Abstract
As our knowledge and technology advance, the indications for elbow arthroscopy continue to grow rapidly. During this expansion, a number of new portals have been described and reported using variable nomenclature and location descriptions. Accordingly, a comprehensive review of these portals is warranted. Given the concern for potential iatrogenic injury to surrounding neurovascular structures, a discussion of these critical nerves and vessels is also timely. In this work, we review pertinent surface anatomy; portal nomenclature, locations, and utility; and review distances to the nearest structures at risk.
Since its initial description in the 1980s, the field of elbow arthroscopy has evolved rapidly.1, 2, 3 Significant advances in arthroscopic technology and equipment have significantly contributed to this growth, and our ever-expanding knowledge of the complex anatomy of the elbow joint and its surrounding structures has permitted what was once considered to be an unsafe procedure to evolve into a reliable treatment option for a number of elbow pathologies.4, 5 Initially used primarily as a diagnostic tool, elbow arthroscopy is now routinely used to treat loose bodies, osteochondral injury, lateral epicondylitis, plicae, valgus extension overload, hypertrophic osteoarthritis, contracture, septic arthritis, synovial proliferative disorders, and select fractures.
Despite these advances, elbow arthroscopy is not without risks and limitations. These are due, in large part, to the fact that the elbow is a complex trochoginglymoid joint closely surrounded by important neurovascular structures including the medial, ulnar, and radial nerves as well as the brachial artery.6 Although these critical structures do not preclude intra-articular access to the elbow, surgeons must be aware of their locations and make every effort to protect them throughout the procedure. A number of portals have been developed that allow surgeons to safely access the joint while minimizing the risk of injury to surrounding neurovascular structures. In the orthopaedic literature, these portals have been described with variable nomenclature and locations. The purpose of this technical note is to provide descriptive and video (Video 1) demonstration of key surface anatomic landmarks, clarify the terminology and locations of the most commonly used portals, and highlight critical neurovascular structures of the elbow. This technical note is Part I in a 3-part series on the Basics of Elbow Arthroscopy. Subsequent parts address setup, patient positioning, and diagnostic arthroscopy in the supine (Part II) and laterally (Part III) positioned patients.
Technique
Anatomic Landmarks
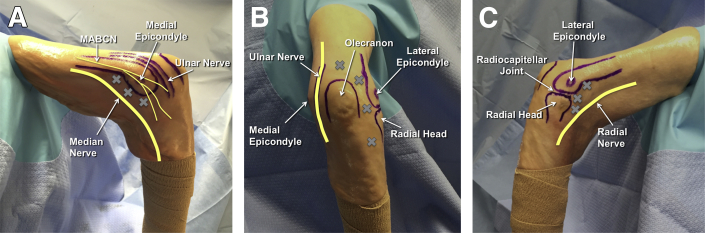
Regardless of how the patient is positioned, there are a few key landmarks that should be identified on all patients before beginning the procedure. These landmarks orient the surgeon, assist with portal localization, and help elucidate the locations of important neurovascular structures. On patients of nearly any size and habitus, the olecranon, medial epicondyle (ME), and lateral epicondyle (LE) can generally be identified with relative ease (Fig 1). For most patients, the radiocapitellar joint can be palpated while pronating and supinating the forearm. Where possible, the ulnar nerve and medial intermuscular septum should also be identified and labeled.
Fig 1.
Key anatomic landmarks and surface anatomy are highlighted on a right elbow in the lateral decubitus position. (A) On the medial side, the medial epicondyle, ulnar nerve, and medial intermuscular septum should be identified. (B) When viewing the posterior aspect of the elbow, the olecranon process is easily visible. (C) Laterally, the lateral epicondyle, capitellum, radial head, and soft spot should be identified. (MABCN, medial antebrachial cutaneous nerve.)
Portals
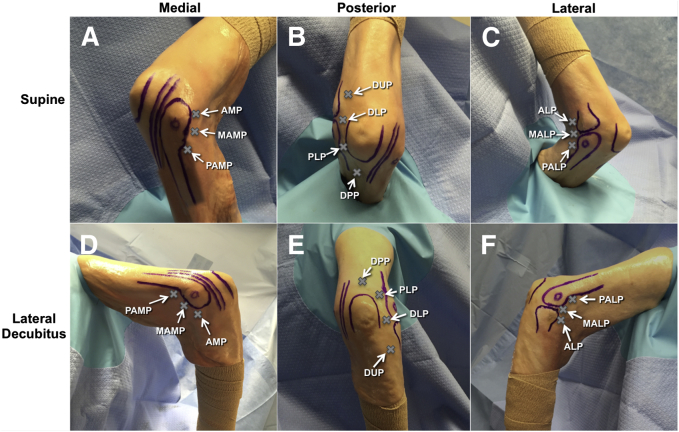
In the current literature, a multitude of portals have been described; however, the naming and description is often redundant and complex. Here, we will strive to describe the most commonly reported portals using the most commonly accepted nomenclature. Generally speaking, there are 3 portals used to access the anterior joint from the medial side (Fig 2 A and D) and 3 to access the anterior joint from the lateral side (Fig 2 C and F). There are an additional 4 described portals used to access the posterior aspect of the elbow joint (Fig 2 B and E). More commonly, the anterior portals lie in closer proximity to neurovascular structures. In addition to having an intimate knowledge of these structures, there are a few strategies that can be taken to reduce the risk of injury by increasing the anterior joint space and improve capsular distension during anterior portal creation. These techniques include proper positioning of the arm (either in the supine or lateral decubitus position) so that gravity retracts the anterior elbow structures away from the joint, flexing the elbow to reduce anterior tissue tension, and joint insufflation with saline before portal placement.
