Abstract
Background
The purposes of this study, performed on a large sample of cancer patient-caregiver dyads, were: i) to simultaneously investigate, using an individualized quality of life (QoL) measure (Schedule for the Evaluation of Individual QoL, SEIQoL), the QoL domains freely expressed by cancer patients and their caregivers, and ii) to explore overlapping between the SEIQoL assessment and QoL assessment using traditional instruments.
Methods
The study employed a cross-sectional design including cancer patients who were going to receive chemotherapy treatment and their caregivers. Quality of life was assessed using condition-specific questionnaires (EORTC QLQ-C30 and CarGOQoL), generic health-related questionnaire (SF-36), and open individualized measure (SEIQoL).
Results
The final sample included 205 patient-caregiver dyads. From the SEIQoL, Family, Health, and Leisures were the most freely expressed QoL domains by patients and caregivers, but reported with different weights. Love life and financial issues were less spontaneously mentioned. The SEIQoL index was moderately correlated to the condition-specific QoL questionnaires (R lower than |0.40|) and to SF-36 (correlation coefficients: R ranging from 0.17 to 0.31).
Conclusion
Individualized QoL measures allow individuals to spontaneously express important, non-predefined domains. This study highlights the need to explore QoL using a combination of individualized questionnaires and standardized questionnaires, capturing complementary facets that patients consider important in their life.
Background
Studies examining health-related quality of life (QoL) have typically used standardized measures, called disease- or condition-specific, or generic measures [1]. These traditional standardized instruments usually include a pre-defined set of items exploring pre-defined domains and have been criticized for potentially missing important domains for assessing an individual’s QoL or including less important domains. To overcome this limitation, individualized measures or patient-generated QoL procedures have been developed, enabling respondents to spontaneously identify which aspects of their lives are actually relevant to their QoL. Thus, individual QoL assessment does not impose any predetermined external value system regarding either the choice of relevant domains or their actual significance for people [2]. This approach seems more suitable than standardized measures in capturing a patient’s actual perspectives [3].
During the last decade, an individualized open QoL measure has been developed, the Schedule for the Evaluation of Individual QoL - Direct Weighting (SEIQoL-DW), which was derived from the original SEIQoL [4–6]. The SEIQoL-DW assesses the individuals’ perception of his or her present QoL and allows the individual to choose the domains to be evaluated followed by a weighting procedure resulting in qualitative and quantitative outcomes. The SEIQoL-DW involves a semi-structured interview to enable individuals to spontaneously and freely name areas that appear important in life. The SEIQoL-DW has been reported as a feasible and valid instrument used in quantitative research [2, 7–9] and outside the research setting [10], with a limited burden on participants [3]. The SEIQoL-DW has proven to be a reliable measure in various populations [3].
SEIQoL-DW has been validated among numerous sick and healthy populations [6, 8, 11, 12], including patients with severe illnesses [2, 13]. The SEIQoL-DW has also been used as the primary outcome in recent large randomized controlled trials focusing on palliative care [14] and multiple sclerosis patients [15]. While the use of the SEIQoL-DW is recognized, few studies have provided SEIQoL-DW data for specific caregivers populations [16, 17]; to our knowledge, only one study, performed on amyotrophic lateral sclerosis patients, simultaneously provided the QoL of caregivers and patients using SEIQoL-DW [18, 19]. Moreover, few studies have explored links between QoL assessment using traditional standardized instruments and individualized measures, neither among patients nor caregivers.
In this context, the purposes of the present study, performed on a large sample of cancer patient-caregiver dyads, were to: i) simultaneously investigate, using the SEIQoL-DW, the QoL domains freely expressed by cancer patients and their caregivers, and ii) explore overlapping between the SEIQoL and traditional instruments.
Methods
Setting
The present study employed a cross-sectional design including cancer patients administered chemotherapy treatment and their caregivers from two French Public Academic Teaching Hospitals (the Oncology and Therapeutic Innovations Department, North Hospital, Marseille, and the Neuro-Oncology Department, Timone Hospital, Marseille). The participating oncologic departments treated patients presenting predominantly lung cancer, prostate/urologic cancer, breast cancer, and genital cancer.
Population
The population included patient-caregiver dyads. The following inclusion and exclusion criteria of the dyads were considered:
Patients: individuals 18 years of age or older, having a cancer defined by histology whatever the origin of the primitive, loco-regionally advanced or metastatic cancer, with an indication of chemotherapy, and able to speak/read French.
Caregivers: individuals 18 years of age or older, designated as the primary caregiver by the patient, able to speak/read French, and free from cancer comorbidity.
Ethics approval and consent to participate
All patients were fully informed of the study and provided written informed consent. The protocol was approved by the ethics committees of Aix-Marseille University, France (reference number: 2014-09-30-05).
