Abstract
INTRODUCTION
This study aimed to explore the level of knowledge of Muslim patients with diabetes mellitus (DM) regarding DM and the self-management of DM when fasting during Ramadan.
METHODS
Muslim patients with DM attending the Diabetes Centre of Singapore General Hospital, Singapore, were surveyed on their knowledge of DM and self-management of DM when fasting during Ramadan. Data on patient demographics, DM history and management of DM during the previous Ramadan was also collected.
RESULTS
A total of 92 patients (34 male, 58 female) were surveyed. The mean age of the patients was 53.4 ± 13.3 years. The patients were either Malay (91.3%) or Indian (8.7%), and most (66.3%) had at least a secondary school education. Most (89.1%) had Type 2 DM. The mean duration of DM was 8.7 ± 5.1 years and mean pre-Ramadan haemoglobin A1c was 8.4% ± 1.8%. DM treatment consisted of insulin therapy (37.0%), oral glucose-lowering drugs (35.9%) and combined therapy (22.8%). The mean DM knowledge score was 58.8% for general knowledge and 75.9% for fasting knowledge. During the previous Ramadan, although 71.4% of the patients consulted their physicians, 37.3% did not monitor their blood glucose levels and 47.0% had hypoglycaemic episodes. Among those who had hypoglycaemia, 10.8% continued to fast.
CONCLUSION
Unsafe self-management practices were observed among DM patients who fasted during Ramadan. Efforts should be made to bridge the gap between knowledge of DM and self-management of DM.
Keywords: diabetes mellitus, fasting, knowledge, self-management
INTRODUCTION
There is a global avalanche of patients with diabetes mellitus (DM). In 2013, 382 million people were living with DM, a number that is projected to increase to 592 million by 2035.(1) Even more alarming is the trend toward younger people developing DM. The global prevalence of DM in 2013 was estimated to be 8.3% among those aged 20–79 years, with the largest increment occurring in the Middle East and Africa (by approximately 100%).(1) In Singapore, the National Health Survey 2010 reported that DM affects 11.3% of those aged 18–69 years.(2) This is an increase from the 8.2% reported in 2004, with the largest increment occurring among the Malay population. As most Malays are Muslims, this increased prevalence of DM among Malays translates to the likelihood that more individuals with DM fast during the Islamic month of Ramadan. As Muslims practise daytime fasting for 30 consecutive days during Ramadan, Muslims with DM who fast have an increased risk of both hyperglycaemia and hypoglycaemia during Ramadan.(3)
Knowledge of DM is a prerequisite for appropriate self-management. Previous studies conducted in Singapore have demonstrated good levels of knowledge about DM among individuals with and without DM.(4-6) However, studies performed in other countries suggest that deficits in knowledge can result in inappropriate practices among DM patients who fast during Ramadan(7) and among healthcare providers caring for these patients.(8) In Malaysia, Yaacob et al found that knowledge deficits (especially regarding hypoglycaemia recognition) and inappropriate practices were prevalent even though their study population had a good attitude toward disease control and had pre-Ramadan consultations with their physicians.(7)
To the best of our knowledge, no study has specifically examined the knowledge adequacy of Muslim patients with DM in Singapore regarding the subject of self-management during Ramadan fasting. Thus, this study aimed to evaluate the knowledge of this group of patients about DM and self-management of DM during the fasting month of Ramadan.
METHODS
This cross-sectional study was approved by the local institutional ethics committee and performed in accordance with the ethical standards of the Declaration of Helsinki. It was conducted over a period of three months (June 2011–August 2011) at the Diabetes Centre of Singapore General Hospital (SGH), Singapore. SGH is a tertiary centre and the annual attendance of the Diabetes Centre is approximately 19,000 patients. The study participants were Muslim patients aged ≥ 16 years with DM who attended outpatient appointments at the Diabetes Centre. Consecutive patients attending their clinic appointments were approached. If they agreed to participate in the study, informed consent was obtained and they were included. Patients who were not able to complete the questionnaire were excluded.
