KEY TEACHING POINTS
|
Introduction
Pulmonary vein isolation (PVI) is the cornerstone of catheter ablation for atrial fibrillation (AF), especially in paroxysmal AF patients.1 In addition to a radiofrequency ablation catheter, a cryoballoon has been proven as an effective technology in PVI for AF. Recently several randomized trials have shown that cryoballoon ablation was noninferior to radiofrequency ablation with respect to efficacy for the treatment of patients with drug-refractory paroxysmal AF, and there was no significant difference between the 2 methods with regard to overall safety.2, 3 Pulmonary vein (PV) stenosis was one of the major complications after PVI.
Case report
A 47-year-old man with paroxysmal AF was referred for catheter ablation. Preoperative contrast-enhanced multidetector computed tomography revealed the presence of persistent left superior vena cava (PLSVC). After informed consent from the patient was obtained, cryoballoon ablation of the paroxysmal AF was performed.
Before cryoballoon ablation, a complete seal of the venous return by the cryoballoon (28-mm, second-generation cryoballoon, Medtronic Inc., Minneapolis, MN) was confirmed with contrast injection in each vein. In the left superior pulmonary vein (LSPV), the first freezing attempt was terminated at 45 seconds owing to an insufficient temperature drop, followed by successful additional attempts at freezing (180 and 120 seconds, minimum temperature of -48°C; fluoroscopic image in Supplemental Figure 1 and details of freezing in Supplemental Tables, available online). In the remaining 3 PVs, 2 sequential freezing attempts (180 and 120 seconds) were successfully performed. No atrial arrhythmia was induced at the end of the procedure.
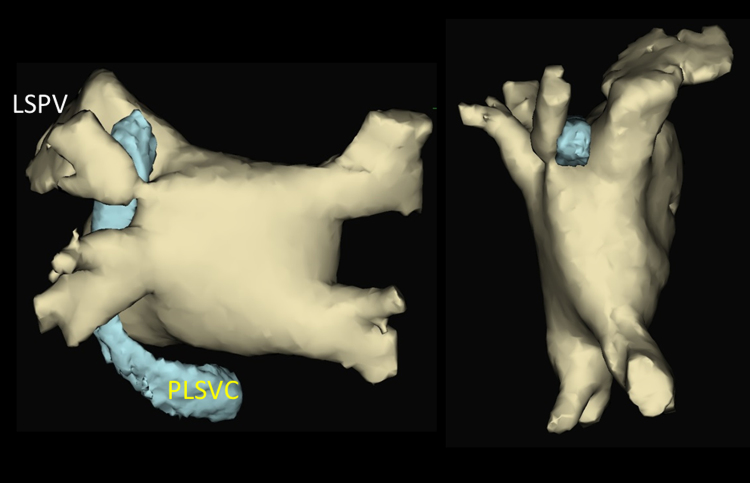
Although he had no AF recurrence thereafter, multidetector computed tomography at 3 months revealed significant LSPV stenosis (≈80% in LSPV, Figure 1). The site of PV stenosis was located right behind the PLSVC.
Figure 1.
The 3-D images of the left atrium (posteroanterior and top view) constructed by multidetector computed tomography after the procedure demonstrated severe left superior pulmonary vein (LSPV) stenosis immediately posterior to the persistent left superior vena cava (PLSVC).
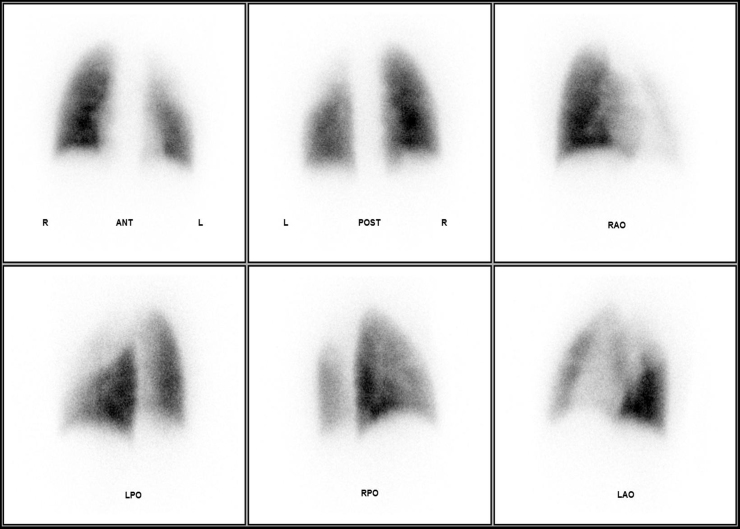
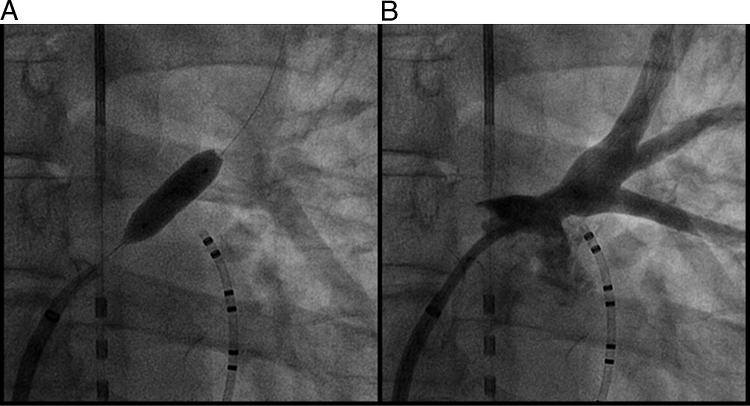
Although the patient remains free from any symptoms attributable to PV stenosis, there was reduction in perfusion to the left upper lobe (Figure 2). We decided to perform an intervention to the LSPV before the patient manifested symptoms. Heparin (100 IU/kg body weight) was administered immediately after venous access was obtained; heparinized saline was also infused to maintain an activated clotting time of 300–350 seconds during both cryoballoon ablation and PV angioplasty. Intravascular ultrasound (Eagle Eye, Volcano Corporation, Rancho Cordova, CA) showed no thrombus in the PV. A successful balloon angioplasty (Sterling, 8.0 × 20 mm, Boston Scientific, Marlborough, MA) was performed with use of the intravascular ultrasound (Figure 3). No complication occurred during PV intervention. After balloon angioplasty, the percentage stenosis improved from 78% pre-intervention to 40%.
