Abstract
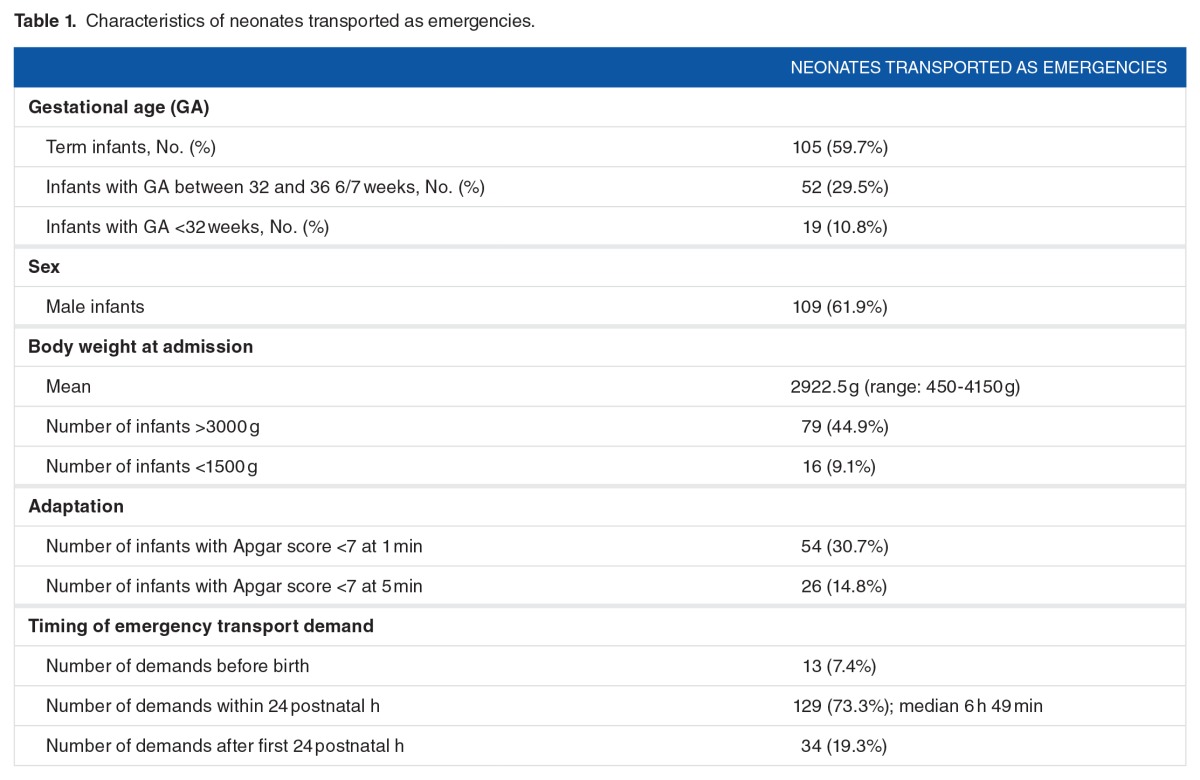
Neonatal transport is an essential part of regionalization for highly specialized neonatal intensive care. This retrospective analysis of prospectively collected data on neonatal transport activity in a large Swiss perinatal network more than 1 year, aimed to quantify this activity, to identify the needs for staff, and the demands regarding know-how and equipment. Of the 565 admissions to the tertiary neonatology clinic, 176 (31.2%) were outborn patients, transported as emergencies to the level III unit. In 71.6% of cases, respiratory insufficiency was one of the reasons for transfer. Circadian and weekly distribution showed increased transport activity on workdays between 8 am and 10 pm, but regular demands for emergency transports regardless of the time frame require a neonatal transport team available 24/7. This study highlights the importance of neonatal transport and unveils several functional and infrastructural insufficiencies, which led to suggestions for improvement.