Data collection and measures
The data for age, gender, educational level, marital status, and professional status were collected for both patient and caregiver. The relationship between the patient and the caregiver was determined: partners, children/parents, brother/sister, and others. For the patient, the localization of cancer, the WHO performance status, and the presence of nodes/metastasis were assessed.
Quality of life
Specific QoL questionnaires were administered: the European Organization for Research and Treatment of Cancer quality of life questionnaire (EORTC QLQ-C30) for patients, and the CareGiver Oncology Quality of Life questionnaire (CarGOQoL) for caregivers. Generic QoL questionnaires were administered to patients and caregivers: the SEIQoL and the Short Form 36 (SF-36).
The EORTC QLQ-C30 is a disease-specific questionnaire assessing the QoL of cancer patients [20]. It includes 30 items describing five functional scales (physical, role, emotional, cognitive, and social), nine symptom scales and single symptom items, and a global health status scale. The scores range from 0 to 100 for each scales/item. A high score for a functional scale represents a high/healthy level of functioning, a high score for the global health status scale represents a high QoL, and a high score for a symptom scale represents a high level of symptomatology.
The CarGOQoL is a well-validated condition-specific questionnaire for caregivers of cancer patients [21]. It includes 29 items describing 10 dimensions: psychological well-being, burden, relationship with health care, administration and finances, coping, physical wellbeing, self-esteem, leisure time, social support and private life. An index was computed. All dimension scores and the index are indicated on a 0–100 scale. A higher score indicates a better QoL.
The SF-36 is a generic health-related QoL questionnaire [22], including 36 items describing eight subscales (Physical function, Social functioning, Role physical, Role emotional, Mental health, Vitality, Body pain and General health), yielding two component summary measures (physical and mental composite scores, PCS-SF36 and MCS-SF36). The SF-36 scoring ranges from 0 (lowest) to 100 (highest QoL level).
The procedure of QoL assessment using the SEIQoL-DW involves a semi-structured interview and follows 3 steps. First the participant is invited to nominate the ‘5 domains’ he/she currently consider to be the most important in his/her life at the time of the assessment. If he/she finds it difficult to nominate the 5 domains, then a standard list of prompts is proposed. Second, the participant is also asked to rate the importance of each nominated domain on a visual analogue scale from 0 (lowest) to 100 (highest importance): the SEIQoL-VAS. Third the participant is asked for the relative importance of each area by a weighting procedure; the participant should quantify the relative importance of each of the 5 nominated areas, where all areas add up to 100: the SEIQoL-weight. The initial patient’s information was transcribed and analyzed by a psychologist (TL) experienced in categorizing patient comments into major themes. He aggregated the original information into 8 mains domains (cues) based on similar meanings. An overall index was obtained by summing the products of the rating (SEIQoL-VAS) with the weight (SEIQoL-weight) of each domain.
Data analysis
The number of patients and caregivers with expressed domains from the SEIQoL were counted. For each domain, the median scores (raw and weighted scores) were provided for patients and caregivers, and the proportions of dyads (patient and caregiver) expressing these domains were provided. For dyads with common domains expressed by both patient and caregiver, scores and weights were compared using Wilcoxon tests. Spearman’s correlations between SEIQoL index and other standardized QoL scores (SF-36, EORTC QLQ-C30, and CarGOQoL) were provided.
Results
Characteristics of patient–caregivers dyads
Among the 388 cancer patients participating in the present study, 205 individuals who completed the SEIQoL-DW were able to nominate a caregiver agreeing to participate. Therefore, the final sample in the present study comprised 205 patient-caregiver dyads. For patients, the mean time since diagnosis was 39 days (Standard deviation 35.1). Approximately, 28% of the patients were diagnosed with lung cancer, 20% of the patients were diagnosed with gynecologic cancer and 10% of the patients were diagnosed with urologic cancer. The relationships between the patients and caregivers were partner relations for 61% of cases. All patient and caregiver characteristics are presented in Table 1.
Table 1.