Figure 2.
Tc-99m macroaggregated albumin perfusion images are shown. There is reduced perfusion in the left upper lobe. ANT = anterior; LAO = left anterior oblique; LPO = left posterior oblique; POST = posterior; RAO = right anterior oblique; RPO = right posterior oblique.
Figure 3.
A: Balloon dilation in the left superior pulmonary vein and B: angiography in the left superior pulmonary vein after venoplasty.
Discussion
The incidence of PV stenosis by cryoballoon ablation is approximately 3.1% using a first-generation balloon (most of which were treated by a 23-mm balloon).4 A second-generation balloon has been regarded to be a safer tool, with phrenic nerve damage as the only major complication.5 Two recent multicenter randomized trials reported no PV stenosis after second-generation cryoballoon PVI.2, 3 However, this case warns us that there may be an unavoidable risk of PV stenosis during cryoballoon ablation, even with a 28-mm, second-generation cryoballoon. In our over 200 cases of experience, this is the only single case with PV stenosis after second-generation cryoballoon ablation. During LSPV isolation, the bottom of the PV ostium was lifted up by the cryoballoon (Supplemental Figure 1). The high pressure used to occlude the PV might have caused the PV stenosis. Whether the presence of an adjacent PLSVC increases the risk of PV stenosis after cryoballoon ablation remains unclear; however, this possibility warrants consideration for further investigation.
In this case, the patient had no symptoms throughout the entire period. PV stenosis was asymptomatic in 60% of cases. The frequent symptoms were dyspnea on exertion (83%), followed by dyspnea at rest (30%), recurrent cough (39%), chest pain (26%), flulike symptoms (13%), and hemoptysis (13%).6, 7 A decision to perform PV angioplasty in an asymptomatic patient is challenging. However, if intervention is not attempted before complete occlusion develops the opportunity to act may be lost.7
The previous study reported that long-term (a mean of 25 months of follow-up) restenosis requiring intervention was lower after stent angioplasty than balloon angioplasty, and time free from restenosis was significantly longer for stent angioplasty than for balloon dilation (HR for balloon dilation 2.6, P = .003).8 However, it remains controversial owing to a lack of randomized data.
Conclusion
This case illustrates the successful angioplasty for LSPV stenosis after cryoballoon ablation.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.hrcr.2016.08.011.
Appendix. Supplementary data
Supplemental Figure 1 Fluoroscopic images during each application of the left superior pulmonary vein are shown. AP = anteroposterior; LAO = left anterior oblique.
References
- 1.Haïssaguerre M., Jaïs P., Shah D.C., Takahashi A., Hocini M., Quiniou G., Garrigue S., Le Mouroux A., Le Métayer P., Clémenty J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–666. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 2.Kuck K.H., Brugada J., Fürnkranz A. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–2245. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 3.Luik A., Radzewitz A., Kieser M. Cryoballoon versus open irrigated radiofrequency ablation in patients with paroxysmal atrial fibrillation: the prospective, randomized, controlled, noninferiority FreezeAF study. Circulation. 2015;132:1311–1319. doi: 10.1161/CIRCULATIONAHA.115.016871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Packer D.L., Kowal R.C., Wheelan K.R. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STP AF) Pivotal Trial. J Am Coll Cardiol. 2013;61:1713–1723. doi: 10.1016/j.jacc.2012.11.064. [DOI] [PubMed] [Google Scholar]
- 5.Martins R.P., Hamon D., Césari O., Behaghel A., Behar N., Sellal J.M., Daubert J.C., Mabo P., Pavin D. Safety and efficacy of a second-generation cryoballoon in the ablation of paroxysmal atrial fibrillation. Heart Rhythm. 2014;11:386–393. doi: 10.1016/j.hrthm.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Pürerfellner H., Martinek M. Pulmonary vein stenosis following catheter ablation of atrial fibrillation. Curr Opin Cardiol. 2005;20:484–490. doi: 10.1097/01.hco.0000179816.80576.3c. [DOI] [PubMed] [Google Scholar]
- 7.Baranowski B., Saliba W. Our approach to management of patients with pulmonary vein stenosis following AF ablation. J Cardiovasc Electrophysiol. 2011;22:364–367. doi: 10.1111/j.1540-8167.2010.01981.x. [DOI] [PubMed] [Google Scholar]
- 8.Prieto L.R., Schoenhagen P., Arruda M.J., Natale A., Worley S.E. Comparison of stent versus balloon angioplasty for pulmonary vein stenosis complicating pulmonary vein isolation. J Cardiovasc Electrophysiol. 2008;19:673–678. doi: 10.1111/j.1540-8167.2008.01110.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1 Fluoroscopic images during each application of the left superior pulmonary vein are shown. AP = anteroposterior; LAO = left anterior oblique.