Abstract
Patient: Female, 56
Final Diagnosis: Acute fibrinous and organizing pneumonia
Symptoms: Cough • dyspnea • fever
Medication: —
Clinical Procedure: —
Specialty: Pulmonology
Objective:
Rare disease
Background:
Acute fibrinous and organizing pneumonia (AFOP) is a newly evolving rare non-infectious lung pathology, characterized by intra-alveolar fibrin balls on histology. It is often difficult to diagnose and is usually mistaken for other lung pathologies. We present an interesting case of AFOP with unusual radiologic findings and disease course.
Case Report:
A 56-year-old woman presented with a 1-day history of high-grade fever, chills, and profuse sweating. She was febrile to 101.2 degree Fahrenheit on presentation. On physical examination, she had decreased air entry in the left upper lobe of the lung. Laboratory testing showed a white cell count of 27,000 cells per microliter of blood with left shift. A chest radiograph showed a left upper lobe consolidation. Computed tomography (CT) of the chest without intravenous contrast showed advanced centrilobular emphysema and left upper lobe consolidation measuring 6.2×5.9 cm. The patient was started on antibiotics. She clinically improved and was discharged on oral antibiotics. After discharge, a trans-bronchial lung biopsy showed acute inflammatory cell infiltrate with intra-alveolar fibrin balls but no hyaline membrane formation or significant eosinophils. These findings were consistent with acute fibrinous and organizing pneumonia. However, she was subsequently lost to follow-up.
Conclusions:
Our case adds to the literature a new and unusual finding of upper lobe infiltrates, in contrast to most cases presenting as bilateral lower lobe infiltrates. In our case, symptomatic improvement after antibiotic treatment suggests a possible role of antibiotics in management of this entity.
MeSH Keywords: Fibrin, Pathology, Pneumonia
Background