Main characteristics of the 205 patient-caregiver dyads
| N (%) | MD | ||
|---|---|---|---|
| M ± SD | % | ||
| 1. Patients | |||
| Age | Years | 61.5 ± 11.7 | 7.8 |
| Gender | Woman | 91 (44.4) | 0 |
| Man | 114 (55.6) | ||
| Educational level | <12 years | 108 (58.1) | 9.3 |
| > = 12 years | 78 (41.9) | ||
| Marital status | Single | 51 (26.2) | 4.9 |
| Couple | 144 (73.8) | ||
| Professional status | Worker | 55 (33.1) | 19.0 |
| Not worker | 111 (66.9) | ||
| Localization of cancer | Lung | 56 (28.3) | 3.4 |
| Head and neck | 51 (24.8) | ||
| Gynecologic | 39 (19.7) | ||
| Urologic | 21 (10.6) | ||
| Soft tissue sarcoma | 8 | ||
| Digestive | 7 | ||
| Dermatologic | 6 | ||
| Lymphoma | 3 | ||
| Bone | 3 | ||
| Adrenal | 2 | ||
| Undefined | 2 | ||
| WHO Performans status | 0 | 125 (63.5) | 3.9 |
| > = 1 | 72 (36.5) | ||
| Nodes | 109 (64.5) | 17.6 | |
| Metastasis | 67 (36.2) | 9.8 | |
| Time since diagnosis | Days | 39.08 ± 35.1 | 9.8 |
| 2. Caregivers | |||
| Age | Years | 55,6 ± 14,4 | 22.4 |
| Relationship with the patient | Partner | 125 (61.0) | 0 |
| Children | 44 (21.5) | ||
| Brother/sister | 12 (5.9) | ||
| Parent | 6 (2.9) | ||
| Othersa | 18 (8.8) | ||
| Gender | Woman | 146 (71.2) | 0 |
| Man | 59 (28.8) | ||
| Educational level | <12 years | 79 (48.8) | 21.0 |
| > = 12 years | 83 (51.2) | ||
| Marital status | Single | 30 (15.8) | 7.3 |
| Couple | 160 (84.2) | ||
| Professional status | Worker | 31 (16.4) | 7.8 |
| Not worker | 158 (83.6) | ||
afriend, other member of the family, previous partner, other cases
N (%): effective (percents); M ± SD: mean ± standard deviation; MD: missing data
SEIQoL domains freely expressed by patients and caregivers
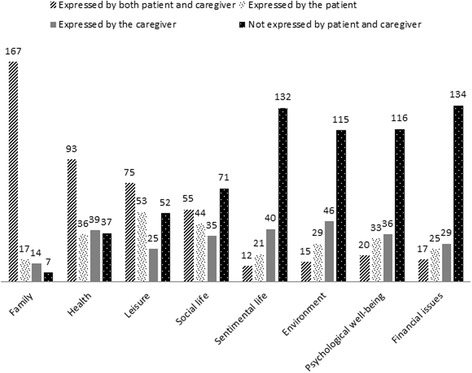
The first five most frequent QoL domains expressed by the patients were strictly identical to the first five most frequent QoL domains expressed by the caregivers. Among these five domains, the Family domain was the most expressed QoL domain (expressed by 90% of the patients and 88% of the caregivers). For the 167 dyads for which the family domain was expressed both by the patient and the caregiver, while the attributed weight to the family domain did not differ between the patients and the caregivers, the family score was significantly lower for caregivers than for the patients. Health, Leisures, and Social life were the 3 most expressed QoL domains by the patients and the caregivers, in the second, third, and fourth positions, respectively. For dyads for which Health and Leisure domains were common expressed domains by the patient and the caregiver, the scores did not differ between the patients and the caregivers. However, the weight of the importance given to these respective domains differed: the weight of Health domain was significantly higher for the caregivers than for the patients, and the weight of Leisure score was significantly higher for the patients than for the caregivers. The Occupational issues domain was the fifth domain expressed by the patients and the caregivers, but was most frequently expressed by the caregivers (for 34% of caregivers compared to 27% of patients). Within the dyads including patients and caregivers mentioning the Occupational issues domain, the QoL score was significantly better for the caregivers than for the patients but the weight assigned to the domain was not different between the two members of the dyad.
The caregivers (25%) most frequently mentioned the Love life domain compared to the patients (16%). The 2 members of a same dyad were quite consistent for the following domains: 81% of the dyads, patient and caregiver simultaneously expressed Family, while Love life and Financial issues were not expressed by two thirds of the patient-caregiver dyads, and Environment and Psychological well-being were not expressed by 56% of the patient-caregiver dyads. The index did not differ between patients and caregivers within the same dyad.
The details of the range, the score, and the attributed weight to each of each expressed domains by patients and caregivers are provided in Table 2. For dyads with patient and caregiver expressing common domains, the differences between scores and attributed weight to each domains expressed are detailed in Table 3. Figure 1 illustrates each expressed domains, considering that the domain has been mentioned according to: a) the 2 members of the dyad, b) only the patient within the dyad, c) only the caregiver within the dyad, and d) neither the patient nor the caregiver within the dyad.
Table 2.
