Abstract
Global smartphone penetration has led to unprecedented addictive behaviors. To develop a smartphone use/non-use pattern by mobile application (App) in order to identify problematic smartphone use, a total of 79 college students were monitored by the App for 1 month. The App-generated parameters included the daily use/non-use frequency, the total duration and the daily median of the duration per epoch. We introduced two other parameters, the root mean square of the successive differences (RMSSD) and the Similarity Index, in order to explore the similarity in use and non-use between participants. The non-use frequency, non-use duration and non-use-median parameters were able to significantly predict problematic smartphone use. A lower value for the RMSSD and Similarity Index, which represent a higher use/non-use similarity, were also associated with the problematic smartphone use. The use/non-use similarity is able to predict problematic smartphone use and reach beyond just determining whether a person shows excessive use.
Introduction
Global smartphone penetration has produced unprecedented social impacts and the overuse of smartphones can be considered to be one form of technological addiction.1 Griffiths operationally defined technological addiction as one type of behavioral addiction that involves human-machine interaction and is non-chemical in nature.2 Internet addiction was first researched by Young, and the study reviewed heavy Internet users with clinical signs of addiction as measured through adapted criteria for pathological gambling, the most well-studied type of behavioral addiction.3 Internet gaming disorder, has been listed in the research criteria of the current version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),4 and categorized in the ‘substance related and addictive disorders' section. The work group focused on gaming because it was the most well-studied and arguably problematic form of Internet use at the time.5
Identical to the components of all variants of Internet addictions,6 smartphone addiction/problematic smartphone use consists of four main components: compulsive behaviors; tolerance, withdrawal and functional impairment.1 Although smartphone gaming, regardless of multiple applications (Apps) use, increased the risk of problematic smartphone use,7 the preliminary diagnostic criteria for problematic smartphone use demonstrated that problematic smartphone use is similar to generalized Internet addiction, rather than to the more specific Internet gaming disorder as outlined in DSM-5.8 This is likely because smartphone use is characterized by the use of multiple Apps. Therefore, the addictive behavioral patterns, resulted from different devices to access Internet (for example, computer and smartphone), are as important as the addictive content (for example, gaming, social networking) for behavioral addiction researchers.
Problematic smartphone use was associated with irregular circadian rhythm,9 mental health problems9 and poor interpersonal relationship.10, 11 The core psychopathology of addiction is impaired control, which manifests as compulsive behaviors. Almost all questionnaires assessed problematic smartphone use presented with the typical compulsive behavior ‘although using smartphone has brought negative consequence, the amount of time spent on smartphone remains unreduced'.1, 12, 13, 14 Our previous study also described problematic smartphone use by the following compulsive symptom criteria for diagnostic interview; these were ‘smartphone use for a period longer than intended' ‘recurrent failure to resist the impulse to use' and ‘despite knowledge of having a persistent or recurrent physical or psychological problem'.8, 15 These compulsive behaviors are shared by individuals with substance use and gambling disorders.4
A mobile App is necessary to improve the accuracy of the assessment for problematic smartphone use because smartphone users can not accurately estimate their smartphone use.8, 16 Nowadays, the close interaction between humans and smartphones has enabled direct analyses of human behaviors on a large scale, in the finest temporal resolution by mobile Apps.17 Psychoinformatics, a novel application of computer science methods to psychology, has been established to study a range of psychological phenomena,18 such as personality traits19, 20, 21 and problematic smartphone use.8, 15, 16 In addition, the big data derived from smartphones overcomes the reliability limitation of traditional psychometric tests based on self-reports and interviews, which can result in memory and training effects in repeated measurements.17 Moreover, real-world data recorded by smartphone provide a better ecological validity, which is commonly lacking in laboratory experiments,22 especially when most confounding factors in the laboratory are excluded. Most importantly, most comparable sources of big data are scarce in undeveloped countries, but mobile phones are a notable exception. A recent study showed that the mobile phone metadata could predict the geographic distribution of poverty and wealth in an Africa country.23
