Dear Editor,
Primary seminal vesicle tumors are rare and mostly reported cases were malignant. Benign primary tumors including cystadenomas are even rarer than malignant neoplasms.1,2 Herein, we report a 71-year-old man with cystadenoma of the seminal vesicle. The clinical presentation, computed tomography (CT), and magnetic resonance imaging (MRI) findings, gross appearance, microscopic features, and immunohistochemical characteristics of this uncommon tumor are described.
A 71-year-old man asymptomatic man was transferred to our hospital for evaluation of a pelvic mass which was revealed incidentally by ultrasonography (US). Five years earlier, artificial femoral head replacement was operated. A digital rectal examination detected a painless mass anterior to the rectum. A pelvic CT scan and MRI confirmed a 5.5 cm × 6.0 cm × 5.3 cm sized oval, soft tissue density, or signal intensity mass located between the bladder and rectum (Figures 1 and 2). A CT-guided fine-needle aspiration biopsy was performed. The cytological examination did not find malignant neoplastic cells.
Figure 1.
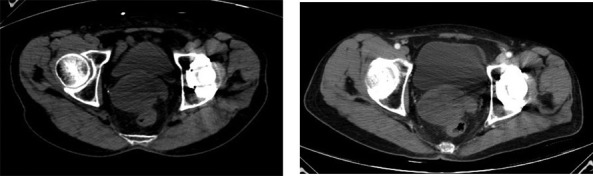
Pelvic CT scan shows a 5.5 cm × 6.0 cm × 5.3 cm sized oval, soft tissue density mass between the bladder and rectum. Unenhanced (a) and contrast-enhanced (b) CT scan show CT value of the tumor is about 10.5 HU and 24.1 HU, respectively CT: computed tomography.
Figure 2.
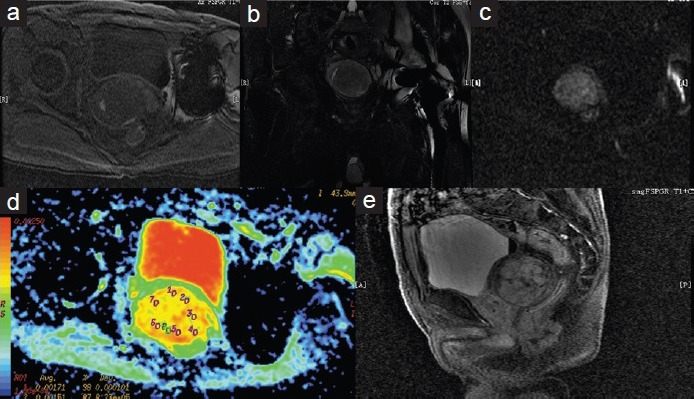
On cross section T1-weighted image (a), the tumor is mixed hypointense and hyperintense. On coronal T2-weighted (b) shows mixed hperintense signal tumor with hypointense capsule. On cross section, DW image (c) shows pale hyperintense signal. On cross section ADC image (d) shows the ADC is about 1.68 × 10−3 mm2 s−1. Contrast-enhanced MRI scan (e) shows prolonged and delayed enhancement pattern with tumor capsule. DW: diffusion-weighted; ADC: apparent diffusion coefficient; MRI: magnetic resonance imaging.
The patient was explored through a midline abdominal incision under general anesthesia. The tumor was completely dissected from attachments to the baldder and prostate anteriorly, rectum posteriorly and the right seminal vesicle. The tumor was covered by a complete gray capsule, and multiple cavities were seen, fulfilled with a clear liquid through the external surface (Figure 3). Histological features of the surgical specimen were compatible with cystadenoma of the seminal vesicle (Figure 4). Immunohistochemical staining showed that carcinoembryonic antigen (CEA), prostate-specific antigen (PSA), cytokeratin (CK), cytokertatin 20 (CK 20), and villin stains gave negative results. The glandular cells showed positivity for CA125 (Figure 5).
Figure 3.