Ranges, scores, and attributed weights of expressed SEIQoL domains by patients and caregivers
| N | Range | Scorea | Weighb | |||||
|---|---|---|---|---|---|---|---|---|
| Patients | Caregivers | Patients | Caregivers | Patients | Caregivers | Patients | Caregivers | |
| Domains | N = 205 | N = 205 | N = 205 | N = 205 | N = 205 | N = 205 | N = 205 | N = 205 |
| N (%) | N (%) | 1–10 | 1–10 | (0–100) | (0–100) | (0–100) | (0–100) | |
| Family | 184 | 181 | 1 | 1 | 87,17 ± 17,65 | 81,64 ± 19,21 | 40,74 ± 18,19 | 40,74 ± 20,91 |
| Health | 129 | 132 | 2 | 2 | 55,96 ± 25,57 | 56,17 ± 25,67 | 34,57 ± 16,28 | 37,16 ± 19,43 |
| Leisures | 128 | 100 | 3 | 3 | 51,41 ± 32,64 | 58,47 ± 28,21 | 16,24 ± 12,27 | 14,65 ± 11,43 |
| Social life | 99 | 90 | 4 | 4 | 82,74 ± 17,92 | 76,96 ± 23,00 | 17,71 ± 9,84 | 17,73 ± 12,09 |
| Occupational issues | 55 | 70 | 5 | 5 | 53,56 ± 32,19 | 75,42 ± 23,04 | 14,44 ± 10,42 | 15,53 ± 9,49 |
| Psychological well-being | 53 | 56 | 6 | 7 | 70,63 ± 23,27 | 69,37 ± 28,93 | 19,81 ± 13,18 | 16,98 ± 12,60 |
| Environment | 44 | 61 | 7 | 6 | 64,72 ± 29,98 | 70,31 ± 26,05 | 15,3 ± 14,26 | 11,90 ± 7,14 |
| Financial issues | 42 | 46 | 8 | 9 | 51,35 ± 24,48 | 62,02 ± 23,89 | 12,17 ± 6,61 | 10,43 ± 8,67 |
| Love life | 33 | 52 | 9 | 8 | 80,27 ± 28,60 | 71,71 ± 24,77 | 31,97 ± 14,24 | 28,65 ± 17,93 |
| Autonomy | 21 | 7 | 10 | 10 | 52,41 ± 28,51 | 61,42 ± 21,15 | 21 ± 13,13 | 13,29 ± 8,56 |
afrom 0 (lower) to 100 (higher) level of quality of life
bfrom 0 (lower) to 100 (higher) weight assigned to the specific domain
M ± SD: mean ± standard deviation
Table 3.
Common domains expressed by both patient and caregiver within the dyad
| Domains | N | Scores’ differencea | p | Weighs’ difference b | p |
|---|---|---|---|---|---|
| Family | 167 | 4.81 | 0.002 | 0.33 | 0.918 |
| Health | 93 | 1.6 | 0.660 | 4.86 | 0.030 |
| Leisures | 75 | 5.9 | 0.099 | 3.34 | 0.042 |
| Social life | 55 | 0.59 | 0.939 | 0.80 | 0.730 |
| Occupational issues | 25 | 19.71 | 0.030 | 4.50 | 0.317 |
| Psychological well-being | 20 | 7.96 | 0.421 | 7.05 | 0.039 |
| Environment | 15 | 6.32 | 0.555 | 4.40 | 0.486 |
| Financial issues | 17 | 5.11 | 0.793 | 1.06 | 0.594 |
| Love life | 12 | 14.5 | 0.176 | 1.00 | 0.929 |
| Autonomy | 2 | - | - | - | |
| Index | 205 | 1.72 | 0.424 |
ascores’ difference between the patient’ score and the caregiver’ score within a same dyad (absolute value)
bweights’ difference between the patient’ weight and the caregiver’ weight within a same dyad (absolute value)
Bold values: p < 0.05
Fig. 1.
Proportions of expressed SEIQoL domains by the patient-caregiver dyads
Relations between SEIQoL and dimensions scores of standardized QoL questionnaires
Condition-specific QoL questionnaires: EORTC QLQ-C30 and CarGOQoL
For patients, the SEIQoL index was significantly correlated with all the functioning scores of EORTC QLQ-C30 (R from 0.15 to 0.27), except the physical functioning score, and with only 3 of 9 symptom scores (R from -0.18 to -0.23): fatigue, nausea, and pain. The SEIQoL index score significantly correlated with 5 of the 10 dimension scores (psychological well-being, burden, finances, physical well-being, and private life, R from 0.18 to 0.31) and the index of CarGOQoL (R = 0.40). All the details are provided in Table 4.
Table 4.