This study was conducted using a self-administered questionnaire that was developed by one of the authors of the study. The questionnaire, which was available in both the English and Malay languages, required 15–20 minutes to complete. It included questions on the patients’ sociodemographic data, history of DM (i.e. type and duration of DM, treatment received for DM and pre-Ramadan haemoglobin A1c [HbA1c] level), knowledge of DM and information regarding the management of DM during the previous Ramadan.
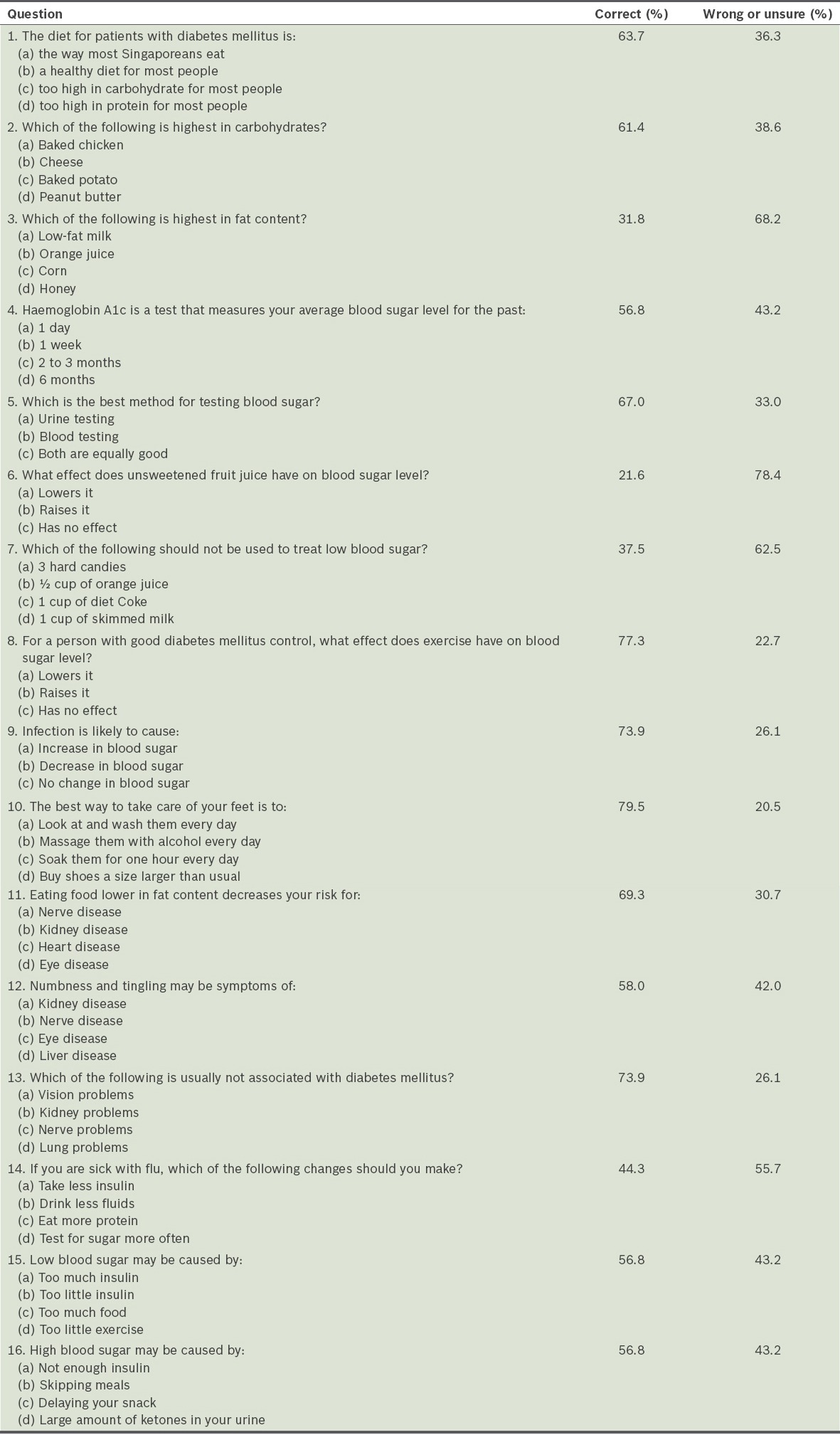
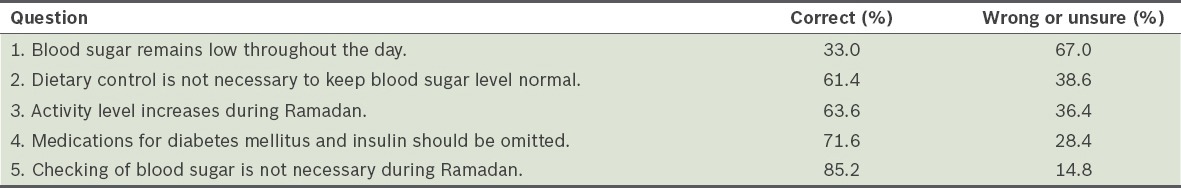
The patients’ knowledge was assessed with questions that were grouped into four main sections; each section focused on a different aspect of knowledge about DM, including management of the disease when fasting during Ramadan. Section 1 tested the patients’ general knowledge of DM using a modified, 16-item version of the validated Michigan Diabetes Knowledge Test (MDKT).(9) All of the questions from the original MDKT were retained, except for Questions 4, 15, 17, 18, 19, 21 and 23, and one option each in Questions 1 and 2 were modified to better suit the Singapore population (Appendix). The patients were required to select the best answer for each of the 16 multiple-choice questions. Sections 2–4 focused on the patients’ knowledge of DM management when fasting during Ramadan. The questions were designed based on the recommendations made in the consensus statement by the American Diabetes Association for the management of DM during Ramadan (update 2010).(10) Section 2 had five questions assessing knowledge of the risks DM patients may face due to changes during Ramadan fasting (Appendix), Section 3 had 12 questions assessing knowledge of the symptoms and complications that DM patients may experience when fasting, and Section 4 had 11 questions assessing knowledge of safe practices and appropriate management of DM when fasting during Ramadan. The patients could answer ‘Yes’, ‘No’ or ‘Don’t know’ for each of these 28 questions. The maximum possible score for knowledge of DM (i.e. the cumulative score of the four sections) was 44. Questions on management of DM during the previous Ramadan were not scored.