Keywords: Neonatal transport, regionalization, neonatal network, perinatal care, emergency transport
Introduction
Regionalization in perinatology is a concept that emerged in the 1960s with the aim of managing highly specialized neonatal resources efficiently.1 In 1971, the American Medical Association advised the establishment of guidelines to reach 2 goals: (1) to permit high-risk pregnancies to be recognized in time to reach a hospital with the appropriate level of care for mother and child and (2) to identify high-risk neonates for rapid transfer to specialized neonatal units.2 Such a system implies 2 types of emergency transport: (1) transport of the pregnant woman with the fetus in utero and (2) postnatal transport of the ill newborn infant. It is now widely accepted that in utero transport is preferable to postnatal referral.3–10
Regionalization in perinatal networks demands the following: (1) the acknowledgment of the degree of care each hospital can provide for mothers and newborn infants, (2) an efficient system for recognizing high-risk pregnancies and permitting their antenatal transport to a hospital with the appropriate level of care, (3) neonatal facilities able to cope quantitatively and qualitatively with all medical requests coming from within the neonatal network, and (4) a suitable neonatal transport operation. Such a neonatal transport service needs to ensure safe and rapid emergency referrals from any maternity department to the neonatal intensive care unit (NICU) around the clock, as well as retransfers of convalescent newborn infants to peripheral hospitals, ideally the one closest to the parents’ home. These retransfers facilitate parental access to their child, increase the availability of cots in the NICU for emergencies, and allow the regional hospitals to uphold their competences.11,12
In Switzerland, the definition of 3 levels of neonatal care has been published recently with level I as a maternity ward providing care for healthy newborn infants, level II as a special neonatal care unit equipped with (level IIB) or without (level IIA) noninvasive nasal continuous positive airway pressure (CPAP) devices, and level III as a network center with a NICU.13 Regionalization of perinatal care in Switzerland, which counts about 80 000 live births per year, is organized into 9 different geographic regions, each with between 4000 and 16 000 births per year and 1 or 2 NICUs.
The goal of this study was to quantitatively analyze the neonatal transport activity and its needs within the Regional Perinatal Network of Lausanne (RPNL), one of the largest perinatal networks in Switzerland, covering most of the western, French-speaking part of the country. The focus of this study was to evaluate the efficacy of the neonatal transport system with special attention to the overall transport activity, the time intervals during transport, and the analysis of the profile of transported neonates, to make suggestions to improve collaboration within the perinatal network.
Patients and Methods
In Switzerland, standards of neonatal care were only defined in 2011 and levels of care were only attributed definitely to pediatric/neonatal units in 2015. However, in the French-speaking part of Switzerland, the roles of each center have been undisputed since the late 1990s.12 According to these practices, all preterm infants <32 weeks of gestation should be delivered in the level III perinatal center to avoid postnatal emergencies. One objective was to determine whether these recommendations were followed during the study year.
The RPNL covers the whole French-speaking, western part of Switzerland (except the cantons of Geneva and Jura) comprising a population of roughly 1.2 million and about 14 000 births per year, of which on average 16% (2400 live births in the study year) take place at CHUV (Centre Hospitalier Universitaire Vaudois—University Hospital of Lausanne). The Clinic of Neonatology with its NICU, as part of the CHUV, is the only tertiary referral center of the RPNL, which includes 9 level II and 3 level I neonatal units. Almost all neonatal transports within the RPNL are performed by a specialized neonatal transport team (NTT) from CHUV composed of a neonatologist or a fellow in training and a nurse qualified in neonatal intensive care. The NTT depends on 2 assigned private emergency companies for the transport vehicle, 1 for ground transport with a specially equipped ambulance (STAR Ambulances, Epalinges, Switzerland) and 1 for air transport with a rescue helicopter (Rega, Lausanne, Switzerland). Transport activities by the NTT can be grouped into 3 main categories: (1) transport of newborn patients in urgent situations (further named emergency transports) from a level I or II unit to a level III unit, (2) referral to another tertiary center due to lack of capacity at CHUV (postnatal refusals), (3) Retransfer of convalescent patients from CHUV to the medical facility closest to the parents’ home (in this case, the NTT is reduced to a single member, usually the nurse) with the same ambulance.
Prenatal transfers are undertaken by different transport companies and organized by the obstetrical team, the details of which are not discussed here.
This study is a retrospective analysis of prospectively collected data of all transported neonatal patients within the RPNL over a full calendar year (2008). Information on neonatal transport is systematically documented on transport forms by the NTT during a transport mission. Emergency transport forms carry administrative information, times of different phases of transport, and patient data. Similar documents exist for refusals and retransfers. Further patient information, in particular, regarding diagnosis and treatment, was collected from the patient’s medical chart, the patient data acquisition system during hospitalization (MetaVision, iMDsoft, Tel Aviv, Israel), and the electronic medical database (Archimède, version V3.8, ELCA Informatique SA, Lausanne, Switzerland).
