Abstract
Isolated patellofemoral osteoarthritis is relatively prevalent, with the lateral facet of the patella being the most commonly affected portion. This pathology can be a result of a patellar maltracking syndrome, patella instability, or idiopathic degenerative changes. A thorough diagnostic work-up with a physical examination and imaging studies are mandatory for a proper diagnosis and to rule out other causes of patellofemoral knee pain. These patients are often treated nonoperatively with exercises for patella mobility, intra-articular injections, braces, patellar tracking, quadriceps balance and strength, and activity modification. Patients with lateral patellar pain that is refractory to nonoperative management, and who have a clear bony deformity on the patella overriding the lateral aspect of the trochlea, can benefit from surgical intervention. We recommend an arthroscopic lateral patellar facetectomy because the joint can be dynamically assessed, treated, and re-evaluated intraoperatively to ensure that normal bony contact has been restored.
Isolated patellofemoral osteoarthritis (PFOA) is relatively prevalent pathology affecting 9% to 15% of patients older than 40 and 60 years, respectively.1 The medial and lateral facets of the patella can each be affected by isolated PFOA. However, isolated PFOA is most often seen in the lateral facet with up to 89% of all isolated PFOA cases seen in this portion of the patella.2 Given the considerable impact PFOA has on a patient's daily living activities including difficulty during stair ambulation and persistent anterior knee pain, effective treatment, whether nonoperative or operative, is crucial.3, 4
Nonoperative treatment options for patellofemoral pain and osteoarthritis include patellar bracing,5 physical therapy intervention,6, 7 and corticosteroid injections.8 The physical therapy protocol for relief of patellofemoral pain focuses on patellofemoral joint mobilization, patellar taping, and strengthening of the quadriceps muscle.6 Although a significant reduction in patellofemoral pain after a 6-week physical therapy regimen has been reported, this is considered a potential short-term fix for many patients.6 Ultimately, surgical treatment is necessary to provide a long-term solution.
Although more aggressive procedures including patellofemoral arthroplasty9, 10 and total knee replacement with patellar resurfacing9 can be performed in cases of isolated PFOA, we recommend an arthroscopic partial lateral patellar facetectomy, which is minimally invasive and effective in selected patients.9 This joint-preserving technique provides relief of anterior knee pain by eliminating excessive pressure on the lateral facet of the patella and improving patellar mobility. Moreover, this technique features a faster recovery period and less morbidity immediately after surgery.11 The indications for this procedure are isolated PFOA in patients with an overhanging lateral facet of the patella with anterolateral knee pain and no response to conservative treatment. The purpose of this Technical Note is to describe our technique for arthroscopic partial lateral patellar facetectomy for the treatment of isolated PFOA.
Surgical Technique
Preoperative Setup and Arthroscopic Portal Placement
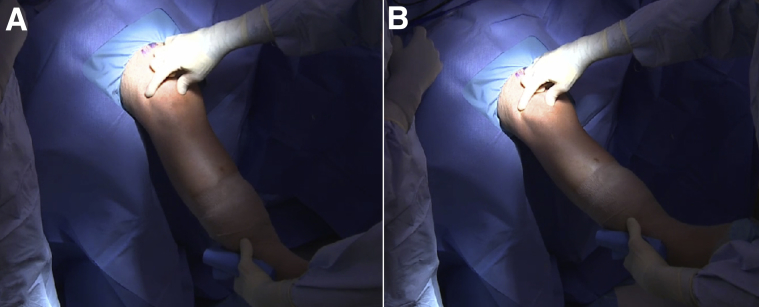
The patient is placed supine on the operating table (Video 1). After the induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent pathology and to assess for knee range of motion, patellar mobility, position, instability, and patellar crepitus during knee flexion (Fig 1). The surgical limb is placed in a leg holder (Mizuho OSI, Union City, CA). The nonoperative limb is flexed and held in an abduction holder (Birkova Product LLC, Gothenburg, NE) to avoid undesirable obstruction during the surgical procedure (Fig 2). A well-padded thigh tourniquet is placed on the upper thigh of the operative leg to maintain a bloodless field.
Fig 1.
Physical examination of patellar mobility performed in a right knee. After the induction of general anesthesia and before the tourniquet inflation, a bilateral knee examination is performed to evaluate for any concurrent pathology and to assess for knee range of motion, patellar mobility in 45° of flexion (A) and extension (B), and instability and patellar crepitus during knee flexion.
Fig 2.