The questionnaire was translated from English to Malay, and efforts were made to ensure that the translated version was semantically and conceptually close to the original questionnaire. The translation was done by a native speaker of Malay who was proficient in English. Another Malay native speaker reviewed the translated version and compared it with the original. The final version was completed and available for use after inconsistencies were resolved.
Data was analysed using IBM SPSS Statistics version 21.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used to describe patient demographics, disease characteristics and knowledge scores. Percentages and frequencies were used for the categorical variables, while mean and standard deviation were calculated for the continuous variables. Correlation analysis was performed to determine the correlation between the patients’ knowledge scores and their demographics, and between the patients’ knowledge scores and their DM characteristics (i.e. type and duration of DM, treatment received for DM and mean pre-Ramadan HbA1c level). Linear regression with a check for multicollinearity was performed. In the reliability analysis, internal consistency was assessed using Cronbach’s alpha coefficient; Pearson’s correlation or Spearman’s rank correlation was used to assess the test-retest reliability. The criterion for accepting Cronbach’s alpha was a score > 0.6.
RESULTS
A total of 92 patients (34 male, 58 female) were surveyed. The demographic characteristics of these patients and the type of DM treatment they received are shown in Table I. The mean age of the patients was 53.4 ± 13.3 years. Most of the patients were Malay (91.3%), while the remaining patients were Indian (8.7%). With regard to the education level of the patients, 66.3% had at least secondary school education, while 19.6% had lower than secondary education and 14.1% had no formal education. Most (59.8%) of the patients were working and 34.8% had a monthly household income < SGD 5,000, which is below the national average monthly household income (SGD 8,726 in 2011).(11)
Table I.
Demographic characteristics of the patients (n = 92) and the type of treatment they received for diabetes mellitus.
