Supplemental Digital Content is available in the text.
Abstract
INTRODUCTION:
Noise in health care settings has increased since 1960 and represents a significant source of dissatisfaction among staff and patients and risk to patient safety. Operating rooms (ORs) in which effective communication is crucial are particularly noisy. Speech intelligibility is impacted by noise, room architecture, and acoustics. For example, sound reverberation time (RT60) increases with room size, which can negatively impact intelligibility, while room objects are hypothesized to have the opposite effect. We explored these relationships by investigating room construction and acoustics of the surgical suites at our institution.
METHODS:
We studied our ORs during times of nonuse. Room dimensions were measured to calculate room volumes (VR). Room content was assessed by estimating size and assigning items into 5 volume categories to arrive at an adjusted room content volume (VC) metric. Psychoacoustic analyses were performed by playing sweep tones from a speaker and recording the impulse responses (ie, resulting sound fields) from 3 locations in each room. The recordings were used to calculate 6 psychoacoustic indices of intelligibility. Multiple linear regression was performed using VR and VC as predictor variables and each intelligibility index as an outcome variable.
RESULTS:
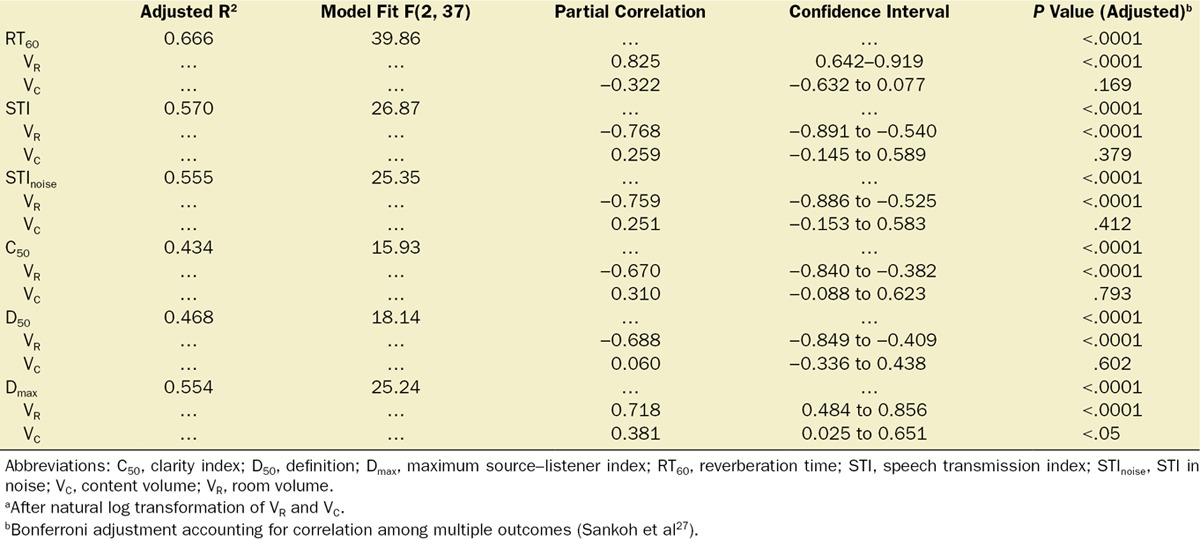
A total of 40 ORs were studied. The surgical suites were characterized by a large degree of construction and surface finish heterogeneity and varied in size from 71.2 to 196.4 m3 (average VR = 131.1 [34.2] m3). An insignificant correlation was observed between VR and VC (Pearson correlation = 0.223, P = .166). Multiple linear regression model fits and β coefficients for VR were highly significant for each of the intelligibility indices and were best for RT60 (R2 = 0.666, F(2, 37) = 39.9, P < .0001). For Dmax (maximum distance where there is <15% loss of consonant articulation), both VR and VC β coefficients were significant. For RT60 and Dmax, after controlling for VC, partial correlations were 0.825 (P < .0001) and 0.718 (P < .0001), respectively, while after controlling for VR, partial correlations were −0.322 (P = .169) and 0.381 (P < .05), respectively.
CONCLUSIONS:
Our results suggest that the size and contents of an OR can predict a range of psychoacoustic indices of speech intelligibility. Specifically, increasing OR size correlated with worse speech intelligibility, while increasing amounts of OR contents correlated with improved speech intelligibility. This study provides valuable descriptive data and a predictive method for identifying existing ORs that may benefit from acoustic modifiers (eg, sound absorption panels). Additionally, it suggests that room dimensions and projected clinical use should be considered during the design phase of OR suites to optimize acoustic performance.
Noise levels in health care settings have steadily increased since 1960,1 and noise is currently a significant source of dissatisfaction among hospital staff and patients.2,3 Sound sources such as beepers, alarms, and conversational speech disrupt patient sleep cycles3–7 and induce physiological effects in critically ill patients,8 and they have also been associated with increased infection rate.9–11 Effects of noise on staff include increased stress,12–14 which may impact performance and increase risk of committing medical error.15 Collectively, many studies indicate that noise, also referred to as the “third pollution” after air and water pollution, likely has a detrimental impact on both caregiver health and patient safety. Operating rooms (ORs), environments in which effective communication and signaling of alarms are integral to patient care, are particularly noisy.16 Data have been published that characterize the excessive sound levels present during surgeries—especially in orthopedic and neurological procedures.17,18 Recently, an intervention program that used behavioral modification and a feedback-providing noise device was able to decrease sound levels in a pediatric surgical suite. The decreased sound levels were associated with fewer postoperative surgical complications.19 As part of the intervention, landline phone ringers were muted, cell phones and any personal conversations were banned during procedures, medical and equipment alarm volumes were decreased, and doors were kept closed with entry and exit activity prevented. Many of these draconian measures may not be practical in all surgical environments.