Each emergency transport mission can be subdivided into different time intervals, as defined in Figure 1. Close attention was paid to reaction time (time interval between emergency call and presence of the NTT at the patient’s bedside) to assess whether and how it could be reduced and to establish recommendations. To have the complete and precise data about the timing of each emergency mission, the times of each step of the intervention noted on the transport forms were matched with the corresponding information on the transport forms of the associated transport company. All emergency transports were further examined to determine whether transport was indeed performed due to an urgent situation. All data were transferred and gathered in an Excel document. Verification of the quality of data was performed by a double check of 25% of all completed data sets selected in a random fashion by the second author. For all the patients, diagnoses were reviewed by 2 authors to define which were relevant for the referral to the NICU, considering the limitations of case management in the centers making the request. Final diagnoses were extracted from the patient’s discharge report of the level III unit and classified according to the following categories: circulation, gastrointestinal disorders, hematology, infection/immunology, malformation, metabolism, neurology, prematurity, and respiration.
Figure 1.
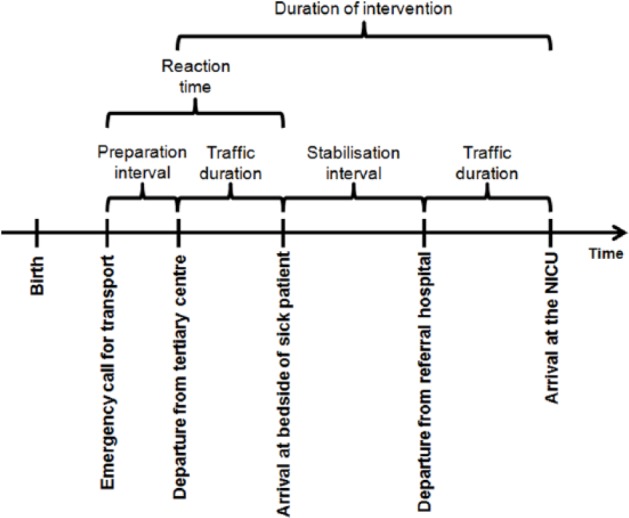
Timing and intervals of neonatal emergency transport. NICU indicates neonatal intensive care unit.
Results
During the study period, 456 patients were transported. In 92% of all transported patients, a full data set was available. Missing items consisted of details on timing, on degree of severity, and on medical procedures undertaken during the transport mission. There were 204 emergency transport missions accomplished by the NTT. On 5 occasions, twins were transported during the same mission, adding to a total of 209 patients involved. In 3 cases, the transport team was sent out, but patient transfer itself was not undertaken due to death of the patient before arrival on 2 occasions and total recovery of the third patient. Of the remaining 206 patients, 175 were transported to CHUV’s NICU, 13 were transported to another level III NICU in Switzerland because of refusal at CHUV, and 18 patients were counted as annex transports (such as referrals to other units of CHUV for specialized investigations). Ground transport performed by the NTT accounted for 86.9% (n = 153/175) of cases, and the remaining 13.1% was by helicopter. Retransfers concerned 250 infants.
Of the 107 preterm infants with gestational age <32 weeks cared for at the CHUV, 97 infants (90.8%) were inborn. The remaining 10 (9.2%) high-risk preterm infants were born in regional hospitals due to imminent delivery preventing immediate intrauterine transport. The NTT was alerted before birth in 8 of these situations, allowing the rescue team to be present at birth or at least within the first 30 minutes in all 8 situations.