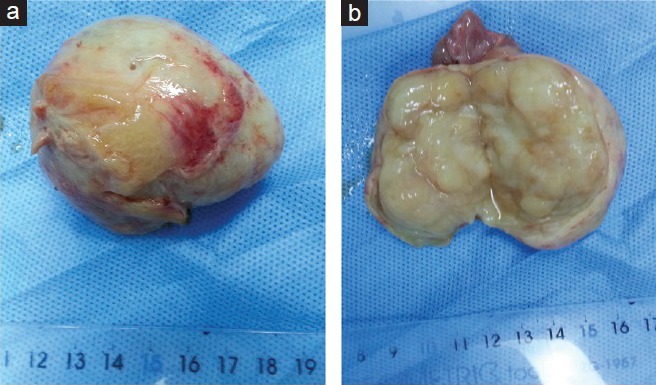
Grossly, the mass consisted of a well-circumscribed, oval contour. Its external surface is smooth, glistening (a). The cut surface showed multilocular cysts (b).
Figure 4.
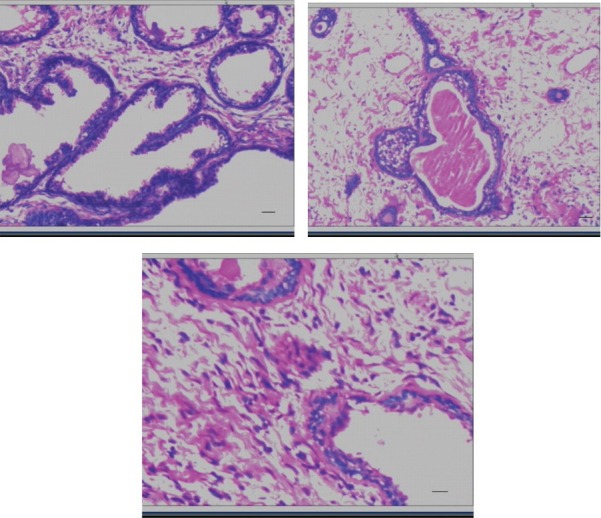
Microscopy: The tumor contains innumerable glands and cysts of varying sizes and shapes filled with pale eosinophilic intraluminal secretions and lined by one to two layers of cuboidal or low columnar cells. Scale bar = 100 μm (a and b). The stromal cells are spindle-shaped and arranged in fascicles between the glands. Scale bar = 200 μm (c).
Figure 5.
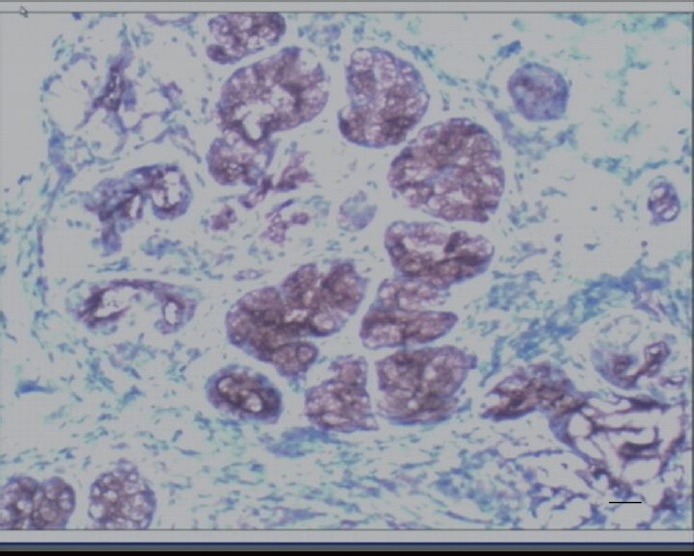
The glandular cells showed positivity for CA125. Scale bar = 100 μm.
The patient postoperative recovery was uneventful and was discharged 9 days after surgery with instructions of outpatient follow-up. Eighteen months after surgery, the patient is still alive with no recurrence of this disease but was revealed lung cancer by chest CT.
Tumors of the seminal vesicles which may be secondary spread from adjacent organs such as the bladder, prostate, rectum, or lymphoma are relatively common.2,3 The unusual sites are more frequently involved by metastatic tumors. The reported examples of primary malignant tumors are adenocarcinomas, pure sarcomas, or cystosarcoma. Benign primary tumors such as cystadenoma are even rarer than these malignant neoplasms.2 Primary seminal vesicle cystadenoma is an extremely rare benign tumor originating from the embryological residues of the Mullerian ducts.4
The clinical features in all patients with seminal vesicle cystadenoma included being asymptomatic, abdominal pain, hematuria, hemospermia, and lower urinary tract symptoms.5,6 The wide variety of presenting features may result from variations in the size and location of the mass. In our case, it was asymptomatic and detected incidentally by the US.