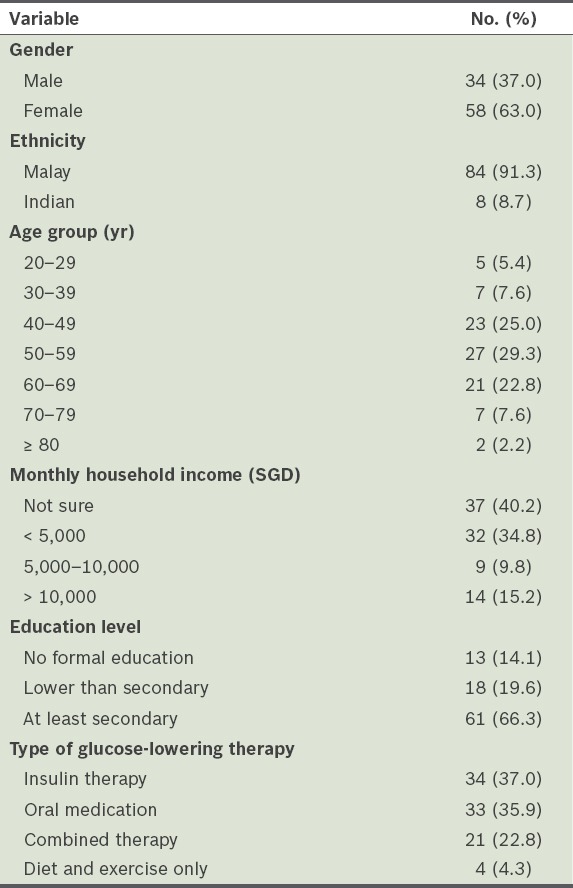
Among the 92 patients, 10 (10.9%) had Type 1 DM, while 82 (89.1%) had Type 2 DM. The mean duration of DM was 8.7 ± 5.1 years. In terms of DM treatment, 37.0% were on insulin therapy, 35.9% were on oral glucose-lowering drugs and 22.8% were on combined oral medication and insulin therapy; 13.0% incorporated lifestyle measures into their treatment regimen. Their mean pre-Ramadan HbA1c was 8.4% ± 1.8% (i.e. 68.3 mmol/mol).
Table II shows the overall test performance of the patients. The overall mean score was 71.3% ± 13.2%, with 8.7% scoring less than 50%. Performance was also analysed according to the four main sections of the test on DM knowledge: Section 1 on general knowledge of DM; Section 2 on knowledge of the risks DM patients may face due to changes during Ramadan fasting; Section 3 on knowledge of the symptoms and complications that DM patients may experience when fasting; and Section 4 on knowledge of the safe practices and appropriate management of DM when fasting during Ramadan.
Table II.
Patients’ performance in the knowledge test on diabetes mellitus (DM).
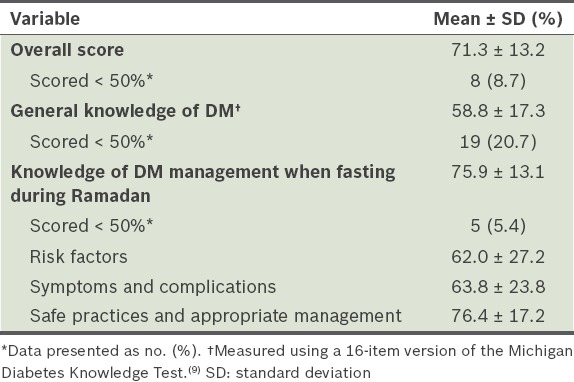
For the section assessing general knowledge of DM, the mean score was 58.8% ± 17.3%, with 20.7% of the patients scoring less than 50%. The patients scored well in the questions on glucose monitoring, the effect of exercise and infection on glucose levels, diabetic foot care, and associated DM complications. However, we observed important knowledge deficiencies regarding appropriate diet (Section 1, Appendix). Most of the patients had misconceptions about food groups and the effect of different food groups on blood glucose levels. They could not identify the fat content of food groups and the effect of unsweetened fruit juice on blood glucose level. More than 60% were unable to identify the food type that must not be used for treating hypoglycaemia. There were also deficiencies in their knowledge of sick day management. Although most of the patients were able to correctly identify the effect of infection on blood glucose levels, more than half did not recognise the need to monitor glucose levels more frequently during illness.