Acute fibrinous and organizing pneumonia (AFOP) is an uncommon disease characterized by the deposition of fibrin in alveoli in a patchy pattern. It can present with markedly variable severity and mortality. Two forms of the disease are described: a severe form causing rapid respiratory failure, and a sub-acute form with a better outcome [1]. It can present at any age [1]. In this article, we present the case of a woman diagnosed with the sub-acute form of the disease, who recovered clinically after receiving antibiotics.
Case Report
A 56-year-old woman presented with 1-day history of high-grade fever, chills, and profuse sweating. One week prior to presentation, she had developed cough productive of greenish sputum, left-sided pleuritic chest pain, and worsening dyspnea. She denied any sick contacts, weight loss, night sweats, or recent travel. She reported a smoking history of 10 pack years. Her past medical history was unremarkable.
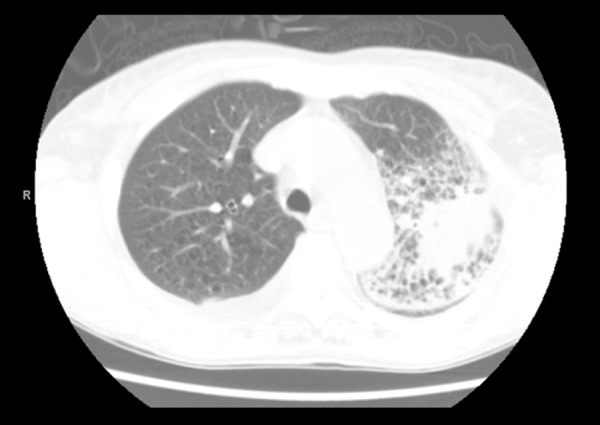
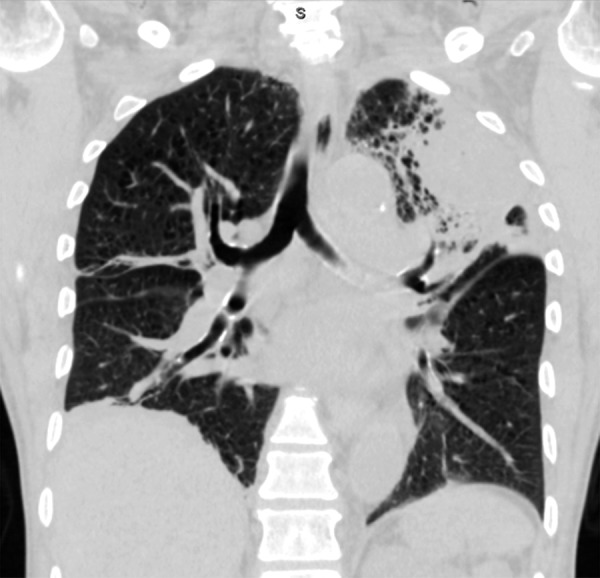
On initial evaluation, the patient was febrile to 101.2° F (38.4° C). Blood pressure was 95/50 millimeters of mercury, heart rate was 100 beats per minute, and respiratory rate was 16 breaths per minute. On physical examination, she had decreased air entry in the left upper lobe of the lung, without any adventitious sounds. The rest of the physical exam was unremarkable. Laboratory testing showed a white cell count of 27,000 cells per microliter of blood, with left shift. A chest radiograph (Figure 1) showed left upper lobe consolidation. Computed tomography (CT) of the chest without intravenous contrast (Figures 2–4) showed advanced centrilobular emphysema and left upper lobe consolidation measuring 6.2×5.9 centimeters.
Figure 1.

Postero-anterior chest radiograph showing left upper lobe consolidation.
Figure 2.
CT chest axial view at the level of aortic arch showing an advanced centrilobular emphysema, and left upper lobe consolidation, measuring 6.2×5.9 centimeters.
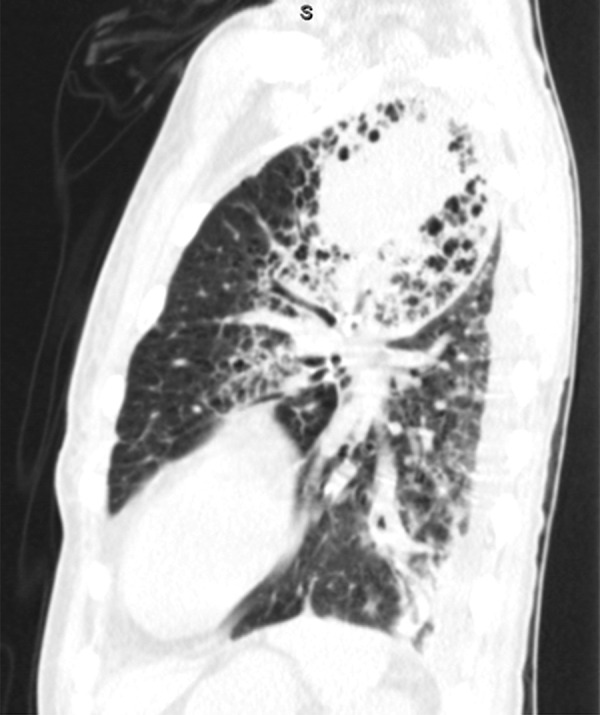
Figure 3.
CT chest showing the left upper lobe consolidation in the background of emphysema on coronal view.
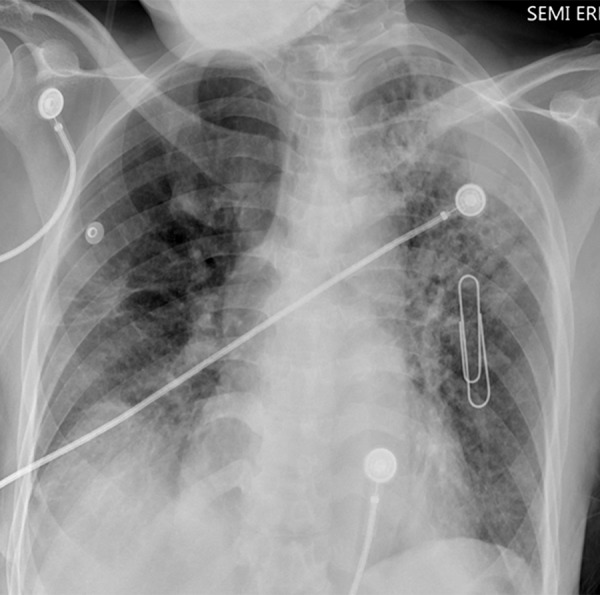
Figure 4.