We have developed an App to identify several addictive behavioral patterns; these included excessive frequent use (smartphone-use frequency>68.4 count per day), long daily use duration (total duration of smartphone use>4.62 h per day) and an increase use trend within one month (trend of the daily median use duration>0).8, 15 We also introduced App-generated parameters with the aim of assisting in the diagnosis of problematic smartphone use.15 In previous studies, we defined an epoch as a use that starts from screen-on and ends at screen-off. There are three fundamental App-generated parameters, use frequency, use duration and use-median. The daily epoch count (use frequency) and the total daily epoch time (use duration) are obtained from the data. The median duration per epoch per day (use-median) is used as a representative for the average epoch within a day.8, 15 Although excessive use is an important criterion in substance addiction4 and time spent on online-gaming is correlated with the severity of Internet addiction,24 it remains a fact that compulsive behavior that is based on impaired control remains the fundamental criteria when diagnosing addiction. Thus, more representative indicators of impaired control than just excessive use not only allow a more accurate diagnosis, but also have the potential to distinguish behavior or substance addiction from normal use. In this study, we aim to expand the App-generated parameters based on epochs of smartphone use to non-use epochs. We also introduce two parameters to quantify the reciprocity between smartphone use and non-use (use/non-use reciprocity), which indicates impaired control for smartphone use. The definitions of all App-generated parameters are listed in Table 1.
Table 1. The App-generated parameters in this study.
| Smartphone use parameters | Smartphone non-use parameters |
| Smartphone use epoch: an epoch as a smartphone use that starts from screen-on and ends at screen-off. | Smartphone non-use epoch: in contrast to smartphone use epoch, an epoch as a smartphone non-use that starts from screen-off and ends at screen-on. |
| Use-frequency: the daily epoch count of smartphone use. | Non-use frequency: the daily epoch count of smartphone non-use. |
| Use-duration: The total daily epoch time of smartphone use. | Non-use duration: the total daily epoch time of smartphone non-use. |
| Use-median: The median duration per epoch per day. | Non-use-median: the median duration per non-use epoch per day. |
| Use/non-use reciprocity | |
| Root mean square of the successive differences (RMSSD): root mean square of the differences between the adjacent duration of use and non-use epochs | |
| Similarity Index: differences between the duration of one non-use epoch and the corresponding three successive use epochs | |
The two specific aims of this study are (1) to develop parameters needed to assess use/non-use reciprocity (use/non-use parameters), and (2) to examine the predictive ability of smartphone use, non-use and use/non-use parameters when making a problematic smartphone use diagnosis. We hypothesized that use/non-use parameters, which are similar to compulsive behaviors, should be able to predict problematic smartphone use, as well as any excessive smartphone use.
Materials and methods
Participants
In total, 79 young adults were recruited from the Department of Electrical Engineering and Department of Computer and Communication Engineering of two universities in northern Taiwan between December 2013 and May 2014. There were 57 males and 22 females, who were aged 22.4 years old on average. The recruitment strategy was based on the potentially high popularity of smartphone use among these students. All participants in this study used a smartphone with an Android operation system. A newly developed App created by our team8, 15 was installed on their smartphones to record their smartphone use for at least 3 weeks. After the researchers had checked the App data, the participants were interviewed by psychiatrists. We investigated the same sample of participants to compare the association between problematic smartphone-use diagnoses and different App-generated parameters, namely use/non-use parameters in the present study versus excessive use parameters in our previous study.8 The study was approved by the Institutional Review Board of National Taiwan University. All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki.
The App-generated parameters
Smartphone-use parameters
Smartphone use from screen-on to the successive screen-off was defined as one epoch of use. This App calculated the average daily epoch count for one month as the use frequency parameter. Similarly, the average daily epoch length and the average daily median epoch duration were calculated as the use duration and use-median parameters, respectively. As the epoch duration for each day did not follow a normal distribution, we preferred to use the median duration, rather than the mean duration, in order to represent the average epoch duration.
