Abstract
Background
The accessibility of surgical patient data is a key safety concern, and relies on efficient clerking and handovers. This project assessed whether the introduction of a surgical clerking proforma improved the recording of patient information in the surgical admissions unit (SAU) at Northwick Park Hospital.
Materials and methods
Existing patient notes were assessed on content and ease of access, using two independent surveys conducted over a 5-day period. The first survey audited patient notes before (n = 28) and after (n = 23) the introduction of the proforma. It assessed whether key patient details were documented, in line with the 17 criteria set out in the Guidelines for Clinicians on Medical Records and Notes by The Royal College of Surgeons in England. The second survey questioned healthcare professionals before (n = 25) and after (n = 17) proforma implementation on the accessibility of patient data and coherency of patient notes.
Results
5 of the 17 criteria showed significant differences post proforma implementation. Of these differences, the recording of height and occupation was most notable (p < 0.01). Medication history, weight and investigations also showed significant increases in documentation (p < 0.05). In all 3 questions asked to healthcare professionals, fewer healthcare professionals were required to revisit archived notes following proforma implementation (p < 0.05).
Conclusion
Our study illustrates that a comprehensive surgical clerking proforma improves patient data documentation and saves healthcare professionals' time compared to the freehand clerking method. The implications of such work are far reaching, and if well implemented could allow a new reliable platform for further clinical audits.
Keywords: Proforma, Surgery, Documentation, Clerking, Safety
Highlights
-
•
A study comparing the implementation of a surgical clerking proforma vs. freehand clerking.
-
•
The coherency of patient notes before and after proforma implementation was assessed.
-
•
5 of the 17 criteria showed significant improvement post proforma implementation.
-
•
Fewer healthcare staff were required to revisit patient notes following proforma implementation.
-
•
The study illustrates that the implementation of a surgical admissions proforma improves patient documentation.
1. Background
Good quality patient care relies on the completeness of information, to which accurate documentation is essential [1]. Failure to produce accessible notes can lead to delayed patient treatment. For effective communication to take place between healthcare professionals, patient information must be recorded as accurately as possible. However, notes are notoriously inaccessible and poorly maintained [2].
The Royal College of Surgeons of England (RCSE) have produced Guidelines for Clinicians on Medical Records and Notes [3]. This sets out 17 criteria that should be included in all surgical patient documentation. This includes the patient's name, address, date of birth, unique identification number, occupation, patient history, past medical and surgical history, current medication, initial examination including patient's height and weight, a working diagnosis and a plan. Unfortunately one or more of these criteria are routinely omitted from documentation [4].
At Northwick Park Hospital the existing clerking system was not standardised, which meant that some information could only be accessed from previous ward notes. The method of choice for clerking was handwriting notes on lined paper. Studies have shown that healthcare professionals prefer printed forms when clerking patients in both general medicine and surgery [5], [6]. Therefore, the implementation of a clear, comprehensive proforma warranted investigation.
The aim of this study was to compare the completeness of a handwritten clerking method to a new surgical clerking proforma for patients admitted to the Surgical Admissions Unit of a large teaching hospital, and to qualitatively assess its impact on the opinions of healthcare staff towards patient notes.