Correlations between SEIQoL index and dimensions scores of standardized QoL questionnaires
| Patients’ SEIQoL indexa | Caregivers’ SEIQoL indexa | ||||
|---|---|---|---|---|---|
| Patient’QoL | R | p | Caregiver’s QoL | R | p |
| SF-36 (generic) | SF-36 (generic) | ||||
| Physical Functioninga | 0.074 | 0.314 | Physical Functioninga | 0.172 | 0.028 |
| Social Functioninga | 0.257 | <0.001 | Social Functioninga | 0.305 | <0.001 |
| Role Limitation physicala | 0.143 | 0.051 | Role Limitation physicala | 0.244 | 0.002 |
| Role Limitation emotionala | 0.075 | 0.322 | Role Limitation emotionala | 0.253 | 0.001 |
| Mental Healtha | 0.242 | 0.001 | Mental Healtha | 0.242 | 0.002 |
| Vitalitya | 0.26 | <0.001 | Vitalitya | 0.273 | <0.001 |
| Bodily Paina | 0.136 | 0.062 | Bodily Paina | 0.234 | 0.003 |
| General Healtha | 0.257 | <0.001 | General Healtha | 0.254 | 0.001 |
| PCSa | 0.079 | 0.304 | PCSa | 0.158 | 0.052 |
| MCSa | 0.245 | 0.001 | MCSa | 0.258 | 0.001 |
| QLQ-C30 (specific) | CARGOQOL (specific) | ||||
| Global healtha | 0.27 | <0.001 | Psychological well-beinga | 0.262 | 0.001 |
| Physical Functioninga | 0.131 | 0.076 | Burdena | 0.313 | <0.001 |
| Role Functioninga | 0.248 | 0.001 | Relationship with health carea | 0.127 | 0.118 |
| Emotional Functioninga | 0.266 | <0.001 | Administration and financesa | 0.182 | 0.023 |
| Cognitive Functioninga | 0.152 | 0.041 | Copinga | 0.105 | 0.188 |
| Social Functioninga | 0.184 | 0.013 | Physical well-beinga | 0.24 | 0.002 |
| Fatigueb | -0.232 | 0.002 | Self-esteema | 0.053 | 0.51 |
| Nauseab | -0.209 | 0.005 | Leisures Timea | 0.132 | 0.096 |
| Painb | -0.175 | 0.019 | Social Supporta | 0.094 | 0.242 |
| Dyspnoeab | -0.135 | 0.071 | Private lifea | 0.237 | 0.004 |
| Insomniab | -0.144 | 0.057 | Index CarGOQoLa | 0.402 | <0.001 |
| Appetiteb | -0.146 | 0.051 | |||
| Constipationb | -0.062 | 0.402 | |||
| Diarrhoeab | -0.045 | 0.560 | |||
| Financial difficultiesb | 0.021 | 0.781 | |||
R Spearman correlation coefficient (values between +1 and -1; the sign (+/-) of the correlation coefficient indicates the direction of the correlation) [32]
ahigher score, higher QoL level
**higher score, lower QoL level
Bold values: p < 0.05
Generic health-related QoL questionnaire: SF-36
For caregivers, the SEIQoL index was positively but moderately correlated with the mental composite score and 8 dimension scores of the generic QoL questionnaire, the SF-36. The range of significant correlation coefficients was 0.17 to 0.31. For patients, the SEIQoL index significantly correlated with the mental composite score and 4 dimensions score, including social- and mental-like dimensions of SF-36 (social functioning, mental health, vitality, and general health). The coefficients ranged from 0.24 to 0.26. All the details are provided in Table 4.
Discussion
The quality of life of cancer patients and their caregivers, assessed with QoL standardized questionnaires, has been extensively described in the literature. However, to our knowledge, the present study is the first to simultaneously assess the QoL of a large sample of cancer patients and their caregivers using an individualized approach based on the use of the SEIQoL questionnaire. Despite the individual approach d when describing the SEIQoL-DW, most published reports present results based on the quantitative parts of the instrument. The present study provided, for the first time, QoL domains spontaneously expressed by both cancer patients and their caregivers.
The first interesting finding is individualized measures were moderately correlated with other standardized QoL measures, highlighting that generic, specific and individualized instruments may explore different facets of the self-perceived quality of life [2, 3, 7, 23]. One explanation may be that these instruments may reflect the different conceptual bases of these measures. Unlike traditional QoL instruments, often focusing on QoL limitations inflicted by disease or treatment, SEIQoL may reflect the capacity of a patient to appreciate and value important areas in life, despite health problems. The standardized instruments not only measure pre-defined domains, but also focus more on the symptoms and disease and less on overall QoL of life issues and even positive life aspects. Previous authors have defined the SEIQoL as a person-centered measure, not a health-based measure [24]; spontaneously defining their personal cues and pondering personal priorities should help the individual to clear his/her concept of QoL and provide a rating in a realistic and valid manner [7]. Some limitations of the SEIQoL have previously been described; these include the arbitrary aspect of the nomination of the cues (raw cues grouped in aggregated cues by experts [25]; the multiple administration modalities (individual semi-structured face to face interviews, group settings, telephone interviews, self-administration, computer version…), which may compromise the direct comparability between studies and the heterogeneity of weighting procedure [3]. Thus, this measure should provide an interesting picture in which the individuals take ownership of the QoL concept.