CT and MRI provided useful information in determining both the extent of the lesion and its invasiveness. In our case, CT demonstrated a homogenous soft tissue density mass. MRI showed an inhomogeneous mass because of high resolution in soft tissue. The outline was clear with well-defined capsule. The contiguous anatomical structures were compressed with no signs of infiltration. This suggested a benign lesion.4 When imaging findings are nonspecific, the US or CT-guided biopsy is crucial. Regardless, biopsies may be inconclusive, and exploratory laparotomy or laparoscopy is usually needed.1,4
Macroscopically, the tumors were well circumscribed and surrounded by a membraneous capsule. The histological finding in these cases demonstrated tumors composed of glands and cysts lined predominantly by cuboidal and columnar epithelium surrounded by fibrous stroma.2,7 Reikie et al.8 proposed that term seminal vesicle “mixed epithelial-stromal tumor” was used to designate the tumors of the seminal vesicle containing epithelial and stromal components, with a distinction of the grade based on the histologic features and the biological behavior. According to their criterion, our case may be designated “low-grade mixed epithelial-stromal tumor.”
Immunohistochemical analysis using PSA, CEA, and villin may be done to exclude prostatic and colon origin.2,7,9
Occasional tumor recurrences may occur when these tumors are incompletely excised.10,11 In this case, it is advisable to remove the whole tumor involving seminal vesicle, even if it is asymptomatic.
AUTHOR CONTRIBUTIONS
XPK participated in drafting the manuscript. QGD participated in the paper's discussion. SYW supervised the study design and coordination. PFW and JMQ helped to collect the clinical data. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing financial interests.
REFERENCES
- 1.Gil AO, Yamakami LY, Genzini T. Cystadenoma of the seminal vesicle. Int Braz J Urol. 2003;29:434–6. doi: 10.1590/s1677-55382003000500009. [DOI] [PubMed] [Google Scholar]
- 2.Lee CB, Choi HJ, Cho DH, Ha US. Cystadenoma of the seminal vesicle. Int J urol. 2006;13:1138–40. doi: 10.1111/j.1442-2042.2006.01511.x. [DOI] [PubMed] [Google Scholar]
- 3.Lorber G, Pizov G, Gofrit ON, Pode D. Seminal vesicle cystadenoma: a rare clinical perspective. Eur Urol. 2011;60:388–91. doi: 10.1016/j.eururo.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Lagalla R, Zappasodi F, Lo Casto A, Zenico T. Cystadenoma of the seminal vesicle: US and CT findings. Abdom Imaging. 1993;18:298–300. doi: 10.1007/BF00198130. [DOI] [PubMed] [Google Scholar]
- 5.Arora A, Sharma S, Seth A. Unusual retrovesical cytic mass in a male patient. Urology. 2013;81:e23–4. doi: 10.1016/j.urology.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Zhu JG, Chen WH, Xu SX, Wang RP, Sun ZL. Cystadenoma in a seminal vesicle is cured by laparoscopic ablation. Asian J Androl. 2013;15:697–8. doi: 10.1038/aja.2013.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santos LD, Wong CS, Killingsworth M. Cystadenoma of the seminal vesicle: report of a case with ultrastructural findings. Pathology. 2001;33:399–402. [PubMed] [Google Scholar]
- 8.Reikie BA, Yilmaz A, Medlicott S, Trpkov K. Mixed epithelial-stromal tumor (MEST) of seminal vesicle: a proposal for unified nomenclature. Adv Anat Pathol. 2015;22:113–20. doi: 10.1097/PAP.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 9.Seong BM, Cheon J, Lee JG, Kim JJ, Chae YS. A case of multilocular prostatic cystadenoma. J Korean Med Sci. 1998;13:554–8. doi: 10.3346/jkms.1998.13.5.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazur MT, Myers JL, Maddox WA. Cystic epithelial-stromal tumor of the seminal vesicle. Am J Surg Pathol. 1987;11:210–7. doi: 10.1097/00000478-198703000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Bullock KN. Cystadenoma of the seminal vesicle. J R Soc Med. 1988;81:294–5. doi: 10.1177/014107688808100520. [DOI] [PMC free article] [PubMed] [Google Scholar]