2. Methods
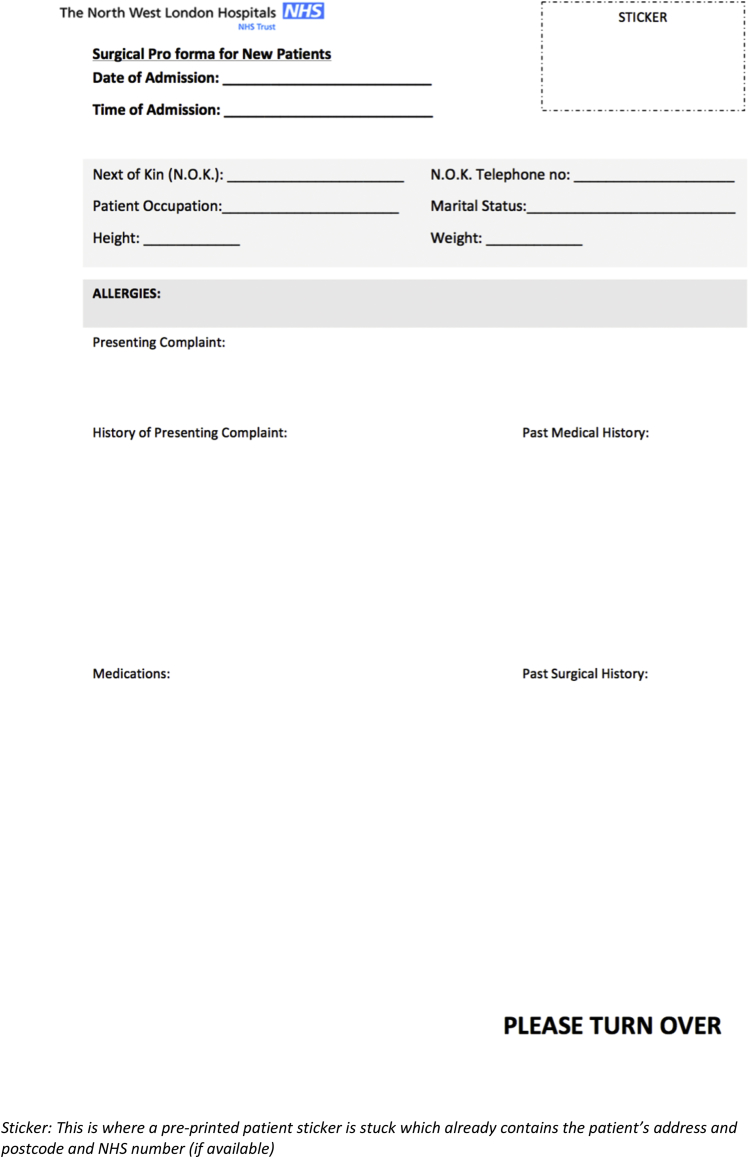
A prospective study of all patients admitted to the Surgical Admissions Unit was conducted during two separate one-week periods, whereby a full audit cycle was completed. The surgical admissions clerking proforma was designed based on the 17 criteria set out by the RCSE, with additional input from senior consultants (Fig. 1). It also included a section where the clerking healthcare professional could identify themselves by name, grade, date and phone/bleep number (Fig. 1).
Fig. 1.
The Surgical Clerking Proforma. A double sided A4 document where patient details can be documented.
The study was split into 3 phases:
-
1)
an initial audit of traditional free-hand patient notes
-
2)
the design and implementation of a new clerking proforma
-
3)
a re-audit of patient notes on the new clerking proforma
All patient notes from surgical admissions between the hours of 8 am to 5 pm over the course of 5 consecutive days were assessed in each arm of the audit. Completeness of documentation was assessed according to the presence or absence of the 17 criteria set out in RCSE guidelines (Table 1).
Table 1.
Score sheet used to assess patient notes before and after implementation of the proforma.
| Criteria | YES/NO |
|---|---|
| Hospital Record | |
| Date of Admission | |
| Time of Admission | |
| NHS Number | |
| Address and Postcode | |
| Date of Birth | |
| Next of Kin | |
| Occupation | |
| Marital Status | |
| Registered GP | |
| Details of Clinical Record | |
| Presenting complaint | |
| History of Presenting Complaint | |
| Full Medication History | |
| Examination Findings | |
| Patients height | |
| Patients weight | |
| Working diagnosis | |
| Medical/Surgical Plan | |
To allow staff to familiarise themselves with the new system, a one-week introduction period was in place. Reminders during staff meetings were in place to raise awareness of the new system. Following the introduction period, the new proforma was audited against the same RCSE guideline score sheet used in phase 1.