Smartphone non-use parameters
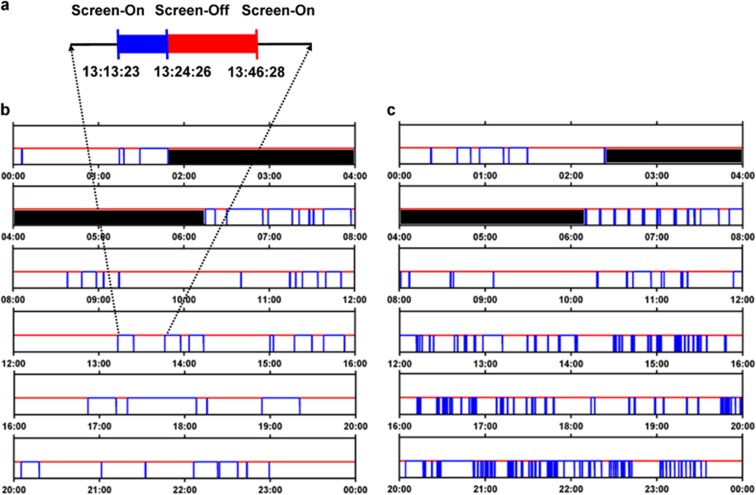
As a reciprocal to the smartphone-use parameters, the event from screen-off to screen-on was defined as one epoch of non-use. Defined as the maximal non-use epoch between 2100 hours and next noon (1200 hours), sleeping time was excluded from the non-use epoch. In addition, we also confirmed that no participant was a shift worker. Thus, the sum of total duration of use, total duration of non-use and sleep time totals exactly 24 h. We used a similar definition of use parameters to calculate the average daily non-use frequency, non-use duration and non-use-median parameters (Figure 1).
Figure 1.
The raw data of smartphone use for one day. (a) The blue highlighting indicates a use epoch, which starts with the screen-on (from 13:13:23) and ends with the screen-off (13:24:26). The duration of this use epoch is 663 s. The red highlighting indicates an adjacent non-use epoch, which starts with the screen-off (from 13:24:26) and ends with the screen-on (13:46:28). The duration of this non-use epoch is 1322 s. (b) One-day of raw data obtained from a non-addictive subject as identified by the psychiatrist: First, we excluded the non-use epoch associated with sleep time. The black epoch is the sleep time, which starts with the screen-off (from 01:48:41) and ends with the screen-on (06:15:00). After this exclusion, there are 35 non-use epochs in this day (non-use frequency=35) with the total duration of the 35 non-use epochs being 48 527 s. Among the 35 non-use epochs, the epoch with the median duration is magnified in (A), that is, the non-use-median duration is 1322 s. (c) The non-use frequency of an addictive subject who has a non-use frequency of 231, a non-use duration of 55 557 s and a non-use-median of 304 s. Similar to the non-addictive subject, we have excluded the black epoch of sleep time, which starts with the screen-off (from 02:23:46) and ends with the screen-on (06:10:00).
Use/non-use reciprocity
The time series of the use and non-use epochs occur in turn. We introduced two parameters – Root Mean Square of the Successive Differences (RMSSD) and Similarity Index—in order to assess the reciprocity between the use and non-use patterns. We calculated the RMSSD and Similarity Index within a day, and apply the average daily RMSSD and Similarity Index in order to predict problematic smartphone use.