Loud and frequent sound sources represent an obvious contribution to the noise problem, but a more complete consideration should include the contribution of room construction and design on room acoustics. The Facility Guidelines Institute has published consensus-based guidelines to inform architectural and engineering practice in the design of new health care facilities that include guidelines for wall and ceiling acoustic finishes that achieve some degree of sound absorption.20 For extant health care facilities, architectural modification can be prohibitive due to expense, invasiveness, and the potential to disrupt patient care. However, a few studies have demonstrated that minor retrofits aimed at decreasing sound reflection from walls and ceilings (reverberation) can be effective in improving the soundscape environment.21,22 After affixing simple sound-absorbing panels to decrease sound reverberation in a busy patient ward, sound levels decreased significantly, and staff and patient experience improved; the sound levels likely decreased because with decreased reverberation, voice levels can be decreased while maintaining intelligibility.21 Similar improvements in acoustics and occupant experience were observed in a coronary critical care unit when sound-absorbing ceiling panels were in place; no benefit was observed when sound-reflecting panels of identical appearance were used.22 To our knowledge, similar interventions have not been tested in the OR setting.
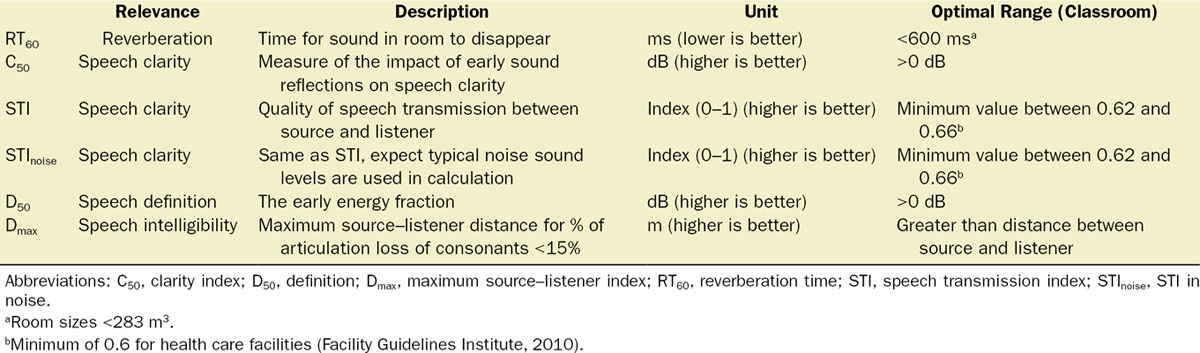
Reverberation is commonly assessed by measuring reverberation time (RT60), the time required for reflected sound levels to decrease by 60 dB, and it is one index among others related to speech intelligibility that we studied in this article (see Table 1). Although ORs have often been cited for being highly reverberant settings,17,23,24 quantitative studies and reporting of indices of speech intelligibility are lacking. The first objective of this article begins to address how OR design and construction affect acoustics. These data could be used to support development of innovative countermeasures to mitigate the noise problem and improve communication and alarm signaling in existing surgical suites. We performed a psychoacoustic analysis of 6 surgical suites at our institution. The suites are comprised of 44 ORs, located in hospital wings and, in some instances, distinct buildings. Collectively, they represent a convenient cross-section of OR design and construction that may be applicable to other institutions. Our second objective was to investigate the relationships between room acoustics, room size, and content using the data set obtained from the first objective. This objective is centered on the principle that reverberation is known to increase with increasing room size and increasing surface reflectiveness to sound.25 It is also based on the results of a pilot study (the data from which are presented here), which suggested that the number of typical objects present in an OR could impact its acoustics.
Table 1.
Speech Intelligibility Indices
METHODS
Acoustical Analyses of Surgical Suites
A detailed reporting of the acoustical analysis used in this study is described by us elsewhere.26 Briefly, each OR was analyzed by playing a series of sweep tones of ascending pitch (Supplemental Digital Content 1, Audio, http://links.lww.com/AA/B756) from a speaker directed at a room corner. The resulting sound fields, referred to as impulse responses, were recorded from 3 different locations in the room at least 1.5 m apart, with recording locations at least 1 m from any room surface or object (Figure 1A). Five impulse response recordings were obtained from each recording location, averaged, and then analyzed using custom Matlab (MathWorks, Natick, MA) scripts to calculate 6 psychoacoustic indices of speech intelligibility (Table 1): RT60, speech transmission index (STI), STI in noise (STInoise), clarity index (C50), definition (D50), and maximum source–listener index (Dmax). These speech intelligibility indices have been empirically validated in laboratory settings in subjects. Importantly, RT60 is present in the formulae used to calculate the other 5 indices, and Dmax is distinguished from the latter by also basing its calculation on room size.26
Figure 1.