Questionnaires were distributed amongst healthcare professionals on the ward before and after the implementation to evaluate views towards the completeness and accessibility of patient information (Table 2). Questions were answered anonymously and responses were recorded in a simple yes/no tick box.
Table 2.
Score sheet used to assess healthcare professionals' attitude towards the completeness of patient notes before and after implementation of the proforma.
| Criteria | YES/NO |
|---|---|
| Have you been required to revisit archived notes regarding this patient's care? | |
| Have you needed further clarification by a fellow health care professional? | |
| Are the notes organised in a coherent and chronological manner? |
A T-Test assuming unequal variance was applied to compare the difference in completion of documentation and healthcare professionals' attitudes before and after the implementation of the proforma. A p-value < 0.05 was considered statistically significant.
3. Results
Patient notes were assessed before and after the implementation of the new clerking proforma (n = 28 and n = 23 respectively). Of the 17 criteria for completeness of documentation, 13 showed increased rates of completion, 5 of which were statistically significant (see Table 4).
Table 4.
Comparison of completeness of documentation before and after implementation of proforma.
| Traditional clerking (%) | New Proforma (%) | p-value | |
|---|---|---|---|
| Date and time of admission | 96 | 100 | 0.33 |
| NHS number | 96 | 100 | 0.33 |
| Address and postcode | 100 | 100 | 1 |
| DOB | 100 | 100 | 1 |
| Next of kin | 86 | 78 | 0.5 |
| Occupation | 4 | 70 | <0.01* |
| Marital status | 79 | 83 | 0.72 |
| Registered GP | 86 | 91 | 0.53 |
| PC | 100 | 100 | 1 |
| HPC | 96 | 100 | 0.33 |
| Full medication history | 79 | 100 | <0.05* |
| Examination findings | 96 | 100 | 0.33 |
| Height | 0 | 43 | <0.01* |
| Weight | 36 | 70 | <0.05* |
| Working diagnosis | 96 | 100 | 0.33 |
| Medical/surgical plan | 100 | 100 | 1 |
| Investigations since admission, with timings | 57 | 87 | <0.05* |
*Denotes statistical significance.
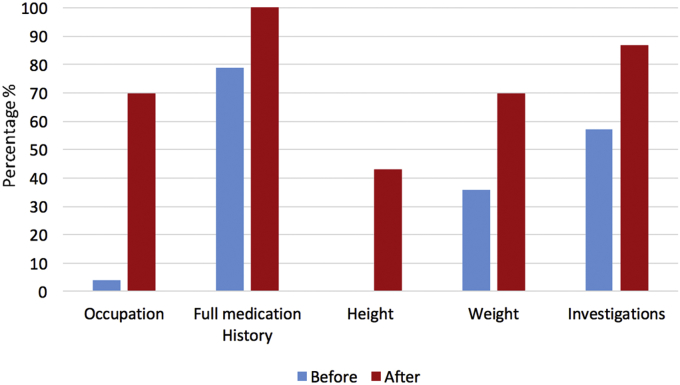
The most significant increases (Fig. 2) were noticed in height (95% Cl +43%, p < 0.01) and occupation (95% CI + 66%, p < 0.01). Significant improvements in documentation of medication history (95% Cl +21%, p < 0.05), weight (95% Cl +34%, p <0.05%) and investigations since admission (95% Cl +30%, p < 0.05) were also found.
Fig. 2.
Completion rates of 5 variables before and after the implementation of the clerking proforma.
Before the implementation of the proforma, 25 healthcare professionals anonymously completed the questionnaire which ascertained the completeness of patient notes. 17 healthcare professionals were subsequently interviewed to identify whether there was a change in attitude towards the accessibility and coherency of notes (the results of which can be seen in Table 3). Fewer healthcare professionals were required to revisit archived notes (p < 0.05) or to clarify information with colleagues following the implementation. Similarly, a greater proportion of participants felt that the notes were organised in a coherent and chronological order after the proforma was in use, although the latter two findings were not statistically significant.
Table 3.