CT Chest showing the left upper lobe consolidation in a lateral sagittal view.
Blood and sputum cultures remained negative. She tested negative for HIV antibodies, mycoplasma antibodies, urine legionella antigen, and sputum acid-fast bacilli. She was started on doxycycline 100 milligrams twice a day, ceftriaxone 1 gram daily, vancomycin 1 gram daily, and oseltamivir 30 milligrams twice a day. Broncho-alveolar lavage (BAL) and trans-bronchial lung biopsy were performed. BAL showed a hazy-appearing colorless fluid with white cell count of 1260 cells per cubic millimeter, mainly (94%) consisting of segmented neutrophils. Viral and bacterial cultures were negative.
The patient did not receive any steroids or immunosuppressive treatment. Five days later, fever, chills, cough, and dyspnea resolved. The white cell count decreased from 27,000 to 13,000 cells per microliter of blood. Repeated portable antero-posterior lung radiographs done after 5 days showed no change in appearance of left upper lung consolidation (Figure 5). The patient was discharged home with oral antibiotics to complete a 10-day course for pneumonia. After discharge, trans-bronchial biopsy showed acute inflammatory cell infiltrate with intra-alveolar fibrin balls without hyaline membrane formation or significant eosinophils. There were no granulomas noted. These findings were consistent with acute fibrinous and organizing pneumonia (Figures 6–8). However, the patient was lost to follow-up.
Figure 5.
Portable antero-posterior lung radiograph done after 5 days showing no change in appearance of left upper lung consolidation.
Figure 6.
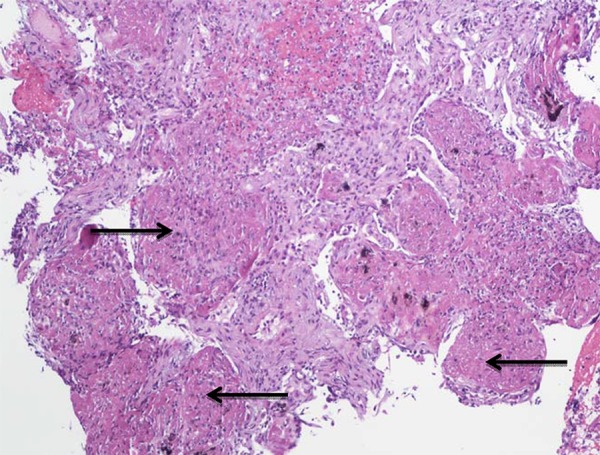
Low power magnification of AFOP showing a filling of airspaces with intra-alveolar fibrin balls.
Figure 7.
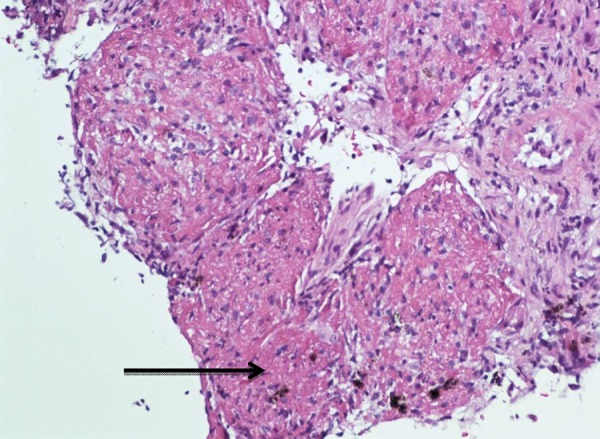
Higher power magnification showing an intra-alveolar fibrin and mild associated interstitial inflammation.