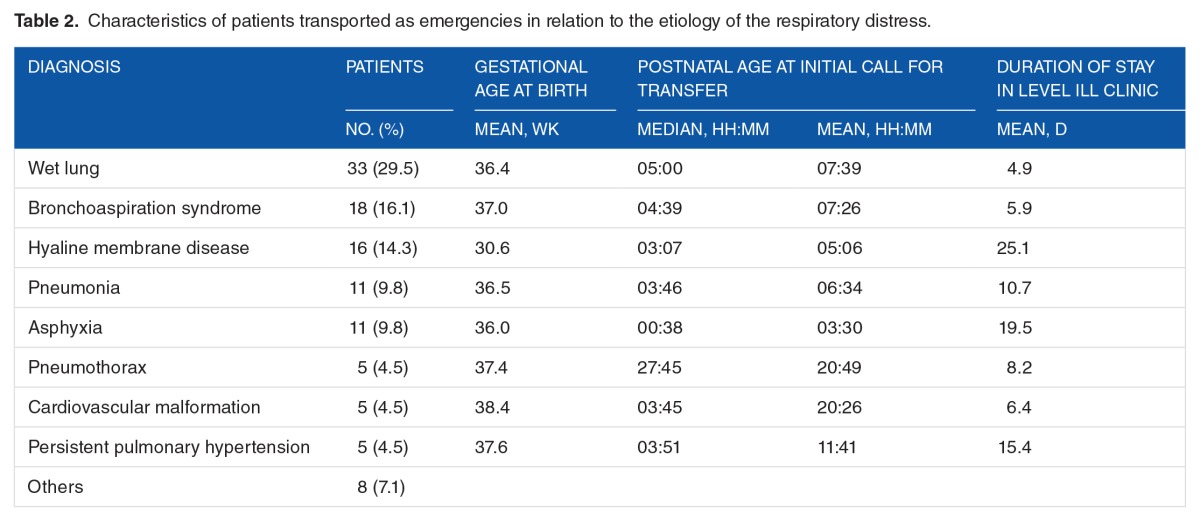
Among the 565 admissions to the Clinic of Neonatology of CHUV, 31.2% (n = 176) were outborn and transported to CHUV as emergencies (175 by the NTT of CHUV and 1 by a neighboring perinatal network’s team). Their characteristics are listed in Table 1. Medical reasons for emergency transport within the first 24 hours are listed in Figure 2. By far, the most important category was respiratory distress (71.6%), which we further analyzed according to final diagnosis (Table 2). Respiratory distress due to wet lung (29.5%), aspiration syndrome (16.1%), surfactant deficiency provoking hyaline membrane disease (14.3%), pneumonia (9.8%), and asphyxia (9.8%) accounted together for 79.6% of all final respiratory diagnoses. Of the 175 transported patients, 112 (64%) were in need of urgent respiratory support consisting of endotracheal intubation with mechanical ventilation in 24 patients (13.7%), noninvasive mechanical ventilation in the form of CPAP with nasal canula (80 patients, 45.7%), and/or drainage of a pneumothorax in 4 patients (2.3%), all highly specialized procedures in newborn and preterm infants. The remaining 4 patients necessitated oxygen therapy only. Unfortunately, data on procedures such as surfactant administration, umbilical line placement, blood gas analysis, and prostaglandin perfusion during transport were too incomplete to be studied.
Table 1.
Characteristics of neonates transported as emergencies.
Figure 2.
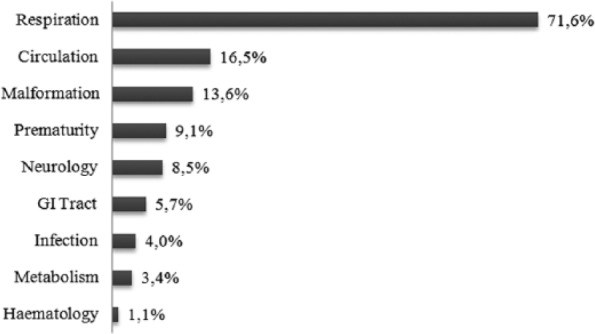
Problems causing neonatal emergency transport related to organ systems. Multiple causes per patient are possible. GI indicates gastrointestinal.
Table 2.
Characteristics of patients transported as emergencies in relation to the etiology of the respiratory distress.
Mean preparation time, that is, the time interval between the first emergency call and the departure of the ambulance at CHUV, was 34 minutes. Reaction time in relation to the distance between referral hospital and CHUV is shown in Figure 3. For ground transport in the RPNL, it was observed that the reaction time was a linear function between the distance (0.58 min/km) and the preparation time. Stabilization time, defined as the interval between the arrival of the NTT at the patient’s bedside and the departure from the referring hospital, averaged at 57 minutes with a median of 45 minutes (range: 15–220 minutes). Longer intervals were in general observed in hospitals with a lower level of care. The mean reaction time in the RPNL was 62 minutes. Mean intervention time for 169 of the 175 patients (timing data are incomplete for 6 patients) was 1 hour 47 minutes (SD: 50 minutes) with a median of 1 hour 33 minutes (range: 28 minutes-5 hours 14 minutes). Most requests for emergency transfers (81.7%; n = 138) were recorded in the 14 hours between 8 am and 10 pm with a maximum of 15.4% between 2 pm and 4 pm (Figure 4(A)). There was a slight predominance of emergency transport requests between Wednesday and Friday; however, even on weekends, a considerable number of transports needed to be performed (Figure 4(C)).
Figure 3.