The surgical limb is placed in a leg holder, whereas the nonoperative leg is flexed and held in an abduction holder to avoid undesirable obstruction during the surgical procedure. A well-padded thigh tourniquet is placed on the upper thigh of the operative leg to maintain a bloodless field. The surgical leg is prepared and draped in a sterile fashion, the leg exsanguinated, and the tourniquet inflated.
The surgical leg is prepared and draped in a sterile fashion, the leg exsanguinated, and the tourniquet inflated. Standard anterolateral and anteromedial portals are created adjacent to the patellar tendon (Fig 3). The joint is insufflated with normal saline and visualized with a 30° arthroscope (Smith & Nephew, Andover, MA). Routine diagnostic arthroscopy, examination of all the compartments of the knee, is performed to investigate for associated lesions. An arthroscopic shaver (Smith & Nephew) is inserted into the knee and any notable adhesions are removed. Any meniscal, cartilage, or ligamentous injury may be treated first. Table 1 summarizes the advantages and disadvantages of this procedure.
Fig 3.
Image showing an arthroscopic patellar facetectomy in a right knee. After preparation of the surgical limb is complete, the knee is put in 90° flexion. A standard anterolateral portal is created (A) adjacent to the patellar tendon; a 30° arthroscope is then inserted through this portal and under arthroscopic visualization of the medial femorotibial compartment an anteromedial portal (B) is created to perform the resection of the lateral facet.
Table 1.
Advantages and Disadvantages of Arthroscopic Patellar Lateral Facetectomy
| Advantages | Disadvantages |
|---|---|
| Arthroscopic procedure allows for the diagnosis and treatment of other intra-articular pathologies concurrently | Might be technically demanding for surgeons who are more comfortable completing open surgery |
| Little soft tissue disruption with arthroscopic allows for early mobilization | In untrained hands, the technique will result in a longer operative time |
| Reduces progression of erosion on the lateral femoral condyle that was caused by the bone spur | This treatment does not address generalized patellofemoral cartilage degeneration |
| Good visualization with an arthroscope is an alternative method to treat isolated patellofemoral osteoarthritis associated with overhanging lateral facet of the patella | Resection of too much lateral retinacular tissue could result in iatrogenic medial patellar instability |
| Disruption of the retinaculum can be avoided by resecting from the joint side | |
| Patellofemoral articulation can be dynamically assessed during surgery to ensure that enough resection has been performed |
Confirmation of Impingement and Bone Resection
The knee is taken throughout a range of motion to directly visualize the impingement of the lateral patellar facet against the trochlea. Next, a radiofrequency probe is used to outline the area to be resected along the lateral patellar facet (Fig 4).
Fig 4.
Arthroscopic image of the right knee showing delineation of the patellar surface to be resected with the use of a radiofrequency probe on the lateral aspect of the patella (viewed through the anteromedial portal) on a right knee. On the right, an intraoperative view of the portal setup is shown. (P, patella; RF, radiofrequency probe.)
While maintaining the knee at 20° of flexion, a 5.5-mm burr is introduced, and under arthroscopic visualization, the lateral patellar osteophyte and the overhanging portion of the lateral facet is carefully resected (Fig 5). It is preferable to start the procedure inferiorly, to obtain good visualization throughout the process. Usually, the width of a burr (5.5 mm) is the minimal amount of bone to be resected. Pearls and pitfalls for this procedure are summarized in Table 2.
Fig 5.
Arthroscopic image of the right side showing lateral patellar facetectomy using a 5.5-mm burr. Of note, progressive resection should be performed throughout the whole surface to allow for a final smooth surface after resection. On the right-hand side, the arthroscope is shown being introduced through the anteromedial portal and the burr through the anterolateral portal.
Table 2.
Pearls and Pitfalls of Arthroscopic Patellar Lateral Facetectomy
| Pearls | Pitfalls |
|---|---|
| Good preoperative diagnosis. Generalized patellofemoral osteoarthritis is a relative contraindication | Poor preoperative diagnosis and planning of how much to resect off the lateral facet |
| Good and thorough diagnostic arthroscopy to address concomitant lesions such as loose bodies, chondral flaps, and meniscal pathology | Under-resecting the bone can result in poor outcomes |
| Careful resection respecting the soft tissue | Over-resecting can compromise the soft tissue attachments laterally and can result in destabilizing the patella |
| Avoid compromising the retinaculum and the vastus lateralis attachment | Poor postoperative rehabilitation can result in poor patella motion and recurrent stiffness |
| Good postoperative rehab to regain range of motion, patella motion, and quadriceps function |
Re-evaluation of Impingement and Closure
Once the bony resection is complete, the knee is dynamically re-evaluated (through flexion and extension and with medial excursion) for residual impingement (Fig 6) and to assess for improvements in patellar mobility. Patellar tracking is assessed to verify that there is no catching in flexion and that patellar mobility is improved. If any impingement does remain, it can be addressed at this point. Moreover, a third portal can be created if access to the superolateral aspect of the patella is difficult to reach. A shaver can be used to remove the debris while trimming the lateral patellar facet. It is of utmost importance to cautiously resect any remnant bony sharp edges that can impinge on the lateral trochlear surface during knee motion. In addition, the lateral patellar retinaculum is carefully preserved so that iatrogenic medial patellar instability does not occur. Hemostasis is performed with a radiofrequency probe to minimize postoperative bleeding. Lastly, the portals are closed and a sterile compressive draping is prepared because the bone resection may produce a bloody effusion.