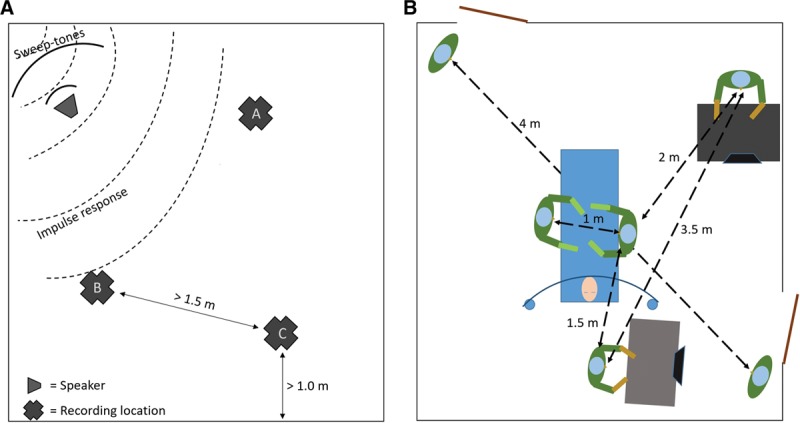
Schematics showing general equipment setup for performing acoustical analyses of operating rooms (A) and typical communication distances between operating room occupants at our institution (B).
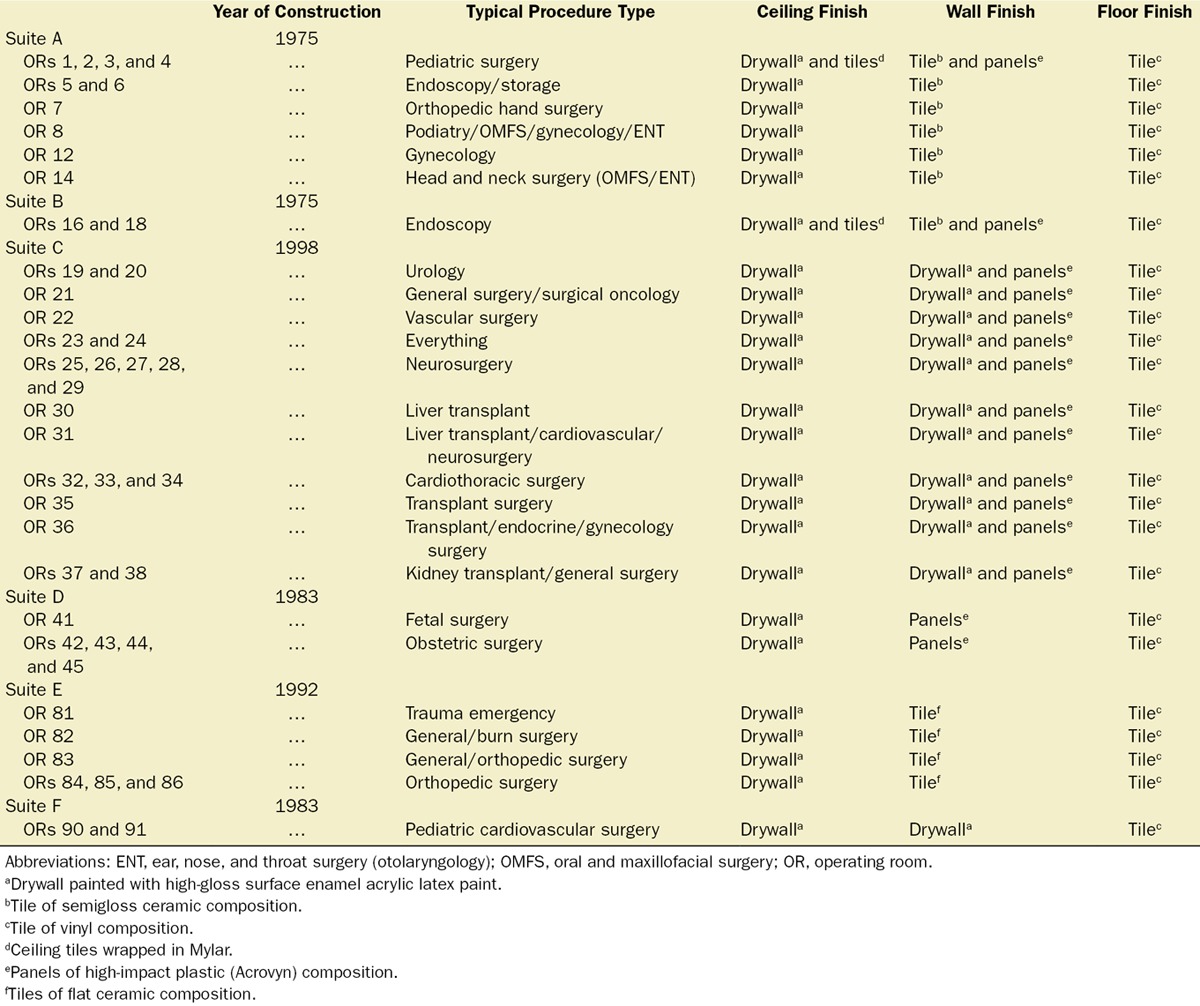
Collection of Surgical Suite Construction and Design Details
Experiments took place during a 5-day period at Jackson Memorial Hospital (JMH), a large, urban county hospital that includes a stand-alone level 1 trauma center and a pediatric hospital. There are 6 individual surgical suites and a total of 44 ORs. While some ORs are used for variable specialties and procedures, others are typically used for one or more surgical specialties. In order to gather these data, the OR case schedule was reviewed for 9 days, and the surgical specialties operating in each OR were noted. After making note of trends, the OR coordinator was consulted in order to confirm or add information to the list of specialties that typically utilize each OR. To determine year of OR construction, floor plans and construction renderings of the hospital areas that contain ORs were reviewed with one of the engineering drafters in the facilities design and construction department offices. The dates of OR construction were noted and confirmed to the best of the knowledge of design and construction staff. To determine the materials used to finish OR surfaces, the assistant director of the JMH engineering department was consulted and arranged for a tour of each OR by a designated foreman typically working in the corresponding hospital wing. The materials of each surface of each OR were visualized and discussed with each foreman and then confirmed with the assistant director. When necessary, the program consultant overseeing JMH construction and design programs was consulted.