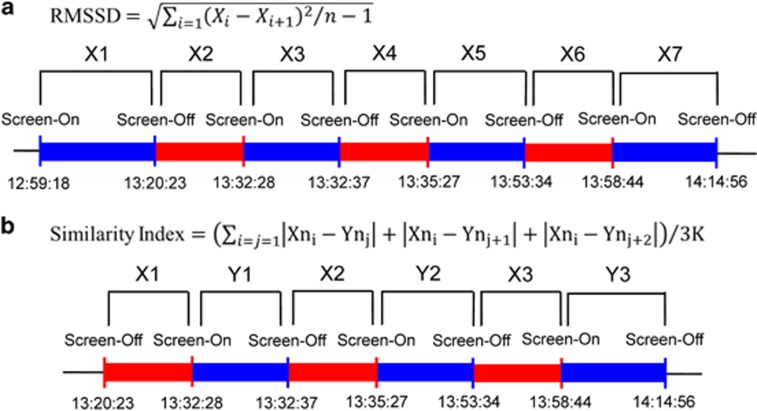
Figure 2a shows the algorithm of the RMSSD. First, we calculated the difference between the adjacent duration of use (Xi) and non-use epochs (Xi+1). Next, each use/non-use difference was passed through a sum of the squares and divided by (n−1) number of epochs. Finally, the RMSSD was calculated to be the square root of the mean square, mathematically expressed as
Figure 2.
Use/non-use reciprocity parameters. (a) A schematic and the equation used to calculate the root mean square of the successive differences (RMSSD). X(i) is the duration of a use or non-use epoch. There are (n−1) successive differences of use/non-use epochs. (b) A schematic and the equation used to calculate the Similarity Index, Xn(i) refers to the duration of a non-use (red) epoch, Yn(j) refers to the duration of a use (blue) epoch. Each non-use epoch (Xni) corresponds to three successive use epochs (Ynj, Ynj+1, Ynj+2). K is the number of non-use epochs in a day. Thus, the similarity index is the average absolute difference between the non-use and use epochs.
Figure 2b shows the algorithm used for the Similarity Index. We calculated the absolute differences between one non-use epoch (Xni) and the corresponding three successive use epochs (Ynj, Ynj+1, Ynj+2). Next the Similarity Index was calculated to be the average of the absolute differences within a day, which can mathematically expressed as
where K was the total number of non-use epoch.
Diagnosis of problematic smartphone use
Three qualified psychiatrists interviewed all participants and they then determined whether individual participant were smartphone addicts or non-addicts using specific diagnostic criteria. The criteria consisted of three parts: criteria A; B; and C. Criterion A consisted of the eight characteristic symptoms of problematic smartphone use, Criterion B described the functional impairment that is secondary to smartphone use or that causes marked distress and Criterion C excluded the addictive behaviors accounted for obsessive-compulsive disorder or bipolar I disorders. Smartphone addicts were individuals who presented with three or more symptoms in criterion A, and met the functional impairment criterion.8 In total, 31 participants were diagnosed as having problematic smartphone use (the addictive group) and 48 were found not to have problematic smartphone use (the non-addictive group).
We also used the App-generated parameters to assist with diagnosis. All criteria were assessed in two ways: (1) using both the App-generated parameters and the psychiatrists' diagnostic interviews for the diagnosis and (2) using solely the psychiatrists' diagnostic interviews for the diagnosis. Using the App-assisted diagnosis (diagnosis based on criteria assessed in the first way), two criteria, excessive use and tolerance, were determined by the App-generated parameters instead of the psychiatrists' interviews. On the basis of our previous findings,1 excessive use was defined as a use frequency parameter >68.4 counts per day, and the tolerance was defined as a use-medium-trend parameter greater than zero. In addition, psychiatrists were provided with information on the extent of the participants' underestimation of their smartphone-use duration ΔD (that is, the difference of self-estimated duration, Dself, and App-recorded duration, DApp).8 According to the App-assisted diagnosis, a total of 27 participants were diagnosed as having problematic smartphone use (the addictive group) and 52 were found not to have problematic smartphone use (the non-addictive group).
Our previous findings showed that both App-assisted diagnosis and solely interview diagnosis (diagnosis based on criteria assessed in the second way) presented with good inter-rater reliability. The agreement between the App-assisted and solely interview diagnoses was 91.1%.15
The prediction ability of the App-generated parameters when making a problematic smartphone use diagnosis
We used two definitions of problematic smartphone-use diagnosis (the solely interview diagnosis and the App-assisted diagnosis) as the gold standards in order to examine the ability to predict problematic smartphone-use diagnosis based on eight App-generated parameters, namely use frequency, use duration, and use-median, non-use frequency, non-use duration and non-use-median, as well as the RMSSD and Similarity Index.