The second interesting finding of this study is that the nature and the frequency of domains spontaneously expressed by a sample of cancer patient was similar to the domains spontaneous expressed by their caregivers. Family was the most frequently expressed domain by both cancer patients and their caregivers, with patients slightly weighing more importance than their caregivers. Family, followed by health and leisure, appears as a common base for various populations that exactly mentioned them in the same sequence: amyotrophic lateral sclerosis patients [25], multiple sclerosis patients [12], cardiac patients [26], or patients undergoing stem cell transplantation [7], or patients with other type of cancer [27]. Among the top 5 domains, the social dimension was the most represented dimension, including family relations, leisure aspect, social life, and even occupational issues. Patients reported lower QoL levels for occupational and financial issues than the caregivers; it is now well-documented that a high proportion of cancer patients become unemployed during the course of the disease (either by job loss or quitting work) resulting to a more difficult financial situation [28]. Autonomy and psychological well-being were less mentioned as independent domain, partially reflecting that the use of the general term of health includes these notions. Other domains were not mentioned, such as spirituality, or less often mentioned, such as financial issues or love life. Some assumptions may be stated. First, these domains strongly depend on socio-cultural and economic context [29]. Second, it is likely that patients and caregivers assume with more difficulties to spontaneously mention these aspects of their life as secondary compared with noble domains, such as ‘family’. Thus, predetermined questionnaires may capture aspects considered as important by the individuals in their daily life but treated with less priority than the disease and treatment importance. Because patients were early in the course of their cancers, future research will benefit from a new focus on the interactions between patients and their relatives later in the course of disease.
The clinical utility of the QoL assessment implementation in clinical practice using this type of measure should be discussed. Individualized measures allow capturing various aspects of QoL, taking into account the uniqueness of the human experience [2, 30]. Wettergren and colleagues recommended the use of these measures in clinical practice to take advantage of the patient’s resources (for example, coping strategies, response shift, and resilience) and act on the problems of greatest importance to the patient. The communication between individuals and therapists should be improved and care could focus on strengthening the patient’s resources and addressing perceived obstacles [31].
Conclusion
The presents study highlighted additional elements confirming the need to explore QoL using a combination of various questionnaires, associating individualized questionnaires and standardized (generic and/or) questionnaires. Individualized measures enabled individuals to spontaneously express important and non-predefined domains and standardized questionnaires facilitated the expression of self-perception on domains considered secondary.
Acknowledgments
The authors thank Claire Morando and Margot Auquier for their logistic support. The authors are grateful to all the subjects for their participation in the study.
Funding
This work has been financially supported by Merck Serono. This work was supported by the National Clinical Research Quality of Life in Oncology Platform labelled by the National Cancer Ligue and the French National Cancer Institute (Grant INCa-DGOS-Inserm 6038). These sponsors had no role in study design; collection, analysis and interpretation of data; writing of the report; decision to submit the article for publication.
Availability of data and materials
Data are unsuitable for public deposition due to ethical and legal restrictions and are therefore available upon request with the signature of a data privacy form. To request the data, the readers may contact Karine Baumstarck (karine.baumstarck@univ-amu.fr).
Authors’ contributions
Conception and design: PA. Study coordination: PA. Acquisition of data: OC, FB, SS, TL. Analysis of data: ZH. Interpretation of data: ZH, KB, TL. Drafting and writing of manuscript: ZH, KB. Revision and approval of final version of the manuscript: ZH, KB, OC, FB, SS, TL, PA.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable (the manuscript does not contain any individual persons data).
Ethics approval and consent to participate
Regulatory monitoring was performed in accordance with the French law that requires approval of the French ethics committee (Comité d’éthique, Aix Marseille University, October 8th 2015, Number 2014-09-30-05). Written consent forms for participation were collected from each patient and caregiver.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- CarGOQoL
CareGiver oncology quality of Life questionnaire
- EORTC
European organization for research and treatment of cancer
- QoL
Quality of life
- SEIQoL
Schedule for the evaluation of individual QoL
- SEIQoL-DW
Schedule for the evaluation of individual QoL - direct weighting
- SF-36
Short form 36
- SF36-MCS
SF36 Mental composite score
- SF36-PCS
SF36 Physical composite score
Contributor Information
Zeinab Hamidou, Email: zeinab.hamidou@univ-amu.fr.
Karine Baumstarck, Phone: +33 491 384 744, Email: karine.baumstarck@univ-amu.fr.
Olivier Chinot, Email: olivier.chinot@ap-hm.fr.