Figure 8.
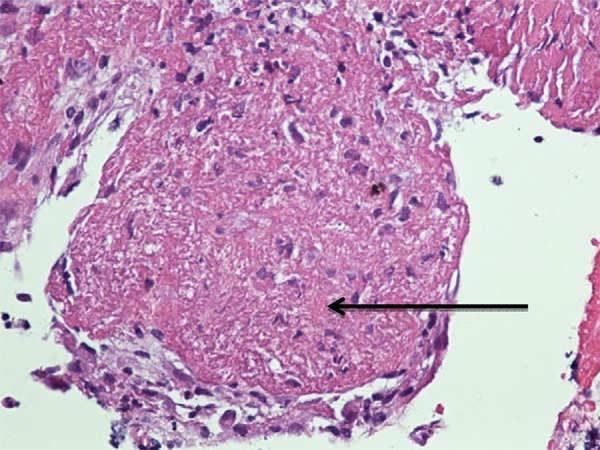
Higher power magnification showing an intra-alveolar fibrin ball without hyaline membrane formation and scant interstitial inflammatory cells, mostly lymphocytes.
Discussion
In 2002, Beasley et al. [1] described first AFOP as “a histologic pattern associated with a clinical picture of acute lung injury that differs from the classic histologic patterns of diffuse alveolar damage (DAD), bronchiolitis obliterans with organizing pneumonia (BOOP), or eosinophilic pneumonia (EP)”. Less than 120 cases were reported till 2016 [2]. In AFOP, fibrin deposits occur in intra-alveolar space and involves usually 50% of the airspace [1–3].
AFOP can be associated with a wide spectrum of clinical conditions, like collagen vascular diseases, drug reactions (amiodarone [4] and abacavir [5]), occupational or environmental exposures, as well as various infections [3,6]. Gomes et al. reported 8 cases of AFOP associated with hematologic disorders, 5 cases associated with drug-induced lung toxicity, 2 cases associated with infections, and 2 idiopathic cases [7]. Two clinical scenarios were described: the first is fulminant, often overlapping with ARDS; and the second is more sub-acute [1], with a favorable treatment response and disease progression. Fever was the most common symptom and was present in 90% of cases [8]. The presence of fibrin in organizing lesions was found to be associated with a less favorable treatment response [3,9]. Based on the clinical course of our patient, we conclude that she had the sub-acute form of the disease. She had no evidence of infection, malignancy, or any other factors known to be related with organizing pneumonia, such as collagen vascular diseases, drug-induced interstitial lung disease, or allergic reactions. This suggests an idiopathic presentation of AFOP. The most frequent radiographic abnormalities were basal/lower lobe infiltrates, predominant in 6 patients and bilateral in 8 patients, among 15 available radiologic reports [1]. In our case, an x-ray showed upper lobe infiltrate, which is very unusual.
It was thought that the pathogenesis of AFOP was due to an alveolar injury causing leakage of plasma proteins and fibrin deposition in the intra-alveolar space. This process mimics pneumonia but does not respond to antibiotics. In most cases, symptoms tend to occur gradually. However, our patient is unique in that the symptoms developed rapidly with astounding evolution of the imaging findings, and she responded to antibiotics therapy.
Various treatment modalities were tried. Beasley et al. [1] and Damas et al. [6] have successfully treated AFOP with various agents, including steroids, cyclophosphamide, or a combination of both. Cases related to allogeneic stem cell transplant were successfully treated with high-dose steroids [10]. The combination of corticosteroids and mycophenolate is safe and effective for treating severe forms of AFOP [11]. Low-dose indomethacin and methylprednisolone also showed an impressive improvement [12]. However, our patient appeared to have a regression of the disease despite receiving only antibiotics, which suggests a role of antibiotics in treatment of AFOP.