The use frequency, use duration and use-median parameters predicted problematic smartphone use. The use frequency and non-use frequency are reciprocally identical and therefore the non-use frequency also is able to predict problematic smartphone use. In contrast, the non-use duration and non-use-median parameters predict non-addiction. We hypothesize that a lower variability of use/non-use is associated with problematic smartphone use. The RMSSD and Similarity Index predicted non-addiction.
Statistically, the two previous definitions of ‘problematic smartphone use' are binary variables, while the App-generated parameters are continuous variables. Therefore, we have presented the point estimates with a 95% confidence interval (CI) of the area under the curve (AUC) of receiver operating characteristic. The App-generated parameters with an AUC >0.5 imply the potential ability to diagnose problematic smartphone use. In order to test the hypothesis, the significantly level was set to 0.05.
Results
Table 2 shows the AUC for the App-generated parameters. All non-use parameters (non-use frequency, non-use duration and non-use-median) are significantly associated with both types of problematic smartphone-use diagnosis. Whereas, the use duration and use-median parameter only are able to predict the App-assisted diagnosis. The AUC of the App-generated parameters for the App-assisted diagnosis were all higher than the AUC for the diagnostic interview alone. The AUCs of all the App-generated parameters, except the use-median parameter, were >0.70 for the App-assisted diagnosis (Supplementary Table).
Table 2. Area under the ROC curve analysis of the App-generated parameters used for problematic smartphone-use diagnosis.
| App-generated parameters | Diagnostic interview AUC (95% CI) | P-value | App-assisted diagnosis AUC (95% CI) | P-value |
|---|---|---|---|---|
| Non-use frequency | 0.632 (0.505–0.760)* | 0.048 | 0.704 (0.577–0.830)* | 0.003 |
| Non-use duration | 0.634 (0.511–0.758)* | 0.045 | 0.705 (0.591–0.819)* | 0.003 |
| Non-use-median | 0.656 (0.533–0.778)* | 0.020 | 0.707 (0.587–0.828)* | 0.002 |
| RMSSD | 0.648 (0.523–0.773)* | 0.027 | 0.721 (0.597–0.848)* | 0.001 |
| Similarity Index | 0.653 (0.530–0.777)* | 0.022 | 0.734 (0.617–0.851)* | 0.001 |
Abbreviations: AUC, area under the curve; CI, confidence interval; RMSSD, root mean square of the successive differences; ROC, receiver operating characteristic.
*P-value<0.05
Table 3 shows the cutoff points for the non-use and use/non-use parameters that maximize the sum of sensitivity and specificity. The non-use frequency and non-use-median parameters provide higher sensitivity than specificity. In contrast, the non-use duration parameters, RMSSD and Similar Index provide higher specificity than sensitivity.
Table 3. The cutoff point for the parameters that maximizes the sum of sensitivity and specificity.
|
Diagnostic interview |
App-assisted diagnosis |
|||||
|---|---|---|---|---|---|---|
| Cutoff point | Sensitivity | Specificity | Cutoff point | Sensitivity | Specificity | |
| Non-use frequency | 58.5 count per day | 0.710 | 0.604 | 67.4 count per day | 0.750 | 0.686 |
| Non-use duration | 52618.8 s per day | 0.608 | 0.786 | 54801.8 s per day | 0.479 | 0.839 |
| Non-use-median | 404.4 s per day | 0.725 | 0.643 | 415.9 s per day | 0.667 | 0.613 |
| RMSSD | 3498.2 s per day | 0.647 | 0.786 | 3783.5 s per day | 0.521 | 0.774 |
| Similarity Index | 857.5 s per day | 0.625 | 0.677 | 857.5 s per day | 0.667 | 0.786 |
Abbreviations: RMSSD, root mean square of the successive differences.
