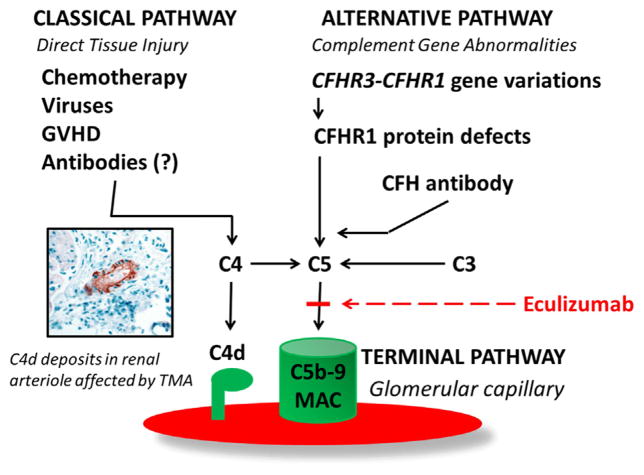
Figure 4.
Complement activation in pathogenesis of HSCT-TMA. Factors involved in classic and alternative pathway activation in patients with HSCT-TMA. The classic pathway can be activated by direct tissue injury from high-dose chemotherapy, viruses, and GVHD. C4d deposits, as the evidence of classic complement pathway activation, can be detected in renal arterioles of HSCT patients affected with TMA [12]. Alternative pathway dysregulation might present as a formation of the pathogenic autoantibody against complement factor H (CFH ab) due to either defects in CFHR3-CFHR1 genes associated with defective or absent CFHR1 protein or immune dysregulation after HSCT without genetic predisposition [11]. Dysregulation in either the classic or alternative pathway of complement results in terminal complement activation detected as elevated sC5b-9 (MAC) that can be blocked by eculizumab, which inhibits the cleavage of C5 to C5a and C5b by the C5 convertase, which prevents the generation of the terminal complement complex C5b-9 and tissue injury.