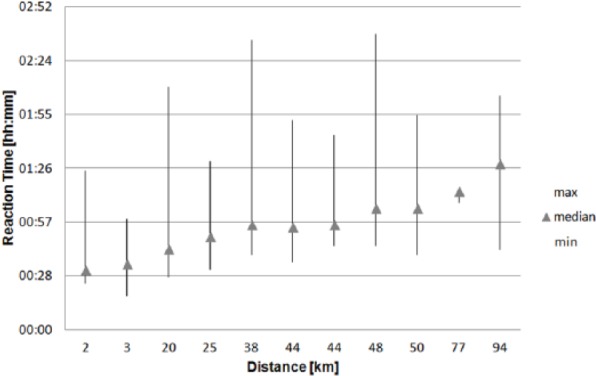
Mean reaction time related to distance between referral center and level III neonatal unit. Reaction time: time lag between initial emergency call and arrival of the transport team at the patient’s bedside. Data given as median and full range per hospital.
Figure 4.
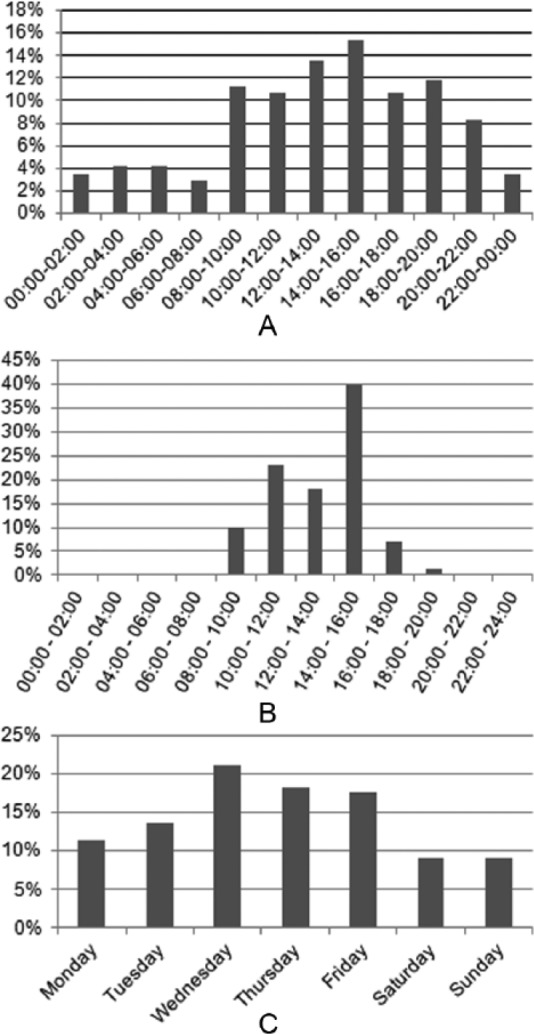
(A and B) Circadian and (C) weekly distribution of (A and C) emergency transports and (B) retransfers.\
During the study year, 33 pregnant women (concerning 50 fetuses due to multiple pregnancies) and 34 newborn infants could not be admitted to the level III unit. Refusal of antenatal requests was caused by a lack of available neonatal cots in the NICU in 84.8% (n = 28). In the other 5 situations, lack of free beds on the obstetrical ward was the cause of refusal. Mean gestational age at the time of the antenatal transfer request was 31 weeks (range: 24–35 weeks). In 28 cases (42 fetuses), transfer took place to another Swiss level III center; on 1 occasion (triplets), the patient remained in the same level IIB unit, and for the remaining 4 women, data were missing. Within the postnatal group, a lack of available cots in the NICU was the reason for refusal in all but 1 case (97.1%) in which a major road traffic accident made transfer impossible. Mean gestational age at birth of the refused newborn infants was 35 weeks (range: 30–41 weeks). Of the 34 refused patients, 16 were admitted to other pediatric units at CHUV, 9 were transferred to other level III centers, 7 showed signs of clinical improvement and stayed at the referral hospital, and 2 were transferred from the level I center to a level IIA center.
Retransfers concerned 250 infants in 222 transport missions (28 simultaneous twin retransfers). Of these, 206 retransfers (233 neonates) were performed by the NTT and the remaining by the accepting hospital.