Discussion
To our knowledge, this is the first study to propose a sophisticated approach to the analysis of use/non-use patterns in order to delineate addictive behavior. Instead of the excessive smartphone-use patterns identified by Apps in previous studies,8, 15, 16 the use/non-use patterns are better to track the problematic smartphone use because this approach avoid time distortion effects on smartphone-use estimation.8, 16 Similar to the smartphone addicts lacked skills in structuring their daily routines,9 the use/non-use parameters indicated the extent of impaired control of smartphone use in the present study. The use/non-use patterns avoid overpathologizing the excessive smartphone use based on the duration of smartphone use. Smartphone use, unlike substance use, is not a problematic behavior in and of itself. Instead, smartphone has been widely engaged in our work, education and social relationship, and improved our quality of life. The high smartphone usage time might be normal functional use of the equipment. Therefore, we apply strict approaches to assess problematic smartphone use in the diagnostic interview—functional impairment is the necessary criterion when the psychiatrists diagnosed a participant with problematic smartphone use in this study. The use/non-use patterns were able to predict this diagnosis of problematic smartphone use.
Our findings provide evidence to support our previous study, which showed that the App-generated parameters were more associated with the App-assisted diagnosis than with the diagnostic interview alone.15 This study also examined three App-generated parameters related to smartphone use and non-use, the Frequency, Duration and Median parameters, which are the same as in previous study.8 The frequency of use and non-use gave rise to identical prediction in relation to problematic smartphone-use diagnosis because the non-use frequency is in reality equivalent to the use frequency. There is a ‘sleep time' gap between non-use duration and 24 h minus use duration. The predictions based on use and non-use duration in terms of problematic smartphone-use are similar. Nevertheless, the non-use duration was able to predict both types of diagnosis, namely by interview and App-assisted assessment, whereas the use duration was only able to predict the App-assisted diagnosis at an acceptable level of significance. The ‘time distortion' effect dampened the role of use time in the diagnosis of problematic smartphone-use solely by interview.8 The App-assisted diagnosis compensated for the time distortion effect and as a result both the use and non-use duration were able to predict the outlined definition of problematic smartphone use similarly.
There are several implications of our findings related to the fact that the non-use-median parameter shows superior predictive ability with respect to problematic smartphone use than the use-median and this is quite different from the similar predictive ability found for frequency and duration between use and non-use. Therefore, first, it should be noted that the non-use-median is a representative interval that starts from the end of a use epoch to continue until the next use epoch in a day. This interval indicates an intensity of the urge to use the smartphone during the non-use condition. We interpret the non-use-median parameters as a use/non-use index rather than as merely non-use parameter. This implies that the non-use-median corresponds to craving symptom in addiction. Second, based on the above the cutoff point of the non-use-median at 6.7 min (404.4 s) or 6.9 min (404.4 s) is likely to have clinical significance. The families and therapists of smartphone addicts can, based on this, remind the addict to delay their craving to use their smartphone from the end of the last use for more than the cutoff point, for example 7 min. Furthermore, it should be possible to apply the non-use-median parameter as an indicator of relapse. Third, any smartphone use epoch is recoded as screen-on to screen-off by the App; however, the App is unable to distinguish between proactive and reactive use. In this context, proactive use is relevant to the addictive behavior, whereas reactive use should be treated more like ‘signal noise' in this analysis. Thus, non-use epochs, which will have less noise from reactive use, are more appropriate when predicting addiction than use epochs.