Assessment of OR Size, Contents, and Development of Room Content Metric
Room dimensions were measured to calculate room spatial volumes in cubic meters (VR). Room contents were left as found during analysis except in specific circumstances described below. Documentation of room content was facilitated by taking equirectangular panoramic (also known as spherical 360°) photographs (see examples in Supplemental Digital Content 2 and 3, Figures 1 and 2, http://links.lww.com/AA/B757 and http://links.lww.com/AA/B758) immediately after each analysis with a smartphone (HTC One M8, Taoyuan, TW). A freeware program (FSPViewer 2.0.0, Prof. H. Dersh, Hochschule Furtwangen University) was used to later review the photographs on a desktop computer (Windows 10, Microsoft, Redmond, WA). Room items were classified into 5 categories based on estimated size ratios of items: “small” (kick bucket, stepstool, small garbage can, and intravenous pole); “medium-small” (mayo stand, forced convection blanket blower, chair, intravenous pole with infusion pump[s], medium garbage can, sharps box, and OR swing light); “medium” (metal table, electrocautery machine, trash bag holder and bag, large garbage can, computer tower, nurse’s desk, and desk cart); “medium-large” (anesthesia workstation, equipment cart, OR bed, and laparoscopic tower); “large” (Omnicell, Mountain View, CA, blanket warmer, microscope, and mini C-arm). In order to obtain an intervallic parameter referred to as the “room content metric” (VC), the small and large categories were assigned weights of 1 and 512, respectively. This ratio was based on the estimation that a large item is 8 times larger than a small item along one dimension and in terms of volume, 83 = 512. The intervening categories were then weighted to be equidistantly spaced on a natural log scale between the small and large categories and are as follows: small = 1, medium-small = 4.74, medium = 22.50, medium-large = 106.61, and large = 512. For each room, VC was calculated by multiplying the number of category items by corresponding category weight and summing the results.
Pilot Study
We originally decided to pursue our second objective, and in particular to include room content as a parameter-of-interest based on the results of a pilot study that we report in this article. We performed the acoustic analysis (see Acoustical Analyses of Surgical Suites) in a single room with its normal content intact (full), and then with most of its contents removed (empty). We did not remove the nurse’s desk with associated computer and other electronic equipment in order to not disrupt workflow and network connectivity. In addition to the nurse’s desk, the empty state was necessarily characterized by the presence of the equipment used to perform the acoustic analysis (this is also true for the other ORs studied). Equirectangular panoramic images of the OR in these 2 states can be downloaded from Supplemental Digital Content 2 and 3, Figures 1 and 2, http://links.lww.com/AA/B757 and http://links.lww.com/AA/B758, and viewed with an appropriate viewer. Impulse responses were recorded 5 times per location from the same 3 locations within the OR for both states (Figure 1A). The 6 indices of speech intelligibility were subsequently calculated as described in Acoustical Analyses of Surgical Suites.
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics (version 24; IBM, Armonk, NY). For the pilot study, a repeated-measures analysis of variance was performed with room content as the within-subjects factor consisting of 2 levels: empty and full. Results are reported for univariate within-subjects comparison of each of the intelligibility indices. In order to investigate the relationships between room acoustics and room size and content, multiple linear regression analysis was performed treating VR and VC, after natural log transformation, as predictor variables and each index of speech intelligibility separately as an outcome variable. Assumptions of linear regression were tested as follows: (1) predictor variable multicollinearity was assessed by examining the bivariate correlation, tolerances, and variance inflation factors; (2) predictor independence of observation was assessed by calculating the Durbin–Watson statistic; (3) normality of variables was assessed by examining the Shapiro–Wilk test and histograms; (4) assumption of linearity was assessed by examining scatter plots of outcome as a function of predictor variables and scatter plots of the regression standardized residual (standardized residuals) as a function of the regression standardized predicted value (standardized predicted values); and (5) homoscedasticity was assessed by examining scatter plots of the standardized residuals as a function of standardized predicted values. Next, multiple linear regression was performed using a forced-entry approach, and a partial correlation analysis was conducted. To assess for data redundancy among the 6 outcome variables, a principal component analysis (direct oblimin rotation) was performed. Significance of extracted components was assessed by examining component eigenvalues (values >1 were considered significant).