Of the 176 outborn neonates initially transported as emergencies to CHUV, 46.3% (n = 81) were retransferred back after stabilization, 12.6% (n = 22) were transferred to other units within CHUV for further management (pediatric intensive care, continuous care unit, or pediatric surgery), 31.4% (n = 55) were discharged home directly, 7.5% (n = 13) joined their mother in the maternity ward, and 4 infants died (2.3%).
Mean duration of the retransfers was 1 hour 25 minutes (range: 22 minutes-4 hours 20 minutes), of which a mean of 29 minutes was spent on the handover of the patient at the peripheral hospital. Of all retransfer missions, 217 (97.8%) departed from CHUV between 8 am and 6 pm with a peak of 39.9% between 2 pm and 4 pm (Figure 4(B)).
Discussion
Perinatal health care is organized in many countries in regional perinatal networks consisting of health institutions with different levels of care for pregnant women as well as for newborn infants. In a well-run perinatal network, the roles, missions, and limits of provision of care are defined and publicly attributed to all participating perinatal health facilities.12,14
As one marker of acceptance of these guidelines, the number of very preterm infants (<32 weeks of gestational age) born in a lower level clinic than the tertiary center was examined. The inborn rate of >90% of high-risk pregnancies at CHUV is among the highest when compared with literature.15–17 Thanks to a rapid and direct alarm system and short transport distances within the network, the specialized NTT of the tertiary center was in charge of the outborn babies at birth or within the first 30 minutes in more than 98% of situations. The goal of the NTT as part of regionalization, that is, providing the highest level of neonatal care over the whole network area, ideally starting at birth, was therefore almost reached, as the equipped NTT can be considered as a mobile NICU.10 The presence of a trained NTT from a tertiary center with all the required NICU equipment was shown to improve the quality of initial management and stabilization.18 The data presented here show that in a regional perinatal network with clear antenatal transfer guidelines and levels attributed to all health care institutions, as well as good communication and straightforward collaboration, high-risk preterm deliveries in a nontertiary center can be reduced to a nonsignificant number. Postnatal emergency transport in foreseeable situations should be avoided.
Neonatal emergency transport mainly concerns late preterm and term infants with medical issues appearing postnatally. In almost three-quarters of all patients, respiratory distress was among the referral causes with indication for noninvasive or invasive respiratory support. This implies that the staff of the NTT needs to be familiar with and equipped for any kind of respiratory support, including endotracheal intubation, possible surfactant application, and drainage of pneumothorax, as well as invasive and noninvasive ventilation during the transport.19 The profession of nurse practitioners or respiratory therapists does not exist in Switzerland. Therefore, the NTT usually counts a trained neonatologist or fellow in training and a nurse experienced in neonatal intensive care.
By Swiss standards, emergency transports in the RPNL are quite frequent with an average of 2 missions every 3 days. However, this workload is not sufficiently high to create an NTT independent from the NICU of the level III center, as a separate stand-alone transport service, as suggested in other countries.20 This has some major drawbacks: (1) being part of the health care team of the NICU, the 2 members of the NTT have to hand over their patients after an emergency call before their departure, which might increase the preparation interval and therefore the reaction time; (2) during the whole duration of an emergency intervention, the 2 staff members of the NTT are dedicated to care for 1 patient only, whereas the other hospitalized patients have to be cared for by the remaining staff; (3) this represents an additional stress not only for the NTT but also for the remaining reduced staff in the NICU. Although the data presented here show a 2-fold to 3-fold number of emergency transports during daytime, they are not rare at night and weekends and are therefore sporadic and unpredictable. This implies that this cost-intensive and highly specialized emergency structure has to be maintained and available 24 hours a day all year round.