Qualitative assessment of patient notes utility by healthcare professional staff.
| Before (% YES) | After (%YES) | Change | |
|---|---|---|---|
| Have you been required to revisit archived notes regarding this patient's care? | 24 | 0 | −24 |
| Have you needed further clarification by a fellow health care professional? | 52 | 35 | −17 |
| Are the notes organised in a coherent and chronological manner? | 48 | 71 | 23 |
4. Discussion
We aimed to evaluate whether a standardised surgical admissions proforma improved the completeness of patient records. We also assessed whether the implementation of a proforma makes it easier for healthcare professional to take coherent notes. This study illustrates that a surgical clerking proforma improves the quality of patient documentation, which is consistent with previous studies [2], [7], [8], [9].
The need for complete and coherent clerking notes is key, since this often forms the basis of information whilst the patient is hospitalised. Clerking notes are a routinely accessible source of the patient's hospital record, their clinical record and their immediate care plans. Indeed, one of the leading causes of unnecessary repeat lab tests is a lack of awareness about previous requests for the same test [10]. Ensuring this information is readily available to clinician is the only way to prevent such inefficiencies. As demonstrated in this study, the documentation of investigations performed increased from 57% to 87% following implementation of the clerking proforma.
Use of structured proformas, as opposed to free lined-sheets, can have the added benefits of ease of access of information, which can in turn improve efficiency. They not only improve the ease of finding information but also avoid delays in the clinical setting [8], [11]. Similarly, consistent use of subheadings in the same structure reduce the likelihood of the unnecessary error associated with healthcare professionals forgetting to enquire. Previous work has shown that the performance of the clerking clinician has improved following the introduction of a standardised proforma [1], which raises questions regarding the true extent of the impact of clear notes on patient outcomes.
This study showed dramatic improvements in documentation of height, weight, occupation, investigations performed and medication history, all of which have implications on patient care. Height (0%), weight (34%) and patient occupation (4%) were among the most under-documented categories before implementation. Weight monitoring was a particular area of concern, since administration of the correct drug dosage is often dependent on this information [12]. The under-reporting of occupational information also demonstrates a disregard for the fact that surgery can cause significant delays in returning to the workplace.
This study's initial questionnaire highlighted that over half of healthcare professionals involved with a particular patient's care deemed notes to be unstructured, with almost a quarter having visited archived notes for clarification of information. As shown in this study, use of structured clerking documents increases the quantity of information available, and the perceived reliability of the notes. In doing so, this study's results have suggested that healthcare professionals are spending less time clarifying information with archived records and colleagues. The importance of this potential benefit cannot be understated. This has knock-on effects on the speed at which investigations and treatments can be ordered. Although the implemented proforma did not eliminate the need to consult colleagues regarding patient information, it included the name, grade, date and phone/bleep number of the clerking professional, making it very easy to identify who needs to be contacted.
This study does have some methodological limitations, not least the small sample sizes. Due to short timeframe the audit was conducted over, the total number of notes available for assessment was limited to the number of admissions over the 2 one-week periods. The small sample sizes restrict its ability to accurately identify differences in documentation rates. Secondly, many of the proformas were accompanied with free hand notes, with a few doctors saying that there was ‘not enough space on the proforma to write down all the information’. This could negate any benefit in time saved in the accessibility of the notes, although future consultations with staff could allow a restructuring of the proforma to accommodate this criticism. Furthermore, a challenge faced during the evaluation of healthcare professionals' view of the notes was that not all of the staff had necessarily seen the proforma by the time they were questioned, and were potentially commenting on their wider, perhaps more established, views on notes. This limited the ability to truly identify whether staff found the introduction of a standardised clerking proforma beneficial compared to free-hand notes.
Whilst this study demonstrated an improvement in the quality and quantity of information documented, it was not designed to elicit the impact it can have on patient outcomes, which is ultimately the goal with healthcare intervention. Standardised proformas may also impact the productivity of staff, although again this study did not directly evaluate this. Further audits are required to demonstrate whether these advantages can be achieved with standardised clerking proformas. In future, such hand-written clerking may be replaced by electronic records, which may make it far easier to access patient records and avoid paper work. A better approach is however needed in the meantime.