Conclusions
AFOP is a rare lung disease with varying morbidity and mortality and no definitive therapy. Our case adds to the literature a new and unusual finding of upper lobe infiltrates in contrast to most cases presenting as bilateral lower lobe infiltrates. Symptomatic improvement after antibiotic treatment suggests the possible role of antibiotics in management of this entity.
Abbreviations
- AFOP
acute fibrinous and organizing pneumonia
Footnotes
Conflict of interests
None.
References:
- 1.Beasley MB, Franks TJ, Galvin JR, et al. Acute fibrinous and organizing pneumonia: A histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med. 2002;126(9):1064–70. doi: 10.5858/2002-126-1064-AFAOP. [DOI] [PubMed] [Google Scholar]
- 2.Saxena P, Kumar K, Mittal S, et al. Acute fibrinous and organizing pneumonia: A rare form of nonbacterial pneumonia. Indian J Crit Care Med. 2016;20(4):245–47. doi: 10.4103/0972-5229.180048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cordier JF. Cryptogenic organising pneumonia. Eur Respir J. 2006;28(2):422–46. doi: 10.1183/09031936.06.00013505. [DOI] [PubMed] [Google Scholar]
- 4.Piciucchi S, Dubini A, Tomassetti S, et al. A case of amiodarone-induced acute fibrinous and organizing pneumonia mimicking mesothelioma. Am J Respir Crit Care Med. 2015;191(1):104–6. doi: 10.1164/rccm.201405-0844IM. [DOI] [PubMed] [Google Scholar]
- 5.Yokogawa N, Alcid DV. Acute fibrinous and organizing pneumonia as a rare presentation of abacavir hypersensitivity reaction. AIDS. 2007;21(15):2116–17. doi: 10.1097/QAD.0b013e3282f08c5a. [DOI] [PubMed] [Google Scholar]
- 6.Damas C, Morais A, Moura CS, Marques A. Acute fibrinous and organizing pneumonia. Rev Port Pneumol. 2006;12(5):615–20. [PubMed] [Google Scholar]
- 7.Gomes R, Padrão E, Dabó H, et al. Acute fibrinous and organizing pneumonia: A report of 13 cases in a tertiary university hospital. A. Medicine (Baltimore) 2016;95(27):e4073. doi: 10.1097/MD.0000000000004073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dai JH, Li H, Shen W, et al. Clinical and radiological profile of acute fibrinous and organizing pneumonia: A retrospective study. Chin Med J (Engl) 2015;128(20):2701–6. doi: 10.4103/0366-6999.167293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoshinouchi T, Ohtsuki Y, Kubo K, Shikata Y. Clinicopathological study on two types of cryptogenic organizing pneumonitis. Respir Med. 1995;89(4):271–78. doi: 10.1016/0954-6111(95)90087-x. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen LP, Ahdoot S, Sriratanaviriyakul N, et al. Acute fibrinous and organizing pneumonia associated with allogenic hematopoietic stem cell transplant successfully treated with corticosteroids: A two-patient case series. J Investig Med High Impact Case Rep. 2016;4(2) doi: 10.1177/2324709616643990. 2324709616643990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhatti S, Hakeem A, Torrealba J, et al. Severe acute fibrinous and organizing pneumonia (AFOP) causing ventilatory failure: Successful treatment with mycophenolate mofetil and corticosteroids. Respir Med. 2009;103(11):1764–67. doi: 10.1016/j.rmed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Zhou CX, Tang TT, Huang LJ, et al. Methylprednisolone combined with low-dose indomethacin treating acute fibrinous and organizing pneumonia after a surgical resection of rectal adenocarcinoma: A case report and literature review. Eur Rev Med Pharmacol Sci. 2016;20(10):2077–89. [PubMed] [Google Scholar]