Fabrice Barlesi, Email: fabrice.barlesi@ap-hm.fr.
Sébastien Salas, Email: sebastien.salas@ap-hm.fr.
Tanguy Leroy, Email: tanguy.leroy@univ-lyon2.fr.
Pascal Auquier, Email: pascal.auquier@univ-amu.fr.
References
- 1.Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ. 2002;324:1417. doi: 10.1136/bmj.324.7351.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waldron D, O’Boyle CA, Kearney M, Moriarty M, Carney D. Quality-of-life measurement in advanced cancer: assessing the individual. J Clin Oncol. 1999;17:3603–3611. doi: 10.1200/JCO.1999.17.11.3603. [DOI] [PubMed] [Google Scholar]
- 3.Wettergren L, Kettis-Lindblad A, Sprangers M, Ring L. The use, feasibility and psychometric properties of an individualised quality-of-life instrument: a systematic review of the SEIQoL-DW. Qual Life Res. 2009;18:737–746. doi: 10.1007/s11136-009-9490-2. [DOI] [PubMed] [Google Scholar]
- 4.McGee HM, O’Boyle CA, Hickey A, O’Malley K, Joyce CR. Assessing the quality of life of the individual: the SEIQoL with a healthy and a gastroenterology unit population. Psychol Med. 1991;21:749–759. doi: 10.1017/S0033291700022388. [DOI] [PubMed] [Google Scholar]
- 5.O’Boyle CA, McGee HM, Hickey A, Joyce CRB, Browne J, O’Malley K. The Schedule for the Evaluation of Individual Quality of Life (SEIQoL): Administration manual. Dublin: Royal College of Surgeons in Ireland; 1993.
- 6.Hickey AM, Bury G, O’Boyle CA, Bradley F, O’Kelly FD, Shannon W. A new short form individual quality of life measure (SEIQoL-DW): application in a cohort of individuals with HIV/AIDS. BMJ. 1996;313:29–33. doi: 10.1136/bmj.313.7048.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frick E, Borasio GD, Zehentner H, Fischer N, Bumeder I. Individual quality of life of patients undergoing autologous peripheral blood stem cell transplantation. Psychooncology. 2004;13:116–124. doi: 10.1002/pon.730. [DOI] [PubMed] [Google Scholar]
- 8.Moons P, Marquet K, Budts W, De Geest S. Validity, reliability and responsiveness of the “schedule for the evaluation of individual quality of life-direct weighting” (SEIQoL-DW) in congenital heart disease. Health Qual Life Outcomes. 2004;2:27. doi: 10.1186/1477-7525-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LeVasseur SA, Green S, Talman P. The SEIQoL-DW is a valid method for measuring individual quality of life in stroke survivors attending a secondary prevention clinic. Qual Life Res. 2005;14:779–788. doi: 10.1007/s11136-004-0795-x. [DOI] [PubMed] [Google Scholar]
- 10.Kettis-Lindblad A, Ring L, Widmark E, Bendtsen P, Glimelius B. Patients‘and doctors’ views of using the schedule for individual quality of life in clinical practice. J Support Oncol. 2007;5:281–287. [PubMed] [Google Scholar]
- 11.O’Boyle CA, McGee H, Hickey A, O’Malley K, Joyce CR. Individual quality of life in patients undergoing hip replacement. Lancet. 1992;339:1088–1091. doi: 10.1016/0140-6736(92)90673-Q. [DOI] [PubMed] [Google Scholar]
- 12.Mattarozzi K, Casini F, Baldin E, Baldini M, Lugaresi A, Milani P, Pietrolongo E, Gajofatto A, Leone M, Riise T, et al. Assessing subjective quality of life domains after multiple sclerosis diagnosis disclosure. Health Expect. 2016;19:437–447. doi: 10.1111/hex.12367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Felgoise SH, Stewart JL, Bremer BA, Walsh SM, Bromberg MB, Simmons Z. The SEIQoL-DW for assessing quality of life in ALS: strengths and limitations. Amyotroph Lateral Scler. 2009;10:456–462. doi: 10.3109/17482960802444840. [DOI] [PubMed] [Google Scholar]
- 14.Valle A, Gallo G, Oliver D, Veronese S, Rivoiro C. Specialist palliative care service for people severely affected by neurodegenerative conditions: does this make a difference to palliative care outcom. Ann Univ Alba Iuli. 2010;2:539–548. [Google Scholar]
- 15.Solari A, Giordano A, Grasso MG, Confalonieri P, Patti F, Lugaresi A, Palmisano L, Amadeo R, Martino G, Ponzio M, et al. Home-based palliative approach for people with severe multiple sclerosis and their carers: study protocol for a randomized controlled trial. Trials. 2015;16:184. doi: 10.1186/s13063-015-0695-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scholzel-Dorenbos CJ, Draskovic I, Vernooij-Dassen MJ, Olde Rikkert MG. Quality of life and burden of spouses of Alzheimer disease patients. Alzheimer Dis Assoc Disord. 2009;23:171–177. doi: 10.1097/WAD.0b013e318190a260. [DOI] [PubMed] [Google Scholar]