In conclusion, our study illustrates that a comprehensive surgical clerking proforma improves patient data documentation. The implications of such work are far reaching, from patient safety to staff productivity. If well implemented, the use of a surgical clerking proforma could lay a sturdy foundation on which to conduct further clinical audits.
Ethical approval
This study was approved by the ethics committee at Northwick Park Hospital and the research undertaken was in accord with the principles outlined in the Declaration of Helsinki.
Sources of funding
None.
Author contribution
Jordan Abdi.
Role: Data collection, data analysis, proforma designer and author (role in drafting and revising the report).
Prashant Bamania.
Role: Data collection, proforma designer and author (role in drafting and revising the report).
Kunal Bhanot.
Role: Data collection, proforma designer and author (role in drafting and revising the report).
Maria Samuel.
Role: Supervisor (role in data analysis and write up).
Josef Watfah.
Role: Supervisor (oversaw running of audit: data collection, proforma design and write up).
Conflicts of interest
All authors report no conflicts of interest.
Guarantor
Kunal Bhanot.
Josef Watfah.
Consent
Not required.
References
- 1.Mann R., Williams J. Standards in medical record keeping. Clin. Med. 2003;3(4):329–332. doi: 10.7861/clinmedicine.3-4-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pullen I., Loudon J. Improving standards in clinical record-keeping. Adv. Psychiatric Treat. 2006;12(4):280–286. http://apt.rcpsych.org/content/12/4/280.abstract Available from: [Google Scholar]
- 3.Guidelines for Clinicians on Medical Records and Notes. The Royal College of Surgeons of England; 1990. [PubMed] [Google Scholar]
- 4.Osborn G.D., Pike H., Smith M., Winter R., Vaughan-Williams E. Quality of clinical case note entries: how good are we at achieving set standards? Ann. R. Coll. Surg. Engl. 2005;87(6):458–460. doi: 10.1308/003588405X60632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho M.Y., Anderson A.R., Nijjar A., Thomas C., Goenka A., Hossain J., Curley P.J. Use of the CRABEL Score for improving surgical case-note quality. Ann. R. Coll. Surg. Engl. 2005;87(6):454–457. doi: 10.1308/003588405X60687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'driscoll R., Al-Nuaimi D. Medical admission records can be improved by the use of a structured proforma. Clin. Med. 2003;3(4):385–386. doi: 10.7861/clinmedicine.3-4-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehsanullah Jasmine, Ahmad Umar, Solanki Kohmal, Healy Justin, Kadoglou Naim. The surgical admissions proforma: does it make a difference? Ann. Med. Surg. 2015;4(1):53–57. doi: 10.1016/j.amsu.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irtiza-Ali A., Houghton C.M., Raghuram A., O'Driscoll B.R. Medical admissions can be made easier, quicker and better by the use of a pre-printed medical admission proforma. Clin. Med. Lond. Engl. 2001;1(4):327. doi: 10.7861/clinmedicine.1-4-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diver A.J., Craig B.F. Admission proforma significantly improves the medical record. Scott. Med. J. 2005;50(3):101–102. doi: 10.1177/003693300505000304. [DOI] [PubMed] [Google Scholar]
- 10.Kwok J., Jones B. Unnecessary repeat requesting of tests: an audit in a government hospital immunology laboratory. J. Clin. Pathol. 2004;58(5):457–462. doi: 10.1136/jcp.2004.021691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nygren E, Wyatt JC, Wright, Helping clinicians to find data and avoid delays, Lancet, 352(9138), 1462–1466. [DOI] [PubMed]
- 12.De Baerdemaeker Luc EC., Mortier Eric P., Struys Michel MRF. Pharmacokinetics in obese patients. Contin. Educ. Anaesth. Crit. Care Pain. 2004;4(5):152–155. [Google Scholar]