Fig 2.
On this right elbow, the most commonly used portals for elbow arthroscopy are detailed in reference to important surrounding anatomic structures in both the supine (A-C) and lateral decubitus (D-F) positions. (A, D) From the medial side, the anteromedial portal (AMP), mid-anteromedial portal (MAMP), and proximal anteromedial portal (PAMP) can provide access to the anterior elbow. (B, E) To access the posterior elbow, the direct posterior portal (DPP), posterolateral portal (PLP), direct lateral portal (DLP), and distal ulnar portals (DUP) can be used. (C, F) Finally, the anterolateral portal (ALP), mid-anterolateral portal (MALP), and proximal anterolateral portal (PALP) can be used to access the anterior elbow joint from the lateral side.
Accessing the Anterior Elbow: Medial Side
Anteromedial Portal
This portal has been described as being 2 cm anterior and 2 cm distal to the ME.2, 4, 5 The anteromedial portal is placed through the flexor pronator musculature and can be relatively close to the median and medial antebrachial cutaneous nerves (MABCN). Accordingly, this portal is often created by needle localization while viewing from the lateral side. The median nerve has been reported to travel as close as a mean distance of 5.0 to 7.0 mm from this portal,7, 8, 9 but other studies found the mean distance as high as 12.0 mm.10 The MABCN is approximately 1.0 to 8.9 mm away,8, 10 whereas the mean distance to the brachial artery ranges from 15.2 to 16.6 mm (Fig 2 A and D).8, 10
Mid-anteromedial Portal
This portal is located 1 cm proximal and 1 cm anterior to the ME. Given its close proximity to the anteromedial portal and proximal anteromedial portal (PAMP), it is rarely used. It is approximately 13.8 mm from the median nerve, 17.6 mm from the brachial artery, and 7.0 mm from the MABCN.10
Proximal Anteromedial Portal
Also referred to as the “proximal medial”5 or “anteromedial accessory”4 portal, the PAMP is located 2 cm proximal to the ME and immediately anterior to the intermuscular septum.11 The PAMP is the most commonly used medial portal and it functions well as a working portal or a retraction portal. When creating the PAMP, the trocar should pass anterior to the intermuscular septum but penetrate the capsule while aiming posterior and distal toward the coronoid fossa. The median nerve and brachial artery are approximately 12.4 and 18.0 mm away, respectively.10
Accessing the Anterior Elbow: Lateral Side
Anterolateral Portal
Although initially described as the “standard anterolateral” or simply the “anterolateral” portal,2 this portal is now often referred to as the distal anterolateral portal (DALP).12 It is located 3 cm distal and 1 cm anterior to the LE just anterior to the radial neck and head. Although it was one of the first described lateral access points,2 it has since fallen out of favor due to its close proximity to the radial nerve. The mean distance of the DALP to the radial nerve has been reported from 4.0 to 7.2 mm.7, 8, 9, 10, 12 The posterior antebrachial cutaneous nerve is approximately 7.6 to 12.6 mm away.8, 10 To avoid this risk of injury, many surgeons advocate moving this portal more proximal. Although they often continue to refer to it as the DALP or “anterolateral portal,” if moved proximal enough that it is anterior to the radiocapitellar joint or the ME, then it is more aptly described as the mid-anterolateral portal (MALP) (Fig 2 C and F).12
Mid-anterolateral Portal
Located directly anterior to the radiocapitellar joint, the MALP is the workhorse of the lateral portals. This location is easily palpable and the MALP can be made in an outside-in fashion directly or while viewing from the medial side. Generally speaking, the more distal this portal is placed, the closer it becomes to the radial nerve, and as it is moved more proximal, the margin of safety increases. At the radiocapitellar joint, the MALP is approximately 9.8 mm from the radial nerve.12
Proximal Anterolateral Portal
Perhaps the safest of the lateral portals, the proximal anterolateral portal (PALP) is located 1 to 2 cm proximal to the LE and just anterior to the humerus. Like the PAMP, the PALP can serve as a working or retraction portal. On the lateral side of the elbow, the PALP is the farthest from the radial nerve with an average distance ranging from 9.9 to 13.7 mm.12 It has been found to be an average of 6.1 mm from the posterior antebrachial cutaneous nerve.8
Accessing the Posterior Elbow
Direct Posterior Portal
The direct posterior portal (DPP) has also been referred to as the “posterior central,” “straight posterior,” or “transtriceps” portal. It is located 3 cm proximal to the tip of the olecranon and pierces through the tendinous portion of the triceps. Accordingly, this incision should be made in a proximal to distal orientation in line with the triceps fibers. The DPP provides direct access to the olecranon fossa and allows near full visualization of the posterior joint. Generally, both the medial and lateral gutters can be visualized with the camera in this portal. Given its transtendinous location, it is relatively safe from surrounding neurovascular structures.7, 8, 10
Posterolateral Portal