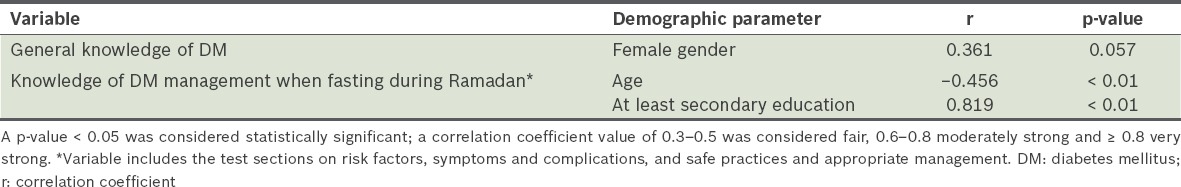
In terms of general knowledge about DM, the female patients appeared to have better scores than the male patients; there was fair correlation and a trend toward significance (r = 0.361, p = 0.057) (Table III). There were poor correlations between the patients’ overall knowledge of DM and their age, occupation, education level, type of DM, duration of DM, DM treatment and pre-Ramadan HbA1c level (i.e. no multicollinearity observed and tolerance measure > 0.6).
Table 3.
Correlation between the knowledge variables and various demographic parameters.
The mean score of the three sections that assessed knowledge of DM management when fasting during Ramadan was 75.9% ± 13.1%, with 5.4% of the patients scoring less than 50%. The patients performed well in the section on the risks that patients with DM may face due to changes during Ramadan fasting. However, the majority were unaware of the effect of daytime fasting on blood glucose level. This lack of awareness may explain the high rate of self-reported hypoglycaemia in the previous fasting month.
In Section 3, which involves symptoms and complications that patients with DM may experience when fasting, the patients showed good recognition of the symptoms of hyperglycaemia and hypoglycaemia. However, weight loss despite normal appetite was not well recognised as a symptom of hyperglycaemia, while tachycardia, confusion and inappropriate speech were not well recognised as a symptom of hypoglycaemia. More than 80% of the patients did not know about the increased risk of these complications during fasting. The fasting month of Ramadan was misconstrued as a period of better glycaemic control. The majority also did not recognise the increased risk of dehydration and thrombosis in DM patients of advanced age.
The subjects performed well in the section on safe practices and appropriate management of DM, which indicated that they were generally aware of the necessary safe practices to manage DM when fasting during Ramadan. However, more than 30% had the misconception that patients with DM should eat more starchy foods during meals in the fasting month. In addition, more than 40% were not aware that checking capillary blood glucose level did not constitute breaking fast.
We found that patients who were younger or had a higher education level (i.e. at least secondary school) scored better in the sections that assessed knowledge of DM management when fasting during Ramadan (Table III). There was a fair correlation for younger patients (Spearman’s rank correlation coefficient r = 0.456, p < 0.01). Patients with at least a secondary school education also appeared to have better scores, showing a very strong correlation on linear regression analysis (Pearson’s correlation coefficient r = 0.819, p < 0.01).
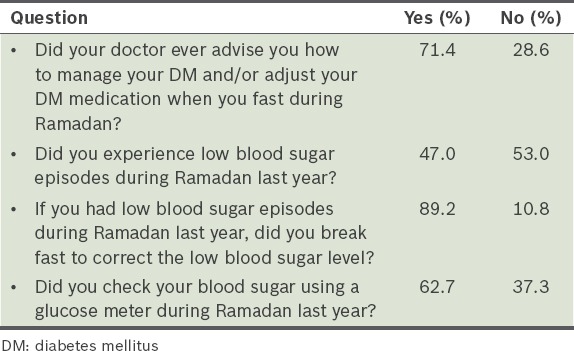
Table IV shows patients’ responses on how they managed their DM during the previous Ramadan, which was part of Section 4. The results revealed that only 71.4% consulted their physicians about DM management when fasting, although approximately 90% of the patients knew that this was necessary. A considerable proportion (47.0%) reported hypoglycaemic episodes, and of those who did, 10.8% did not treat the hypoglycaemia but continued to fast. More than a third of the patients (37.3%) reported that they did not monitor their capillary blood glucose levels during the previous fasting month.