Power Analysis.
Power analysis was performed using G*Power 3.1.9.2 (test family: “F-tests,” statistical test: “linear multiple regression: fixed model, R2 deviation for 0”). A sample size of 44 ORs was chosen for the regression analysis based on the total number of ORs at our institution. Our expected effect size (R2) was 0.30, which gives Cohen’s f2 equal to 0.429. Because there were 6 outcome variables (ie, 6 regression models) to be tested, the α level after Bonferroni adjustment was conservatively set at .0083. There were 2 explanatory variables. Based on these, the available power was calculated to be .87.
Reduction of Type I Error.
To decrease the risk of type I error, we adjusted P values with a Bonferroni method that accounts for the observed correlation in the 6 intelligibility indices.27 This strategy helps reduce the risk of type II error when outcome data are redundant. The P values were adjusted for the 6 linear regression models using this method. Then P values were further adjusted for VR and VC using Bonferroni correction based on 2 outcomes. Confidence intervals for the VR and VC partial correlations were likewise adjusted.
RESULTS
Results From Pilot Study
Manipulation of room content had an impact on room acoustics in a selected OR (P < .05; Supplemental Digital Content 4, Figure 1, http://links.lww.com/AA/B759). Significant differences were observed between the empty and full states for RT60 (1.08 [0.04] vs 0.81 [0.04], P < .05), STI (0.77 [0.00] vs 0.82 [0.01], P < .001), STInoise (0.67 [0.00] vs 0.70 [0.00], P < .001), C50 (1.25 [0.17] vs 1.70 [0.24], P < .005), D50 (0.55 [0.03] vs 0.63 [0.03], P < .05), and Dmax (1.10 [0.05] vs 1.36 [0.04], P < .001), and all indices were less favorable for speech intelligibility in the empty state as reflected by the criteria presented in Table 1. This result suggested that inclusion of VC in our investigation would be justified.
Results From Objective No. 1
Twenty-three years separate the oldest from the most recent of the surgical suites studied (Table 2). Most of the OR ceilings consist of drywall painted with a high-gloss surface enamel acrylic latex paint. Some also contain small areas of ceiling tile wrapped in Mylar (DuPont, Wilmington, DE), a type of polyester resin that is heat resistant. The wall finishes are variable depending on OR but include the following materials: drywall, semigloss ceramic tile, flat ceramic tile, and a protective hard plastic cover (Acrovyn; C/S, Lebanon, NJ) that covers either the bottom half or the entire wall. All OR floors are vinyl composition tile.
Table 2.
OR Surface Finish Characteristics
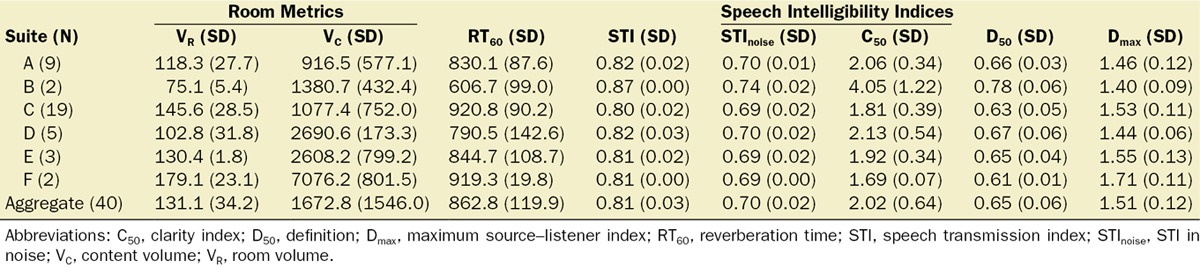
A total of 40 ORs were studied (4 ORs were not available during the 5-day period of our analysis). Descriptive results grouped by OR suite for both VR and VC and the 6 intelligibility indices are shown in Table 3. An insignificant correlation was observed between VR and VC (Pearson correlation = 0.223, P = .166; Supplemental Digital Content 5, Figure 2, http://links.lww.com/AA/B760). Descriptive results grouped by OR suite for the 6 speech intelligibility indices are shown in Table 3. Principal component analysis indicates that 79.42% of the variance in these indices can be explained by 1 component, and that 95.80% can be explained by 2 components, although the second component just missed significance due to an eigenvalue (0.983) <1. In the 2-component extraction, the first component loaded with RT60, STI, STInoise, C50, and D50, while the second component loaded with Dmax (Supplemental Digital Content 6, Table 1, http://links.lww.com/AA/B761).
Table 3.
Descriptive Results Grouped by Surgical Suite
Results From Objective No. 2
Assumptions for linear regression were satisfied as they pertain to VR and VC and each of the 6 indices of speech intelligibility. The results of multiple linear regression and partial correlation analyses are shown in Table 4; additional linear regression results including β coefficients and constants can be found in Supplemental Digital Content 7, Table 2, http://links.lww.com/AA/B762.
Table 4.