RMSSD has been well-established as part of heart rate variability analysis.24 A lower RMSSD indicates a lower variability and a higher similarity. When there is a craving to use a smartphone, non-use is followed by a proportional amount of smartphone use. These behaviors manifested themselves both as the reciprocity with respect to use/non-use and as a low variability of successive use/non-use, which corresponds to the RMSSD in the present study. RMSSD delineates only the reciprocity of the adjacent use and non-use epochs and as a result we have proposed an additional novel parameter, the Similarity Index. This is able to demonstrate a more generalized form of use/non-use reciprocity. The Similarity Index investigates the craving to use the smartphone by assessing the reciprocity of a non-use epoch with its successive three use epochs. Problematic smartphone use is different from the craving to use the Internet or when there is substance use, this is because there is relatively limited accessibility to the craved entity in the latter two cases compared with a smartphone, which is available almost all the time. The portability of smartphones, which makes them readily available, is likely to result in a craving for smartphone use during the non-use epoch being distributed over successive use epochs. More specifically, it becomes more appropriate to examine more than one use epoch corresponding to a given non-use epoch when examining the characteristics of frequent and short period smartphone use. Overall, the comparatively high predictive natures of RMSSD and the Similarity Index imply that use/non-use reciprocity is validated with respect to the compulsive symptoms of problematic smartphone use. Despite the parameters of use, non-use and use/non-use showing similar levels of prediction with respect to the App-assisted diagnosis, the good predictive ability of use/non-use with respect to the diagnostic interview remains noteworthy because most of the criteria used for the App-assisted diagnosis were originally based on the diagnostic interview.
There are several methodological limitations that should be noted when interpreting our findings. First, smartphone use and non-use were defined in this study by screen-on and screen-off. This definition cannot completely represent the status of smartphone use. Second, we did not actually exclude sleeping time in the present study. Instead, we excluded the relative long time of non-use that surrounds midnight, which ought to simultaneously exclude the non-use period around actual sleep time. Third, we did not differentiate proactive and reactive smartphone use, which may have resulted in the non-use parameters being more accurate when predicting problematic smartphone use than the use parameters. Fourth, 34.2% (according to App-assisted diagnosis) to 39.2% (according to diagnostic interview) of our participants would be evaluated as having problematic smartphone use. These results did not indicate that over 30% of healthy college students are likely to have problematic smartphone use because our participants were selected from a potentially high-risk group in order to validate the App-generated parameters. Finally, the sample contained only college students, which limits the ability to generalize our findings to other groups of smartphone users.
In conclusion, use/non-use reciprocity, including the Non-Use Median of, RMSSD and the Similarity Index, which correspond to the compulsive symptoms, are able to predict problematic smartphone use; this extends our ability to identify smartphone addictive behavior beyond merely assessing excessive use of a smartphone.
Acknowledgments
We thank Professor Norden E. Huang of the Research Center for Adaptive Data Analysis of National Central University of Taiwan for the numerous occasions when technical support was provided. TBJ Kuo was supported by a grant (YM-103AC-B3) from the Ministry of Education, Aim for the Top University Plan and grant (NSC 100-2627-B-010-002) from National Science Council, Taiwan. We thank the Ministry of Science and Technology their support of the Center for Dynamical Biomarkers and Translational Medicine, National Central University, Taiwan (MOST 103-2911-I-008-001). We also thank Dr. Tzu-Ting Chen for providing excellent technical assistance.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
The authors declare no conflict of interest.