Table IV.
Patients’ responses on management of DM during the previous Ramadan.
DISCUSSION
The Muslim patients with DM surveyed in the present study had an acceptable level of general knowledge of DM (mean score 58.8% ± 17.3%); only about one-fifth of the patients had scores that were lower than 50%. This may be due to the high level of literacy in our study population and the fact that the patients had been recruited from a tertiary centre, where they were likely to have received prior education on DM. The female patients appeared to have better scores than the male patients in the section on general knowledge of DM. This finding is similar to that of a study conducted by Al-Qazaz et al, in which the authors sought to validate a Malaysian version of the MDKT.(12) However, unlike that study, we found no correlation between the patients’ scores and their degree of glycaemic control (as measured by HbA1c).
There were important deficiencies in the patients’ general knowledge of DM in the present study, pertaining to diet, management of hypoglycaemia and sick day management. Understanding the effects of specific food groups on blood glucose level is essential for self-management of DM; a lack of understanding can impact patients’ long-term blood glucose control, as well as their glycaemic control during Ramadan fasting. Improper management of hypoglycaemic episodes can result in an increased risk of severe hypoglycaemia or rebound hyperglycaemia. Increased risk of severe hypoglycaemia resulting from hypoglycaemia unawareness can occur if the patient is unable to identify the symptoms of hypoglycaemia or if the symptoms are ignored and the hypoglycaemia is undertreated. On the other hand, the patient is at risk of rebound hyperglycaemia if the hypoglycaemia is over-treated. In a previous study by Wee et al, which was also conducted in Singapore, poor management of hypoglycaemia was observed among those patients who lacked knowledge of the need for standby hypoglycaemia treatment.(4) Knowledge of how to manage blood glucose levels during sick days is also crucial to prevent complications such as dehydration and hyperglycaemic crisis.
The patients in the present study had better knowledge concerning DM management when fasting during Ramadan (i.e. risks due to changes, potential symptoms and complications, and safe practices and appropriate management of DM) compared to their general knowledge of DM (75.9% ± 13.1% vs. 58.8% ± 17.3%). Only 5.4% of patients scored less than 50% on the DM management section. As Yaacob et al demonstrated in their study, the patients’ knowledge scores may be related to the absence or presence of prior health education.(7) However, despite these relatively good knowledge scores in DM management, there were some areas of deficiency. Among our patients, there was the misconception that glycaemic control is improved during fasting; some patients also failed to recognise that there is increased risk of complications (i.e. hypoglycaemia, hyperglycaemia and dehydration with thrombosis). These findings are similar to those of a study done by Gaborit et al in a different cultural setting (France), in which more than half of the patients carried on fasting against their doctors’ advice.(8)
The relationship between dietary control and glycaemic control during the fasting month is still poorly understood. The patients in the present study believed that eating foods with high starch content was necessary during meals at predawn and breaking of fast in order to sustain euglycaemia during the fasting hours. In the study by Gaborit et al, a considerable proportion of the patients did not consume the predawn meal prior to the start of the day’s fast, in addition to other factors such as sulphonylurea consumption and not seeking a medical consultation if unwell, which predisposed them to increased risk of hypoglycaemia.(8) However, we were unable to compare their findings with those of our cohort, as we did not obtain information on whether our study population consumed the predawn meal, the food content of the meal consumed and medication usage.
It was notable that there was an extremely high incidence of self-reported hypoglycaemic episodes during the previous fasting month. This may be caused by lack of consultation with primary care physicians, thus emphasising the need for Muslim patients with DM to seek medical consultation prior to fasting for Ramadan. One possible explanation for the lack of consultation is that primary care physicians may not be cognisant of the religious sensitivities of patients when discussing the religious practice of fasting, as cross-cultural and inter-religious barriers(8) are present in multicultural Singapore society. In comparison, there was a lower incidence of hypoglycaemia among the patients in Gaborit et al’s study, although many of them had a lower literacy level and were fasting against medical advice.(8) Another alarming fact was that a substantial proportion of the patients in the present study persisted with fasting even after they had identified that they were experiencing a hypoglycaemic episode. This is of concern, especially given the fact that more than one-third of the patients did not monitor their capillary glucose levels during fasting, even though the majority of them were aware of this need. Further studies are needed to examine the reasons for these harmful practices.