Regression Model Resultsa With Partial Correlations (N = 40)
DISCUSSION
At our institution, the average maximum distance at which there is less than a 15% loss of consonant articulation (Dmax, which we will also refer to going forward as the optimum communication distance) is about 1.5 m. To put this in perspective, after informally measuring typical distances between relevant personnel at our institution (Figure 1B), we propose that individuals in our ORs whose roles keep them in the vicinity of the OR bed are most likely to be routinely within measured optimum communication distances. Increasing room size, as expected, was shown to be correlated with increased amounts of room reverberation as measured by RT60, and in general to correlate with less favorable resultant values for STI, STInoise, C50, and D50. Not unexpectedly, these 5 indices were also observed to track together (or were redundant) based on our principal component analysis. However, Dmax did not track with the other indices and was observed to increase with increasing room size when adjusted for RT60. This is explainable based on the fact that unlike the other indices, the formulaic definition of Dmax depends on both RT60 and room size. Due to redundancy and since the best regression model fit and significant partial correlations were for RT60 and Dmax, respectively, we propose that outcome measurements in future studies can ignore STI, STInoise, C50, and D50. We also present a way to show the relationships between RT60, room size, and Dmax in the form of a contour or isoline plot on which we also superimpose our OR data points (Figure 2). Two generalizations can be drawn from this type of plot: (1) for a given room size, efforts to decrease room reverberation will increase the optimum communication distance between 2 individuals; and (2) larger room size is correlated with increased optimum communication distance when predicted concomitant increases in room reverberation can be mitigated or prevented. Not represented in Figure 2 is the beneficial impact room content may have on reverberation and optimum communication distance, decreasing the former (P = .169) while increasing the latter (P < .05), as shown in Table 4. This is understandable considering that room objects are expected to absorb or scatter (filter) sound energy. While studying our OR suites, we often anecdotally observed that some of the smallest rooms seemed to be relatively more packed and cramped than our largest rooms that often had wide open spaces, and these observations may partly explain the insignificant correlation we observed between room size and content metric at our institution. Formal investigation is warranted to determine whether mismatch between room size and room content, specifically with respect to large rooms with relatively few contents, can have a clinically significant detrimental impact on room acoustics. Of note, the suite with the largest ORs analyzed at our institution (Suite F in Table 3) had an average measured RT60 of 919.3 ms (as well as the largest measured Dmax), a value more consistent with smaller OR sizes. We attribute this finding to the impact of room content (this OR suite also had the largest estimated VC) and to serendipitously favorable matching between VR and VC.
Figure 2.
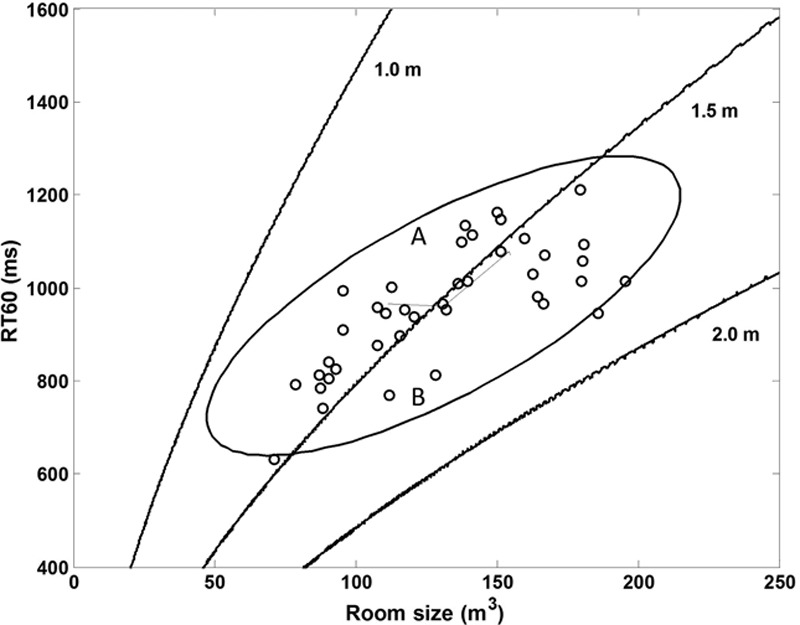
Contour plot showing use of our data to illustrate the relationship between RT60, room size, and Dmax (represented by the isolines). A room in which RT60 is manipulated between 2 levels will occupy 2 locations along a vertical line on the plot (eg, points labeled A and B). The 95% confidence ellipse for our data is shown and was calculated using a custom Matlab script. Dmax indicates maximum source–listener index; RT60, reverberation time.
