Figure 2.
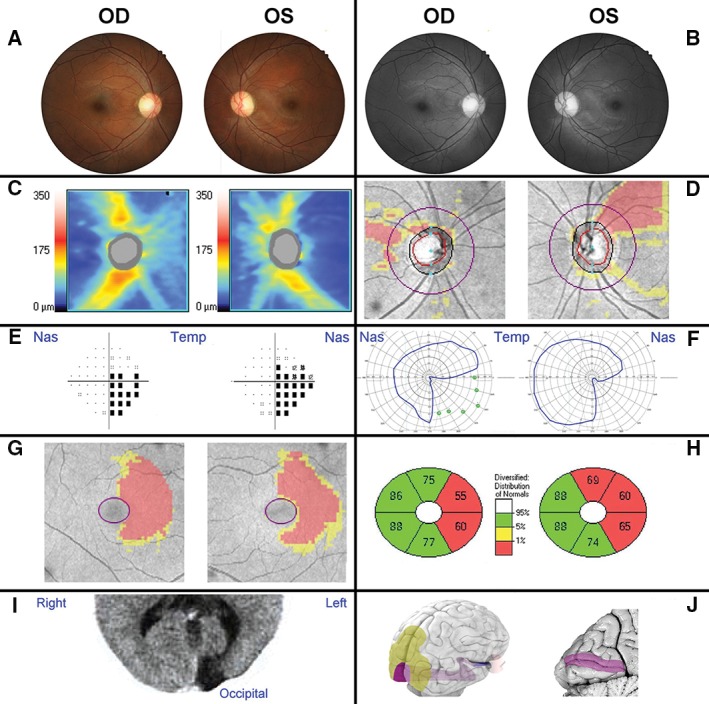
Clinical examination of a 38‐year‐old male patient with neuropathy. Patient 1 had no systemic conditions, relevant family and/or medical history. Visual acuity (6/7.6 R, 6/6 L) and intraocular pressures (15 mmHg OU) were near normal range and no relative afferent pupil defect was present. A. The patient presented with a possible temporal pallor of the optic nerve head and slight superior sloping of the left retinal rim. B. Red‐free photography of the posterior pole further indicated superotemporal retinal nerve fibre drop‐out consistent with a potential arcuate defect. C, D. The retinal nerve fibre layer defects were confirmed by optical coherence tomography images, as shown by the thickness heat map (C) and deviation map (D). E–H. A central 24–2 threshold visual field test identified a right inferior quadrantanopia (pattern deviation), which was corroborated by the restricted pattern obtained with Goldmann perimetry (F, blue outlines) and agrees with the ganglion cell analysis deviation map (G) and sector thickness analysis (H). I. Computerised axial tomography revealed an area of hyporeflectivity at the left occipital brain pole. J. An overview of the anatomy of the visual system from a right caudolateral view onto the brain illuminates the position of the optic nerve, optic tract and visual radiation (blue/purple) in relation to the eye and visual cortex (purple) and association areas (yellow). A sagittal section through the visual cortex (left side) reveals the calcarine fissure corresponding to the aberrant area in the patient's brain scan.