It is well recognised that patient education can empower DM patients in their self-care, resulting in improved blood glucose control.(13) The findings of the present study support the idea that future efforts should be targeted at improving patients’ general knowledge of DM, as well as their knowledge of DM management when fasting. While the results suggest that there are knowledge deficits and inappropriate practices among Muslim patients with DM, we did not find any correlation between knowledge level and glycaemic control. Nonetheless, it is important that efforts be made to educate the public on how to manage DM when fasting, in order to avert serious complications among DM patients who fast.
International recommendations for DM patients who fast during Ramadan include risk profiling, education on appropriate diet consumption, abstinence from excessive physical activity during fasting, regular blood glucose monitoring, and intervention with adjustment of medications.(10,14) Studies have shown that interventional education programmes, such as those used in the Ramadan Education and Awareness in Diabetes study and the Ramadan Prospective Diabetes Study,(15,16) were able to reduce the high complication rates that were observed during fasting (as demonstrated in the EPIDIAR study(3)). Other studies have also shown that there is a need for preparation (e.g. medication adjustment) prior to the month-long fast.(17) Structured education and interventional programmes, for both Muslim patients with DM and healthcare professionals involved in the care of these patients,(18-21) are important to bridge the knowledge gap and to correct inappropriate practices so that the complication rates observed among these patients during Ramadan can be reduced.
This study was not without limitations. We did not have data on whether the patients received prior education on DM (e.g. hypoglycaemia treatment and sick day management). Such data could have enabled us to identify the reason(s) for the patients’ misconceptions about the basic concepts of DM management; this would then help in the development of future patient education on DM. In addition, as this study involved retrospective data collection, there may have been recall bias when the patients reported the complications they encountered during fasting and self-adjustments for DM treatment. We also did not have information about the advice that the patients received on DM management when fasting. The type of advice given may have varied, depending on whether it was given by endocrinologists, primary care physicians or other specialists.
In conclusion, the present study revealed deficiencies in DM knowledge and inappropriate practices among Muslim patients with DM who fast during Ramadan. These may have a major impact on the incidence of DM-related complications, which can be magnified when patients fast during Ramadan. There is a need for a focused educational and interventional programme that encourages optimal patient care during this critical period. For example, a programme should be developed to educate both Muslim patients with DM and healthcare providers on how to manage potential complications during fasting. Future large-scale studies are also necessary to evaluate the effectiveness of current DM education and interventional programmes in reducing the rates of DM-related complications during fasting. The development of public health programmes that specifically address DM management when fasting is especially important in countries where a significant proportion of diabetic patients practise fasting during Ramadan. This is pertinent given the projected exponential increase in the global prevalence of DM.
ACKNOWLEDGEMENTS
We would like to thank Dr James Tom Fitzgerald for granting us permission to use and modify the Michigan Diabetes Knowledge Test. We would also like to extend our gratitude to the staff of the Diabetes Centre and Department of Endocrinology, Singapore General Hospital, Singapore, for their contributions to this study.
APPENDIX
Section 1.
General knowledge of diabetes mellitus (adapted from Fitzgerald et al).(5)
Section 2.
Knowledge of risk factors for diabetes mellitus during Ramadan.
REFERENCES
- 1.International Diabetes Federation. IDF Diabetes Atlas. 6th edition. [Accessed April 26 2017]. Available at: http://www.diabetesatlas.org/component/attachments/?task=download&id=76 .
- 2.Ministry of Health Singapore. National Health Survey 2010. [Accessed April 22 2015]. Available at: https://www.moh.gov.sg/content/moh_web/home/Publications/Reports/2011/national_health_survey2010.html .
