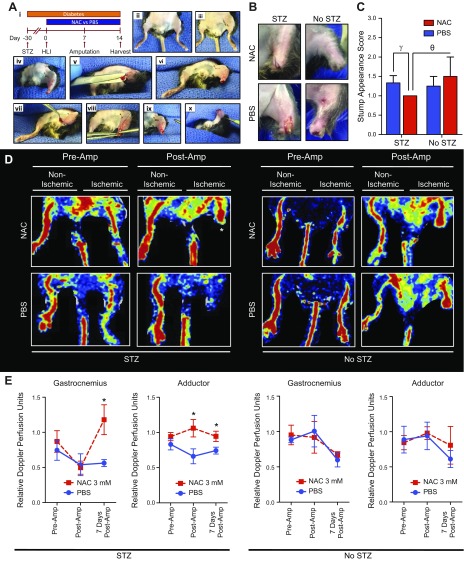
Figure 1.
NAC improves ischemic hindlimb stump perfusion and appearance. A) In a novel hindlimb ischemia-amputation model (i), mice were pretreated with STZ to induce hyperglycemia over a 1-mo period followed by staged unilateral hindlimb ischemia (HLI), infrageniculate amputation 7 d later, and tissue harvest 14 d later. HLI was performed through a small subcentimeter incision in the adductor region (ii, iii) After a 7-d recovery period, a guillotine transtibial amputation was performed under general anesthesia with aseptic technique (iv). Remnant proximal tibia was further resected to create an adequate ventral tissue rotational flap (v, vi). The ventral tissue flap was rotated over the amputation site to create a durable stump closure. The stump was closed using 3 interrupted 6-0 silk sutures (vii–x). B) Amputation stumps of diabetic and nondiabetic mice treated with NAC improved healing. There was no significant edema or inflammation in the NAC and PBS groups. C) Stump appearances were improved (lower appearance scores) in diabetic (10 NAC, 12 PBS) and nondiabetic (4 NAC, 4 PBS) mice 3 and 7 d after amputation. D) Diabetic and nondiabetic mice that were treated with NAC demonstrated higher amputation stump perfusion 7 d postamputation, particularly diabetic mice (indicated by an asterisk). E) Diabetic (7 NAC, 5 PBS) and nondiabetic (5 NAC, 3 PBS) mice demonstrated significantly increased perfusion in the gastrocnemius and adductor regions of healing ischemic hindlimb amputation stumps of mice treated with NAC for 14 d (d 1–14). *P < 0.05, γP = 0.06.