The posterolateral portal is located along the lateral border of the triceps tendon approximately 1 cm anterior to the midpoint of a line connecting the olecranon and the LE. The proximal-distal location can be adjusted from the level of the tip of the olecranon to 3 cm proximal without neurovascular risk. This portal can be used for working or visualization in conjunction with the DPP or the direct lateral portal (DLP). As long as the location of the radial nerve is understood proximally, this portal is relatively safe.
Direct Lateral Portal
Also described as the “mid-lateral,” “soft-spot,” or “direct posterolateral” portal, the DLP is located in the soft spot of the elbow at the center of a triangle connecting the olecranon tip, LE, and radial head. It pierces the anconeus and can be very helpful for addressing pathology of the radiocapitellar joint. The nearest structure at risk is the lateral antebrachial cutaneous nerve that is located approximately 9.6 mm from the DLP.10
Distal Ulnar Portal
Initially described in 2011, the distal ulnar portal is located 3 to 4 cm distal to the radiocapitellar joint along the lateral border of the ulna.13 This portal also pierces the anconeus and can be helpful in treating osteochondral defects of the posterior and distal capitellum. With increasing degrees of elbow flexion, a larger area of the capitellum can be accessed from this portal. Because it begins 3 to 4 cm distal to the joint, some soft tissue must be traversed before penetrating the capsule. Although there is little risk in the way of neurovascular structures, attempts should be made to minimize injury to the anconeus.
Discussion
The use of elbow arthroscopy is growing at a rapid pace. As technology advances and our knowledge of elbow pathology and anatomy increases, indications for elbow arthroscopy are expanding faster than ever. Although it has evolved into a relatively safe and reliable procedure, complications can occur. Some of the more commonly encountered complications can arise as a result of aberrant tunnel placement, improper patient positioning, or incorrect surgical indications (Table 1). It is critical that the surgeon fully understands and outlines key anatomical structures, especially in cases of prior surgery such as ulnar nerve transposition. To reduce the rate of complications, only the minimal number of portals needed to perform the procedure in a safe and effective manner should be used. Given the propensity of the elbow to swell during arthroscopy, great care should be taken to minimize fluid extravasation. Surgeons should carefully consider the risks and benefits of regional anesthesia for each case on an individual basis. Although it may help with pain control, a regional blockade will delay the time until a postoperative neurologic examination can be performed (Table 1).
Table 1.
Pearls and Pitfalls for Creating Portals for Safe, Arthroscopic Access to the Elbow
| Pearls | Pitfalls |
|---|---|
| Properly position the patient so that the anterior and posterior compartments of the elbow can easily be accessed. | Small errors in patient positioning can compromise intra-articular access and limit the surgeon's ability to complete the case efficiently, effectively, and safely. |
| Meticulously identify and label all key anatomic landmarks before portal creation. | Beware of prior surgical interventions that may have altered or distorted normal anatomy (i.e., previous ulnar nerve transposition). |
| Consider the location of intra-articular elbow pathology when determining which portals to create. | Excessive swelling and fluid extravasation can limit flexion/extension and alter the position of previously known anatomical structures. |
| To reduce the risk of injury or complication, use the fewest number of portals required to safely complete the procedure. | Although multiple accessory portals may be required for complex cases, each additional portal created may increase the risk of complication. |
| Be aware of the proximity of the radial nerve when creating lateral portals. The more proximal the portal, the greater the zone of safety. | Inadvertent distal placement of anterior portals may decrease the safe working distance from critical neurovascular structures. |
| When accessing the anterior elbow from the medial side, be conscientious of the proximity of the median nerve. | Although generally beneficial, preoperative regional blockade will delay the surgeon's ability to perform a postoperative neurologic examination. |
| Always be cognizant of the location of the ulnar nerve, especially if it has previously been transposed. | Because of the location of the ulnar nerve, there is no true safe zone on the medial side of the posterior elbow. |
In an attempt to provide surgeons with a detailed review of the basics of elbow arthroscopy, this 3-part series highlights key principles ranging from surface anatomy to portal placement to patient positioning to diagnostic arthroscopy. It is our hope that this work will help equip new surgeons with knowledge that is critical for successful implementation and execution of this valuable and growing surgical technique.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.S.D. receives support from Arthrex, Conmed Linvatec, Ossur, Biomet, and Wolters Kluwer Health. J.S-S. receives support from Tornier, Merk, Elsevier, and Stryker.
