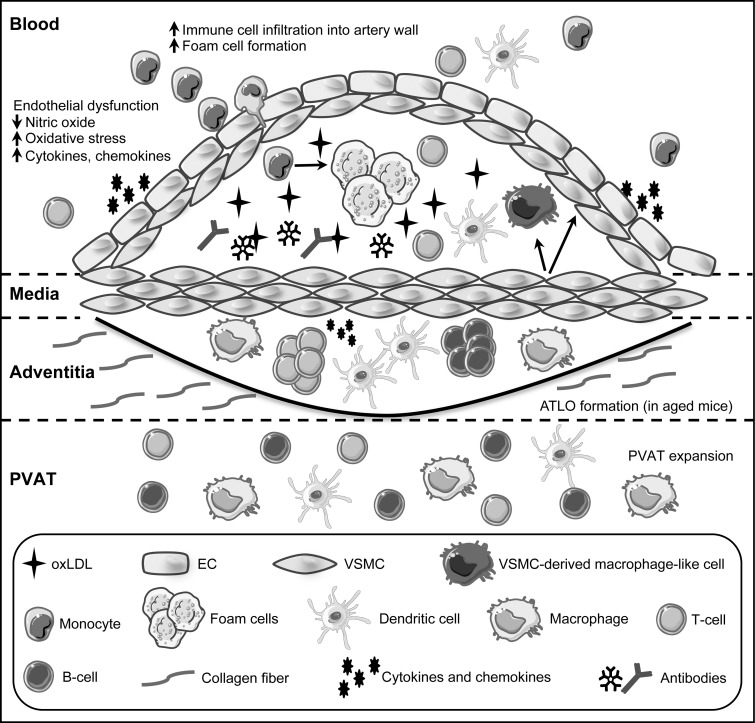
FIG. 1.
Cell types and structure of the vessel wall in atherosclerosis. During atherosclerosis, buildup of oxidized low-density lipoprotein (oxLDL) in the arterial intima leads to endothelial cell dysfunction. The resulting inflamed endothelium secretes inflammatory cytokines, chemokines and presents adhesion molecules that recruit circulating immune cells into the artery wall. Monocytes that transmigrate into the subendothelial space take up oxLDL and differentiate into lipid-laden macrophages (foam cells). Immune components, including dendritic cells, T cells, and B cell antibodies that are specific for oxLDL, accumulate as the lesion expands, having both pro- and anti-inflammatory effects, depending on cell type. A subset of vascular smooth muscle cells (VSMC) enters a proliferative state and migrates to form the fibrous cap, whereas other SMC phenotypically switch into macrophage-like cells within lesions. Pro- and anti-inflammatory immune cell subsets are present within the adventitia and perivascular adipose tissue (PVAT) at homeostasis. These cells increase in number in response to atherogenic stimuli and organize to form arterial tertiary lymphoid organs (ATLO) with distinct B cell and T cell zones that are similar to secondary lymphoid organs in aged mice.