- 17.Khanjari S, Langius-Eklof A, Oskouie F, Sundberg K. Family caregivers of women with breast cancer in Iran report high psychological impact six months after diagnosis. Eur J Oncol Nurs. 2014;18:630–635. doi: 10.1016/j.ejon.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Bromberg MB, Forshew DA. Comparison of instruments addressing quality of life in patients with ALS and their caregivers. Neurology. 2002;58:320–322. doi: 10.1212/WNL.58.2.320. [DOI] [PubMed] [Google Scholar]
- 19.Lo Coco G, Lo Coco D, Cicero V, Oliveri A, Lo Verso G, Piccoli F, La Bella V. Individual and health-related quality of life assessment in amyotrophic lateral sclerosis patients and their caregivers. J Neurol Sci. 2005;238:11–17. doi: 10.1016/j.jns.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 21.Minaya P, Baumstarck K, Berbis J, Goncalves A, Barlesi F, Michel G, Salas S, Chinot O, Grob JJ, Seitz JF, et al. The CareGiver oncology quality of life questionnaire (CarGOQoL): development and validation of an instrument to measure the quality of life of the caregivers of patients with cancer. Eur J Cancer. 2012;48:904–911. doi: 10.1016/j.ejca.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Leplege A, Ecosse E, Verdier A, Perneger TV. The French SF-36 health survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol. 1998;51:1013–1023. doi: 10.1016/S0895-4356(98)00093-6. [DOI] [PubMed] [Google Scholar]
- 23.Becker G, Merk CS, Meffert C, Momm F. Measuring individual quality of life in patients receiving radiation therapy: the SEIQoL-questionnaire. Qual Life Res. 2014;23:2025–2030. doi: 10.1007/s11136-014-0661-4. [DOI] [PubMed] [Google Scholar]
- 24.Lintern TC, Beaumont JG, Kenealy PM, Murrell RC. Quality of Life (QoL) in severely disabled multiple sclerosis patients: comparison of three QoL measures using multidimensional scaling. Qual Life Res. 2001;10:371–378. doi: 10.1023/A:1012219504134. [DOI] [PubMed] [Google Scholar]
- 25.Neudert C, Wasner M, Borasio GD. Patients’ assessment of quality of life instruments: a randomised study of SIP, SF-36 and SEIQoL-DW in patients with amyotrophic lateral sclerosis. J Neurol Sci. 2001;191:103–109. doi: 10.1016/S0022-510X(01)00612-8. [DOI] [PubMed] [Google Scholar]
- 26.Smith HJ, Taylor R, Mitchell A. A comparison of four quality of life instruments in cardiac patients: SF-36, QLI, QLMI, and SEIQoL. Heart. 2000;84:390–394. doi: 10.1136/heart.84.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stone PC, Murphy RF, Matar HE, Almerie MQ. Measuring the individual quality of life of patients with prostate cancer. Prostate Cancer Prostatic Dis. 2008;11:390–396. doi: 10.1038/pcan.2008.16. [DOI] [PubMed] [Google Scholar]
- 28.Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77:109–130. doi: 10.1016/j.critrevonc.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Caqueo-Urizar A, Urzua A, Boyer L, Williams DR. Religion involvement and quality of life in patients with schizophrenia in Latin America. Soc Psychiatry Psychiatr Epidemiol. 2016;51:521–528. doi: 10.1007/s00127-015-1156-5. [DOI] [PubMed] [Google Scholar]
- 30.Wettergren L, Hedlund Lindberg M, Kettis A, Glimelius B, Ring L. Comparison of two instruments for measurement of quality of life in clinical practice--a qualitative study. BMC Med Res Methodol. 2014;14:115. doi: 10.1186/1471-2288-14-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Locke DE, Cerhan JH, Wu W, Malec JF, Clark MM, Rummans TA, Brown PD. Cognitive rehabilitation and problem-solving to improve quality of life of patients with primary brain tumors: a pilot study. J Support Oncol. 2008;6:383–391. [PubMed] [Google Scholar]
- 32.Cohen, J. Statistical power analysis for the behavioral sciences (2nd ed.) New Jersey: Lawrence Erlbaum; 1988 p. 400.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are unsuitable for public deposition due to ethical and legal restrictions and are therefore available upon request with the signature of a data privacy form. To request the data, the readers may contact Karine Baumstarck (karine.baumstarck@univ-amu.fr).