An important next step will be to determine the relationships between room acoustics and clinically relevant outcome measures. While typical OR sound levels can range from 62 to 72 dBA,28 Engelmann et al19 showed in a nonrandomized, prospective study that decreasing noise levels from 63 to 59 dBA in a pediatric surgical suite was associated with improvement in team communication and a decrease in postoperative complication rate. We previously demonstrated in a randomized, controlled, simulation-based experiment that exposure to typical OR background noise is associated with increased perception of fatigue and task load levels by anesthesia residents.12 Measured noise level depends on direct sounds emanating from room sources and the sound reflected from room surfaces. A source producing a constant level of sound may therefore contribute more to noise levels, especially for late reflected sounds, as room reverberation increases.25 Contribution of verbal communication to noise level is a special case, since as speech intelligibility decreases, the natural action by stakeholders is an escalation of voice levels. Countering of this positive feedback loop was suggested by MacLeod et al21 as the reason overall noise levels decreased by 5 dBA after sound-absorbing panels were installed in a patient ward; nurses also reported improved communication and concentration during morning report and patient sign-offs. Several studies suggest that when RT60 increases and approaches 1 second, intelligibility of speech signals is decreased for individuals independent of hearing ability,29,30 and there is evidence that that the detrimental impact of RT60 on intelligibility is greater in the presence of background noise than in isolation.31,32 Based on our results, increasing room volume from 75 to 150 m3, a size span represented at our institution, predicts an increase in RT60 from about 0.8 to 1.2 seconds, potentially representing a large effect, and the concomitant presence of typically high-intraoperative background noise would be expected to compound this effect. Further investigations are needed to study the role of room acoustics on perioperative outcome measures, and the methodology presented here will be helpful. In this regard, we plan, for example, to experimentally manipulate RT60 in our OR suites, as illustrated in Figure 2 (see the A and B markers) through the use of acoustical treatments.
There are several limitations associated with this study. First, the results of our first objective show that our surgical suites are composed of a highly heterogeneous group of ORs (see Table 2), and factors expected to affect room acoustics, such as age of construction, surface finishes, and room shape, were not controlled for in our regression model and partial correlation analysis. Nonetheless, we observed (resilient) correlations despite OR heterogeneity between all intelligibility indices and room size and between both RT60 and Dmax indices and room content. Therefore, the data obtained in our ORs may potentially be extrapolated to other institutions. Ultimately, multisite efforts would be useful to build a more representative database that can help establish the scope of the problem, allow interinstitutional comparisons and guide future research. In this regard, the relationships-of-interest as depicted in Figure 2 may be useful. A second limitation is that the process used to calculate VC was arbitrary and not based on actual object size, volume, shape, or type of surface, but rather on estimation and there is clearly room for improvement in this regard. Additionally, some objects such as a metal OR instrument table would be expected to be more reflective to sound than an OR bed that might be more absorptive to sound, for example. It is possible that had these and other factors been incorporated into VC, weaker correlation would have been observed. However, it is also possible that the aforementioned refinements in how room content is calculated in the future will result in improved model fits and increase the predictive value and utility of the approach.
CONCLUSIONS
Our results suggest that the size and contents of an OR (eg, anesthesia machine, carts, tables, and garbage cans) can predict a range of psychoacoustic indices of speech intelligibility. Generally, increasing OR size correlated with worse speech intelligibility, while increasing amounts of OR contents correlated with improved speech intelligibility. This study provides a method for studying and identifying existing ORs that may benefit from acoustic modifiers (eg, sound-absorption panels). Additionally, it suggests that room dimensions and projected clinical use may be a consideration during the design phase of OR suites to optimize acoustic performance.
DISCLOSURES
Name: Richard R. McNeer, MD, PhD.
Contribution: This author helped design the study, conduct the study, analyze the data, perform the statistical analysis, and write the manuscript.
Name: Christopher L. Bennett, PhD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Name: Danielle Bodzin Horn, MD.
Contribution: This author helped conduct the study, analyze the data, and write the manuscript.
Name: Roman Dudaryk, MD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
This manuscript was handled by: Nancy Borkowski, DBA, CPA, FACHE, FHFMA.
Supplementary Material
Footnotes
Funding: None.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website.
Reprints will not be available from the authors.
REFERENCES
- 1.Busch-Vishniac IJ, West JE, Barnhill C, Hunter T, Orellana D, Chivukula R. Noise levels in Johns Hopkins Hospital. J Acoust Soc Am. 2005;118:3629–3645. [DOI] [PubMed] [Google Scholar]