Supplementary Material
References
- Lin YH, Chang LR, Lee YH, Tseng HW, Kuo TB, Chen SH. Development and validation of the Smartphone Addiction Inventory (SPAI). PLoS ONE 2014; 9: e98312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths MD. Gambling on the Internet: a brief note. J Gambl Stud 1996; 12: 471–473. [DOI] [PubMed] [Google Scholar]
- Young KS. Psychology of computer use: XL. Addictive use of the Internet: A case that breaks the stereotype. Psychol Rep 1996; 79: 899–902. [DOI] [PubMed] [Google Scholar]
- American Psychiatric AssociationAmerican Psychiatric Association DSM-5 Task Force Diagnostic and statistical manual of mental disorders: DSM-5. 5th edn, American Psychiatric Association: Washington, DC, 2013. [Google Scholar]
- Petry NM, O'Brien CP. Internet gaming disorder and the DSM-5. Addiction 2013; 108: 1186–1187. [DOI] [PubMed] [Google Scholar]
- Block JJ. Issues for DSM-V: Internet addiction. Am J Psychiatry. 2008; 165: 306–307. [DOI] [PubMed] [Google Scholar]
- Liu CH, Lin SH, Pan YC, Lin YH. Smartphone online gaming and frequent use pattern associated with smartphone addiction in high school students. Medicine 2016; 95: e4068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YH, Lin YC, Lee YH, Lin PH, Lin SH, Chang LR et al. Time distortion associated with smartphone addiction: Identifying smartphone addiction via a mobile application (App). J Psychiatr Res. 2015; 65: 139–145. [DOI] [PubMed] [Google Scholar]
- Montag C, Kannen C, Lachmann B, Sariyska R, Duke É, Reuter M et al. The importance of analogue zeitgebers to reduce digital addictive tendencies in the 21st century. Addict Behav Rep 2015; 2: 23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi HS, Lee HK, Ha JC. The influence of smartphone addiction on mental health, campus life and personal relations-Focusing on K university students. J Korean Data Information Sci Soc 2012; 23: 1005–1010. [Google Scholar]
- Park SJ, Kwon MA, Baek MJ, Han NR. Relation between smartphone addiction and interpersonal competence of college students using social network service. J Korea Contents Assoc 2014; 14: 289–297. [Google Scholar]
- Kwon M, Lee JY, Won WY, Park JW, Min JA, Hahn C et al. Development and validation of a smartphone addiction scale (SAS). PLoS ONE 2013; 8: e56936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon M, Kim DJ, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS ONE 2013; 8: e83558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Lee Y, Lee J, Nam JK, Chung Y. Development of Korean Smartphone addiction proneness scale for youth. PLoS ONE 2014; 9: e97920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YH, Lin PH, Chiang CL, Lee YH, Yang CC, Kuo TB et al. Incorporation of mobile application (App) measures into the diagnosis of smartphone addiction. J Clin Psychiatry. in press. [DOI] [PubMed]
- Montag C, Blaszkiewicz K, Lachmann B, Sariyska R, Andone I, Trendafilov B et al. Recorded behavior as a valuable resource for diagnostics in mobile phone addiction: evidence from psychoinformatics. Behav Sci (Basel) 2015; 5: 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowetz A, Blaszkiewicz K, Montag C, Switala C, Schlaepfer TE. Psycho-informatics Big Data shaping modern psychometrics. Med hypotheses 2014; 82: 405–411. [DOI] [PubMed] [Google Scholar]
- Yarkoni T. Psychoinformatics: new horizons at the interface of the psychological and computing sciences. Curr Dir Psychol Sci 2012; 21: 391–397. [Google Scholar]
- Montag C, Blaszkiewicz K, Sariyska R, Lachmann B, Andone I, Trendafilov B et al. Smartphone usage in the 21st century: who is active on WhatsApp? BMC Res Notes 2015; 8: 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag C, Błaszkiewicz K, Lachmann B, Andone I, Sariyska R, Trendafilov B et al. Correlating personality and actual phone usage: evidence from psychoinformatics. J Ind Diff 2014; 3: 158–165. [Google Scholar]
- Chittaranjan G, Blom J, Gatica-Perez D. Mining large-scale smartphone data for personality studies. Pers Ubiquit Comput 2013; 17: 433–450. [Google Scholar]
- Montag C, Reuter M, Markowetz A. The impact of psychoinformatics on internet addiction In: Montag C, Reuter M (eds) Internet Addiction—Neuroscientific Approaches and Therapeutical Interventions. Springer: Switzerland, 2015. pp 143–150. [Google Scholar]
- Blumenstock J, Cadamuro G, On R. Predicting poverty and wealth from mobile phone metadata. Science 2015; 350: 1073–1076. [DOI] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996; 93: 1043–1065. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.