Supplementary Data
The key anatomic landmarks, portal locations, and at risk neurovascular structures are discussed. A right elbow is viewed from the medial, posterior, and lateral sides. For comparative purposes, these key landmarks are shown on a patient in the lateral decubitus position with the arm rested over an arm holder and a patient in the supine position with the arm suspended across the chest in an arm holder.
References
- 1.Guhl J.F. Arthroscopy and arthroscopic surgery of the elbow. Orthopedics. 1985;8:1290–1296. doi: 10.3928/0147-7447-19851001-17. [DOI] [PubMed] [Google Scholar]
- 2.Andrews J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1:97–107. doi: 10.1016/s0749-8063(85)80038-4. [DOI] [PubMed] [Google Scholar]
- 3.O'Driscoll S.W., Morrey B.F. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84–94. [PubMed] [Google Scholar]
- 4.Adams J.E., King G.J., Steinmann S.P., Cohen M.S. Elbow arthroscopy: Indications, techniques, outcomes, and complications. J Am Acad Orthop Surg. 2014;22:810–818. doi: 10.5435/JAAOS-22-12-810. [DOI] [PubMed] [Google Scholar]
- 5.Dodson C.C., Nho S.J., Williams R.J., Altchek D.W. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16:574–585. doi: 10.5435/00124635-200810000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Morrey B.E. Anatomy of the elbow joint. In: Morrey B.E., Sanchez-Sotelo J., editors. The elbow and its disorders. Ed 4. WB Saunders; Philadelphia: 2008. pp. 11–38. [Google Scholar]
- 7.Marshall P.D., Fairclough J.A., Johnson S.R., Evans E.J. Avoiding nerve damage during elbow arthroscopy. J Bone Jt Surg Br. 1993;75:129–131. doi: 10.1302/0301-620X.75B1.8421009. [DOI] [PubMed] [Google Scholar]
- 8.Stothers K., Day B., Regan W.R. Arthroscopy of the elbow: Anatomy, portal sites, and a description of the proximal lateral portal. Arthroscopy. 1995;11:449–457. doi: 10.1016/0749-8063(95)90200-7. [DOI] [PubMed] [Google Scholar]
- 9.Lynch G.J., Meyers J.F., Whipple T.L., Caspari R.B. Neurovascular anatomy and elbow arthroscopy: Inherent risks. Arthroscopy. 1986;2:190–197. doi: 10.1016/s0749-8063(86)80067-6. [DOI] [PubMed] [Google Scholar]
- 10.Unlu M.C., Kesmezacar H., Akgun I., Ogut T., Uzun I. Anatomic relationship between elbow arthroscopy portals and neurovascular structures in different elbow and forearm positions. J Shoulder Elb Surg. 2006;15:457–462. doi: 10.1016/j.jse.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Poehling G.G., Whipple T.L., Sisco L., Goldman B. Elbow arthroscopy: A new technique. Arthroscopy. 1989;5:222–224. doi: 10.1016/0749-8063(89)90176-x. [DOI] [PubMed] [Google Scholar]
- 12.Field L.D., Altchek D.W., Warren R.F., O'Brien S.J., Skyhar M.J., Wickiewicz T.L. Arthroscopic anatomy of the lateral elbow: A comparison of three portals. Arthroscopy. 1994;10:602–607. doi: 10.1016/s0749-8063(05)80055-6. [DOI] [PubMed] [Google Scholar]
- 13.van den Ende K.I.M., McIntosh A.L., Adams J.E., Steinmann S.P. Osteochondritis dissecans of the capitellum: A review of the literature and a distal ulnar portal. Arthroscopy. 2011;27:122–128. doi: 10.1016/j.arthro.2010.08.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The key anatomic landmarks, portal locations, and at risk neurovascular structures are discussed. A right elbow is viewed from the medial, posterior, and lateral sides. For comparative purposes, these key landmarks are shown on a patient in the lateral decubitus position with the arm rested over an arm holder and a patient in the supine position with the arm suspended across the chest in an arm holder.