- 2.Baker CF. Sensory overload and noise in the ICU: sources of environmental stress. CCQ. 1984;6:66–80. [PubMed] [Google Scholar]
- 3.Novaes MA, Knobel E, Bork AM, Pavão OF, Nogueira-Martins LA, Ferraz MB. Stressors in ICU: perception of the patient, relatives and health care team. Intensive Care Med. 1999;25:1421–1426. [DOI] [PubMed] [Google Scholar]
- 4.Cmiel CA, Karr DM, Gasser DM, Oliphant LM, Neveau AJ. Noise control: a nursing team’s approach to sleep promotion. Am J Nurs. 2004;104:40–48. [DOI] [PubMed] [Google Scholar]
- 5.Aaron JN, Carlisle CC, Carskadon MA, Meyer TJ, Hill NS, Millman RP. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep. 1996;19:707–710. [DOI] [PubMed] [Google Scholar]
- 6.Parthasarathy S, Tobin MJ. Sleep in the intensive care unit. Intensive Care Med. 2004;30:197–206. [DOI] [PubMed] [Google Scholar]
- 7.Cureton-Lane RA, Fontaine DK. Sleep in the pediatric ICU: an empirical investigation. Am J Crit Care. 1997;6:56–63. [PubMed] [Google Scholar]
- 8.Czaplik M, Rossaint R, Kaliciak J, et al. Psychoacoustic analysis of noise and the application of earplugs in an ICU: a randomised controlled clinical trial. Eur J Anaesthesiol. 2016;33:14–21. [DOI] [PubMed] [Google Scholar]
- 9.Dholakia S, Jeans JP, Khalid U, Dholakia S, D’Souza C, Nemeth K. The association of noise and surgical-site infection in day-case hernia repairs. Surgery. 2015;157:1153–1156. [DOI] [PubMed] [Google Scholar]
- 10.Kurmann A, Peter M, Tschan F, Mühlemann K, Candinas D, Beldi G. Adverse effect of noise in the operating theatre on surgical-site infection. Br J Surg. 2011;98:1021–1025. [DOI] [PubMed] [Google Scholar]
- 11.Wysocki AB. The effect of intermittent noise exposure on wound healing. Adv Wound Care. 1996;9:35–39. [PubMed] [Google Scholar]
- 12.McNeer RR, Bennett CL, Dudaryk R. Intraoperative noise increases perceived task load and fatigue in anesthesiology residents: a simulation-based study. Anesth Analg. 2016;122:512–525. [DOI] [PubMed] [Google Scholar]
- 13.Morrison WE, Haas EC, Shaffner DH, Garrett ES, Fackler JC. Noise, stress, and annoyance in a pediatric intensive care unit. Crit Care Med. 2003;31:113–119. [DOI] [PubMed] [Google Scholar]
- 14.Topf M, Dillon E. Noise-induced stress as a predictor of burnout in critical care nurses. Heart Lung. 1988;17:567–574. [PubMed] [Google Scholar]
- 15.Beyea SC. Noise: a distraction, interruption, and safety hazard. AORN J. 2007;86:281–285. [DOI] [PubMed] [Google Scholar]
- 16.Katz JD. Noise in the operating room. Anesthesiology. 2014;121:894–898. [DOI] [PubMed] [Google Scholar]
- 17.Kracht JM, Busch-Vishniac IJ, West JE. Noise in the operating rooms of Johns Hopkins Hospital. J Acoust Soc Am. 2007;121:2673–2680. [DOI] [PubMed] [Google Scholar]
- 18.Fritsch MH, Chacko CE, Patterson EB. Operating room sound level hazards for patients and physicians. Otol Neurotol. 2010;31:715–721. [DOI] [PubMed] [Google Scholar]
- 19.Engelmann CR, Neis JP, Kirschbaum C, Grote G, Ure BM. A noise-reduction program in a pediatric operation theatre is associated with surgeon’s benefits and a reduced rate of complications: a prospective controlled clinical trial. Ann Surg. 2014;259:1025–1033. [DOI] [PubMed] [Google Scholar]
- 20.Anonymous. 2014 FGI Guidelines for Hospitals and Outpatient Facilities. 2015. Available at: https://www.fgiguidelines.org/product/2014-guidelines-for-design-and-construction-of-residential-health-care-and-support-facilities-2/. Accessed April 24, 2017.
- 21.MacLeod M, Dunn J, Busch-Vishniac IJ, West JE, Reedy A. Quieting Weinberg 5C: a case study in hospital noise control. J Acoust Soc Am. 2007;121:3501–3508. [DOI] [PubMed] [Google Scholar]
- 22.Blomkvist V, Eriksen CA, Theorell T, Ulrich R, Rasmanis G. Acoustics and psychosocial environment in intensive coronary care. Occup Environ Med. 2005;62:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stringer B, Haines TA, Oudyk JD. Noisiness in operating theatres: nurses’ perceptions and potential difficulty communicating. J Perioper Pract. 2008;18:384, 386–391. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro RA, Berland T. Noise in the operating room. N Engl J Med. 1972;287:1236–1238. [DOI] [PubMed] [Google Scholar]
- 25.Hodgson M, Nosal EM. Effect of noise and occupancy on optimal reverberation times for speech intelligibility in classrooms. J Acoust Soc Am. 2002;111:931–939. [DOI] [PubMed] [Google Scholar]
- 26.Bennett CL, Dudaryk R, Ayers AL, McNeer RR. Simulating environmental and psychological acoustic factors of the operating room. J Acoust Soc Am. 2015;138:3855–3863. [DOI] [PubMed] [Google Scholar]
- 27.Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med. 1997;16:2529–2542. [DOI] [PubMed] [Google Scholar]
- 28.Tsiou C, Efthymiatos G, Katostaras T. Noise in the operating rooms of Greek hospitals. J Acoust Soc Am. 2008;123:757–765. [DOI] [PubMed] [Google Scholar]
- 29.Sato H, Sato H, Morimoto M, Ota R. Acceptable range of speech level for both young and aged listeners in reverberant and quiet sound fields. J Acoust Soc Am. 2007;122:1616. [DOI] [PubMed] [Google Scholar]
- 30.Nábělek AK, Pickett JM. Reception of consonants in a classroom as affected by monaural and binaural listening, noise, reverberation, and hearing aids. J Acoust Soc Am. 1974;56:628–639. [DOI] [PubMed] [Google Scholar]
- 31.Harris RW, Reitz ML. Effects of room reverberation and noise on speech discrimination by the elderly. Audiology. 1985;24:319–324. [DOI] [PubMed] [Google Scholar]
- 32.Finitzo-Hieber T, Tillman TW. Room acoustics effects on monosyllabic word discrimination ability for normal and hearing-impaired children. J Speech Hear Res. 1978;21:440–458. [DOI] [PubMed] [Google Scholar]


