described in the literature.8, 9 Risk factors for lead perforation are older age, female sex, body mass index of <20 kg/m², active lead fixation, implantable cardioverter-defibrillator, use of corticosteroids within 7 days, and an inexperienced operator.10 The clinical characteristics of cardiac perforation after pacemaker implantation vary significantly.5 In most cases of acute perforations, cardiac tamponade and sudden cardiac death occur. By contrast, delayed lead perforations may be asymptomatic.4 The patient in the present case had several risk factors, including older age, low body mass index (20.2 kg/m²), and active lead fixation. The perforation probably occurred at the time of lead repositioning. However, it was diagnosed only after 10 days because the only clinical symptom was subfebrile temperature. The unclear symptomatic nature of this perforation is explained by its atypical locus (the extrapericardial part of the superior vena cava), without pericardial effusion and cardiac tamponade. The atrial lead dysfunction and the computed tomography data allowed us to establish the correct diagnosis.
According to published data in the literature, the most frequently used method for lead perforation treatment is percutaneous lead extraction with transesophageal echocardiographic monitoring.5, 11 For unstable patients and difficult cases (lead migration from the pericardium, injury to other organs, etc), open surgery is performed.5 Hussain et al12 presented a case of successful minimally invasive, robotically assisted repair of a right atrium perforation. Another alternative method is to use a thoracoscopic approach. We have extensive experience with totally thoracoscopic epicardial atrial fibrillation ablation and thoracoscopic pericardiectomy in patients with pericarditis. This experience enabled us to use an endoscopic approach for lead perforation management. In comparison with percutaneous lead extraction, thoracoscopy allows the repair of perforations under visual control while preventing possible complications (continuous bleeding with development of cardiac tamponade). Both thoracoscopy and the conventional approach provide excellent visualization. However, avoiding sternotomy decreases the frequency of wound infection complications, length of mechanical ventilation, duration of intensive care unit and hospital stay, and pain intensity, which is especially important in elderly patients. Moreover, in comparison with the robotic-assisted surgery, thoracoscopy is a more accessible and reproducible method with significant economic benefit. Operating in a hybrid operating room makes it possible to eliminate life-threatening complications and simultaneously reposition or reimplant the lead with physiological pacing recovery.
The patient in this case was hemodynamically stable; therefore, the thoracoscopic approach was chosen. In urgent situations, a sternotomy is the preferred approach because it can be performed in the shortest time and allows repair of heart perforations in any location. Moreover, in patients who are hemodynamically unstable, carbon dioxide insufflation into the pleural cavity during the thoracoscopic approach is contraindicated because of significant mediastinum dislocation and hemodynamic disorders.
Conclusion
In conclusion, this case demonstrates that the totally thoracoscopic approach is a feasible option for lead perforation treatment in clinics with elective thoracoscopic cardiac surgery experience.
References
- 1.Hirschl D.A., Jain V.R., Spindola-Franco H., Gross J.N., Haramati L.B. Prevalence and characterization of asymptomatic pacemaker and ICD lead perforation CT. Pacing Clin Electrophysiol. 2007;30:28–32. doi: 10.1111/j.1540-8159.2007.00575.x. [DOI] [PubMed] [Google Scholar]
- 2.Brignole M., Auricchio A., Baron-Esquivias G. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA) Eur Heart J. 2013;34(29):2281–2329. doi: 10.1093/eurheartj/eht150. [DOI] [PubMed] [Google Scholar]
- 3.Satpathy R., Hee T., Esterbrooks D., Mohiuddin S. Delayed defibrillator lead perforation: an increasing phenomenon. Pacing Clin Electrophysiol. 2008;31:10–12. doi: 10.1111/j.1540-8159.2007.00919.x. [DOI] [PubMed] [Google Scholar]
- 4.Khan M.N., Joseph G., Khaykin Y., Ziada K.M., Wilkoff B.L. Delayed lead perforation: a disturbing trend. Pacing Clin Electrophysiol. 2005;28:251–253. doi: 10.1111/j.1540-8159.2005.40003.x. [DOI] [PubMed] [Google Scholar]
- 5.Refaat M.M., Hashash J.G., Shalaby A.A. Late perforation by cardiac implantable electronic device leads: clinical presentation, diagnostic clues, and management. Clin Cardiol. 2010;33(8):466–475. doi: 10.1002/clc.20803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkfeldt R.E., Johansen J.B., Nohr E.A., Moller M., Arnsbo P., Nielsen J.C. Risk factors for lead complications in cardiac pacing: a population-based cohort study of 28,860 Danish patients. Heart Rhythm. 2011;8:1622–1628. doi: 10.1016/j.hrthm.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Koyama S., Itatani K., Kyo S., Aoyama R., Ishiyama T., Harada K., Ono M. Subacute presentation of right ventricular perforation after pacemaker implantation. Ann Thorac Cardiovasc Surg. 2013;19(1):73–75. doi: 10.5761/atcs.cr.11.01863. [DOI] [PubMed] [Google Scholar]
- 8.Haque A., Roy S., Biswas B. Perforation by permanent pacemaker lead: how late can they occur? Cardiol J. 2012;19(3):326–327. doi: 10.5603/cj.2012.0059. [DOI] [PubMed] [Google Scholar]
- 9.Alla VM, Reddy YM, Abide W, Hee T, Hunter C. Delayed lead perforation: can we ever let the guard down? Cardiol Res Pract. 〈DOI:10.4061/2010/741751〉. [DOI] [PMC free article] [PubMed]
- 10.Mahapatra S., Bybee K.A., Bunch T.J., Espinosa R.E., Sinak L.J., McGoon M.D., Hayes D.L. Incidence and predictors of cardiac perforation after permanent pacemaker placement. Heart Rhythm. 2005;2(9):907–911. doi: 10.1016/j.hrthm.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Rydlewska A., Małecka B., Zabek A., Klimeczek P., Lelakowski J., Pasowicz M., Czajkowski M., Kutarski A. Delayed perforation of the right ventricle as complication of permanent cardiac pacing – is following the guidelines always the right choice? Non-standard treatment – a case report and literature review. Kardiol Pol. 2010;68(3):357–361. [PubMed] [Google Scholar]
- 12.Hussain S., Adams C., Mechulan A., Leong-Sit P., Kiaii B. Minimally invasive robotically assisted repair of atrial perforation from a pacemaker lead. Int J Med Robot. 2012;8(2):243–246. doi: 10.1002/rcs.459. [DOI] [PubMed] [Google Scholar]