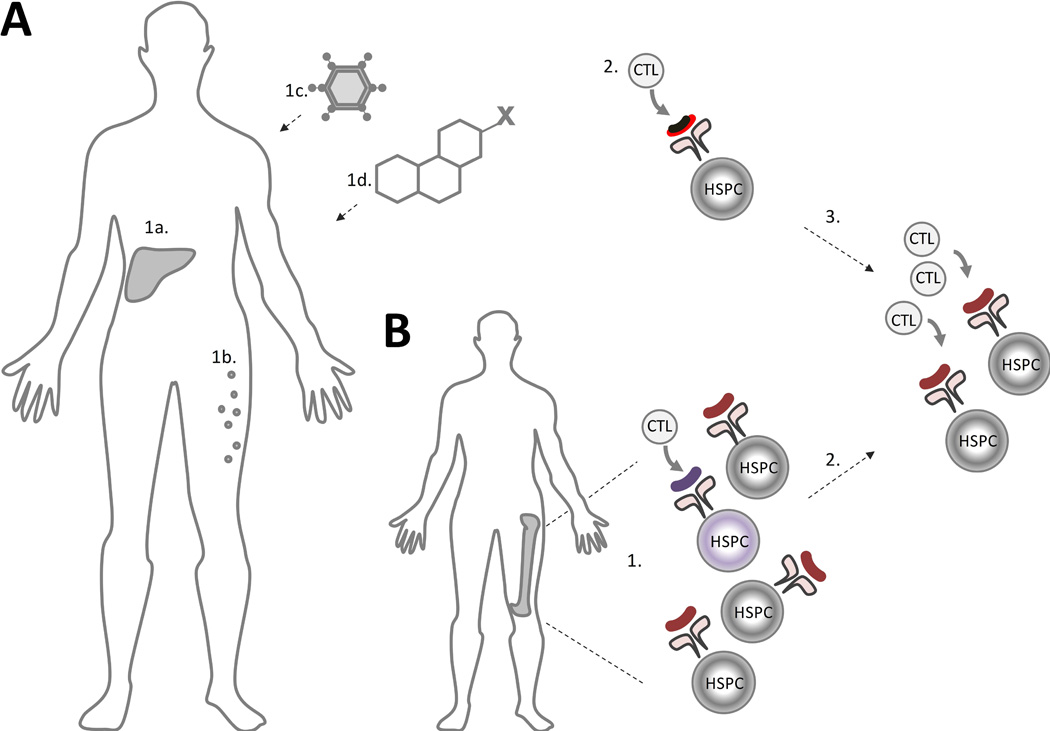
Figure 4. Model of Autoimmune Pathogenesis of AA and of the AA/MDS Overlap Syndrome.
A) In aplastic anaemia (AA), an immune trigger, such as type-negative hepatitis (1a), eosinophilic fasciitis (1b), or an exposure to an infectious agent (1c), drug or toxin (1d) leads to immune recognition of a neoantigen or an aberrantly expressed autoantigen (black and red line) presented in the context of a patient’s human leucocyte antigen (HLA) molecules (2). (3) Immune-mediated bone marrow aplasia is caused by subsequent clonal expansion of cytotoxic T lymphocytes (CTL) with autoreactivity against the normal haematopoietic stem and progenitor cells (HSPCs) due to epitope spread. B) In patients with coexisting AA and myelodysplastic syndrome (MDS), pre-existing MDS-related mutations may lead to presentation of an aberrantly-expressed or somatically modified neoantigen in the MDS HSPC (1) (shown in purple). Unlike the traditional model of AA, where a T-cell mediated immune response is directed at the healthy HSPCs, patients with the overlap AA/MDS have the immune response triggered by an underlying MDS clone with immune-mediated aplasia to the “bystander” wild type HSPCs (2).