- 3.Salti I, Bénard E, Detournay B, et al. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–11. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 4.Wee HL, Ho HK, Li SC. Public awareness of diabetes mellitus in Singapore. Singapore Med J. 2002;43:128–34. [PubMed] [Google Scholar]
- 5.Lee WR, Lim HS, Thai AC, et al. Diabcare Singapore Local Working Group & Diabetic Society of Singapore. A window on the current status of diabetes mellitus in Singapore--the Diabcare-Singapore 1998 study. Singapore Med J. 2001;42:501–7. [PubMed] [Google Scholar]
- 6.Tham KY, Ong JJ, Tan DK, How KY. How much do diabetic patients know about diabetes mellitus and its complications? Ann Acad Med Singapore. 2004;33:503–9. [PubMed] [Google Scholar]
- 7.Yaacob N, Ismail AA, Wan Bebakar WM. Knowledge, attitude and practice of type 2 diabetes mellitus patients on Ramadan fasting at Hospital Universiti Sains Malaysia. J IMA. 2007;39:6–12. [Google Scholar]
- 8.Gaborit B, Dutour O, Ronsin O, et al. Ramadan fasting with diabetes: an interview study of inpatients’ and general practitioners’ attitudes in the South of France. Diabetes Metab. 2011;37:395–402. doi: 10.1016/j.diabet.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21:706–10. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 10.Al-Arouj M, Assaad-Khalil S, Buse J, et al. Recommendations for management of diabetes during Ramadan: update 2010. Diabetes Care. 2010;33:1895–902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Statistics Singapore. Key Household Income Trends. 2014. [Accessed April 22 2015]. Available at: http://www.singstat.gov.sg/publications/publications-and-papers/population .
- 12.Al-Qazaz HK, Hassali MA, Shafie AA, Sulaiman SA, Sundram S. The 14-item Michigan Diabetes Knowledge Test: translation and validation study of the Malaysian version. Pract Diab Int. 2010;27:238–41a. doi: 10.1016/j.diabres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan AS, Yong LS, Wan S, Wong ML. Patient education in the management of diabetes mellitus. Singapore Med J. 1997;38:156–60. [PubMed] [Google Scholar]
- 14.Ibrahim M, Abu Al Magd M, Annabi FA, et al. Recommendations for management of diabetes during Ramadan: update 2015. BMJ Open Diabetes Res Care. 2015;3:e000108. doi: 10.1136/bmjdrc-2015-000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bravis V, Hui E, Salih S, et al. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with Type 2 diabetes who fast during Ramadan. Diabet Med. 2010;27:327–31. doi: 10.1111/j.1464-5491.2010.02948.x. [DOI] [PubMed] [Google Scholar]
- 16.Ahmedani MY, Haque MS, Basit A, Fawwad A, Alvi SF. Ramadan Prospective Diabetes Study: the role of drug dosage and timing alteration, active glucose monitoring and patient education. Diabet Med. 2012;29:709–15. doi: 10.1111/j.1464-5491.2011.03563.x. [DOI] [PubMed] [Google Scholar]
- 17.Gray LJ, Dales J, Brady EM, et al. Safety and effectiveness of non-insulin glucose-lowering agents in the treatment of people with type 2 diabetes who observe Ramadan: a systematic review and meta-analysis. Diabetes Obes Metab. 2015;17:639–48. doi: 10.1111/dom.12462. [DOI] [PubMed] [Google Scholar]
- 18.Wilbur K, Al Tawengi K, Remoden E. Diabetes patient management by pharmacists during Ramadan. BMC Health Serv Res. 2014;14:117. doi: 10.1186/1472-6963-14-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee JY, Lee SW, Nasir NH, et al. Diabetes telemonitoring reduces the risk of hypoglycaemia during Ramadan: a pilot randomized controlled study. Diabet Med. 2015;32:1658–61. doi: 10.1111/dme.12836. [DOI] [PubMed] [Google Scholar]
- 20.Hassan A, Meo SA, Usmani AM, Shaikh TJ. Diabetes during Ramadan - PRE-approach model: presentation, risk stratification, education. Eur Rev Med Pharmacol Sci. 2014;18:1798–805. [PubMed] [Google Scholar]
- 21.Hassan A, Meo SA. Diabetes during Ramadan: underestimated, under-investigated, needs more attention. Eur Rev Med Pharmacol Sci. 2014;18:3528–33. [PubMed] [Google Scholar]