For patient safety in a network, reaction time should be as short as possible. This time depends on the rapid availability of the transport vehicle and the NTT. Ideally, the vehicles for ground and air transportation should be located at the same place together with a centralized independent NTT. For economic reasons, an independent NTT is not an option in the RPNL. To minimize preparation time, the ambulance for ground transport is required to be based at the hospital, whereas accessibility of the helicopter demands more time. In perinatal networks with short travel distances, as is the case in the RPNL with most centers within a range of 50 km of the level III unit, air transportation is of limited use. In the 2 centers at a distance of >90 km, reaction time for air transport seemed to be slightly but clinically not significantly shorter compared with ground transportation (data not shown), similar to findings in recent literature.21,22 However, in each perinatal network, specific recommendations have to be based on the local traffic situation, geographic circumstances, and weather conditions.23
The number of refusals is a key parameter in a perinatal network, reflecting its efficiency, its neonatal health care resources, and its saturation. During the study period, 6 admissions to the NICU had to be confronted to 1 refusal on average, either pre- or postnatally. This clearly demonstrates the insufficient availability of NICU cots to face the neonatal needs of the 14 000 live births in the network area. Patients had to be transferred to other tertiary perinatal centers with, as a consequence, prolonged transport times and separation of the patients from their family. Such data can support demands for an extension of the NICU, to reach the minimal requirements of 1 NICU bed per 1000 live births.24
An optimal use of health care resources, provided by the different participating facilities in a perinatal network, relies on the retransfer of stabilized patients, who no longer need intensive care, to a lower level of care. The number of retransferred patients within the RPNL exceeded the total of emergency transfers by more than 40%. This reflects that high-risk pregnancies are usually transported prenatally, as required, and that there is no unnecessary retention of newborn infants in the tertiary center. Retransfers are usually performed by a single nurse who does not participate in the emergency NTT. However, the ambulance vehicle is the same. The data have shown that more than 80% of the patients were retransferred between 10 am and 4 pm, which corresponded to the same peak times as emergency transports (Figure 4). Based on this fact, efforts of the recipient hospitals within the RPNL were made to admit retransferred patients earlier in the morning and later in the evening, as well as at weekends. Furthermore, an improved communication concept has been elaborated together with the ground transport company to inform them earlier on upcoming possible retransfers to anticipate the availability of a second ambulance for emergencies if necessary.
This study was designed to analyze the setup of neonatal transport and the population of transported infants and as such does not allow a comparison of morbidity and mortality of transported, outborn, versus inborn patients in our population. One of the goals of this study was to examine the quality of the transport activity, including the medical procedures performed, events leading to a clinical deterioration, and also any technical problems during the transport missions. Unfortunately, our inspection of the record sheets showed that the information provided regarding these aspects was insufficient, except for respiratory interventions, and therefore did not permit us to make representative statements. As a result, a project for a better standardization of medical records during transport was started. This includes supplying the NTT with a laptop computer loaded with a user-friendly questionnaire to replace the paper record sheets and better documentation during transport with integration of the data from the monitor and ventilation systems of the transport unit into the patient’s medical chart once at the NICU. Such a system will not only be of interest for statistical use, but, and more importantly, for patient safety and also for financial and potential legal aspects.
Conclusions
Although antenatal transfer of high-risk pregnancies to tertiary perinatal centers is the favored method of transport in a perinatal network, postnatal urgent transport remains a key component of interhospital, perinatal collaboration. Analyses, as performed in this study, are an important tool for describing, quantifying, and qualifying different aspects of neonatal transport, and, in particular, for discovering pitfalls and to achieve improvements. Therefore, we suggest that further studies should focus on the efficacy, performance, functionality, and safety of neonatal transport to improve this high-risk intervention in the most delicate period of life of the very vulnerable population of newborn infants.
Footnotes
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 988 words, excluding any confidential comments to the academic editor.
FUNDING: The author(s) received no financial support for the research, authorship, and/or publication of this article.
DECLARATION OF CONFLICTING INTERESTS: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
CGME, MSB, and MRK designed the research (project conception, development of the overall research plan). CGME, ED, MSB, and CSD conducted the research (patient data collection, data verification, and data analysis). CGME wrote the manuscript under the supervision and with participation of JFT and MRK.
Ethical Approval
This study involving human participants was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethical Commission for Clinical Research of the Canton de Vaud. Designed as an observational study, no informed consent was needed.
REFERENCES
- 1.Yu VY, Dunn PM. Development of regionalized perinatal care. Semin Neonatol. 2004;9:89–97. doi: 10.1016/j.siny.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Ryan GM. Editorial: childbirth, American style. JAMA. 1975;233:451. doi: 10.1001/jama.233.5.451. [DOI] [PubMed] [Google Scholar]
- 3.Brun JL, Billeaud C, Elleau C, et al. Maternal transport to the Bordeaux University Hospital: a retrospective study of 263 cases (1996–1998) J Gynecol Obstet Biol Reprod (Paris) 2000;29:414–422. [PubMed] [Google Scholar]
- 4.Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK, Canadian Neonatal Network Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol. 2001;98:247–252. doi: 10.1016/s0029-7844(01)01438-7. [DOI] [PubMed] [Google Scholar]
- 5.Harris BA, Jr, Wirtschafter DD, Huddleston JF, Perlis HW. In utero versus neonatal transportation of high-risk perinates: a comparison. Obstet Gynecol. 1981;57:496–499. [PubMed] [Google Scholar]
- 6.Kollee LA, Eskes TK, Peer PG, Koppes JF. Intra- or extrauterine transport? Comparison of neonatal outcomes using a logistic model. Eur J Obstet Gynecol Reprod Biol. 1985;20:393–399. doi: 10.1016/0028-2243(85)90063-2. [DOI] [PubMed] [Google Scholar]
- 7.Hohlagschwandtner M, Husslein P, Klebermass K, Weninger M, Nardi A, Langer M. Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet. 2001;265:113–118. doi: 10.1007/s004040100197. [DOI] [PubMed] [Google Scholar]
- 8.Kempley ST, Baki Y, Hayter G, Ratnavel N, Cavazzoni E, Reyes T. Effect of a centralised transfer service on characteristics of inter-hospital neonatal transfers. Arch Dis Child Fetal Neonatal Ed. 2007;92:F185–F188. doi: 10.1136/adc.2006.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2010;95:F403–F407. doi: 10.1136/adc.2010.183236. [DOI] [PubMed] [Google Scholar]
- 10.Messner H. Neonatal transport: a review of the current evidence. Early Hum Dev. 2011;87:S77. doi: 10.1016/j.earlhumdev.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 11.Bowman E, Doyle LW, Murton LJ, Roy RN, Kitchen WH. Increased mortality of preterm infants transferred between tertiary perinatal centres. BMJ. 1988;297:1098–1100. doi: 10.1136/bmj.297.6656.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tolsa JF, Calame A, Fawer CL, Prod’Hom LS. Experiences of the division of neonatology of Lausanne. Arch Pediatr. 1999;6:222s–224s. doi: 10.1016/s0929-693x(99)80419-9. [DOI] [PubMed] [Google Scholar]
- 13.Commission for the Accreditation of Neonatal Units (CANU) in Switzerland Minimum requirements for Swiss neonatal units. http://www.neonet.ch/files/7314/4968/0165/2013_08_28_-_Minimum_Requirements_for_Swiss_Neonatal_Units.pdf. Published August 28, 2013.
- 14.Marlow N, Bryan GA. Establishing neonatal networks: the reality. Arch Dis Child Fetal Neonatal Ed. 2007;92:F137–F142. doi: 10.1136/adc.2005.086413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Nisi G, Berti M, Malossi R, Pederzini F, Pedrotti A, Valente A. Comparison of neonatal intensive care: Trento area versus Vermont Oxford Network. Ital J Pediatr. 2009;35:5. doi: 10.1186/1824-7288-35-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lecoeur C, Thibon P, Prime L, et al. Frequency, causes and avoidability of out-born births in a French regional perinatal network. Eur J Obstet Gynecol Reprod Biol. 2014;179:22–26. doi: 10.1016/j.ejogrb.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Clerc J, Doret M, Decullier E, Claris O, Picaud JC, Dupuis O. Is it possible to prevent preterm births outside of level-3 maternity wards? Experience of Greater Lyon perinatal network. Gynecol Obstet Fertil. 2011;39:412–417. doi: 10.1016/j.gyobfe.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 18.McNamara PJ, Mak W, Whyte HE. Dedicated neonatal retrieval teams improve delivery room resuscitation of outborn premature infants. J Perinatol. 2005;25:309–314. doi: 10.1038/sj.jp.7211263. [DOI] [PubMed] [Google Scholar]
- 19.Karlsen KA, Trautman M, Price-Douglas W, Smith S. National survey of neonatal transport teams in the United States. Pediatrics. 2011;128:685–691. doi: 10.1542/peds.2010-3796. [DOI] [PubMed] [Google Scholar]
- 20.Fenton AC, Leslie A, Skeoch CH. Optimising neonatal transfer. Arch Dis Child Fetal Neonatal Ed. 2004;89:F215–F219. doi: 10.1136/adc.2002.019711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Insoft RS. Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015. [Google Scholar]
- 22.Ohning B. Transport of the critically ill newborn. http://emedicine.medscape.com/article/978606-overview. Published 2012.
- 23.Killion CS, Stein HM. The impact of air ambulance transport on neonatal outcomes. Newborn Infant Nurs Rev. 2009;5:207–211. [Google Scholar]
- 24.Wilkinson A. Standards for hospitals providing neonatal intensive and high dependency care. http://www.bapm.org/publications/documents/guidelines/hosp_standards.pdf. Published 2001.