Fig 6.
Arthroscopic patellar lateral facetectomy performed in a right knee. Once the bony resection is complete, the knee is dynamically re-evaluated through flexion (A) and extension (B) for residual impingement and to assess for improvements in patellar mobility under arthroscopic visualization using a 30° arthroscope through the anteromedial portal. Patellar tracking is assessed to verify that there is no catching in flexion and that patellar mobility is improved. If any impingement does remain, it is addressed at this point.
Rehabilitation Protocol
After an arthroscopic patellar lateral facetectomy, there is no restriction on knee range of motion, and flexion/extension exercises are initiated as soon as possible. No brace is necessary, but crutches are required during the first week immediately after the procedure until the patient can ambulate without a limp. The patient is allowed to bear weight as tolerated during this first week. Flexion/extension exercises, patella and patellar tendon mobilization, quadriceps and hamstrings exercises, ankle pump exercises, and stationary biking with no resistance are initiated immediately after surgery through postoperative week 8. Toe and heel raises as well as balancing exercises are initiated at week 3. Then, treadmill walking with 7% incline and swimming are initiated at week 7. Later on in the rehabilitation period, single plane agility exercises are begun at week 16 and gradually progressed to multidirectional exercises at week 20. Return to sport or their desired activities is permitted, as tolerated by the patient, at postoperative week 20.
Discussion
This Technical Note describes our preferred surgical technique to treat patellofemoral pain in patients with isolated PFOA who present with an overhanging lateral facet of the patella and limited patellar mobility. PFOA can cause severe disability and, sometimes, it is more disabling than osteoarthritis in the medial tibiofemoral compartment.12 This ultimately leads to pain during activities that require a deep flexion of the knee, which results in a challenging and limiting issue especially in young and active patients.11
Nonoperative treatments, such as physiotherapy treatment, taping, intra-articular, and viscosupplementation, are described as possible initial approaches to treat PFOA.9 However, in patients with disability and pain who do not respond to conservative treatment, surgical treatment may be required.9
Patellofemoral arthroplasty and total knee arthroplasty with patellar resurfacing have been previously reported as possible surgical treatment options with improved patient outcomes.9, 13 However, these procedures are more invasive and are associated with more complications.14
Patellar lateral facetectomy is described in the literature as a safe procedure to treat isolated PFOA, and it does not affect a potential patellar replacement, if needed.15 Marten and De Rycke16 reported good-to-moderate results in 90% of 20 patients in a prospective case series, with a mean follow-up of 2 years. Furthermore, functional improvement has been reported to be maintained for a long-term period.17 Interestingly, medial tibiofemoral pain, loss of extension, and a low clinical score for tibiofemoral osteoarthritis were reported as significant risk factors for failure of the procedure.18
When analyzing the treatment of patients with isolated PFOA via open lateral facetectomy, lateral release, and tibial tubercle medialization, Becker et al.11 reported that the results were not significantly greater than isolated facetectomy. As a result, the authors did not recommend this combination of procedures for young and middle-age patients with isolated PFOA until further studies with longer-term follow-up have been completed.
In conclusion, in accordance with positive clinical outcomes seen in the literature and our clinical experience, we recommend our approach for treatment of isolated PFOA in patients with an overhanging lateral facet of the patella and anterior knee pain. Nevertheless, future long-term studies with large sample sizes are needed to further assess the efficacy of this procedure in comparison with more aggressive approaches.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: G.M. receives research grants from Health South East, Norway, and Arthrex. R.F.L. receives support from Smith & Nephew Endoscopy, Ossur Americas, Arthrex, Siemens Medical Solutions USA, Small Bone Innovations, ConMed Linvatec, and Opedix; he is on the editorial/governing board for AJSM and KSSTA, and has member/committee appointments with AOSSM, ISAKOS, AANA, and ESSKA.
Supplementary Data
The patient is placed supine on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent pathology and to assess for knee range of motion, patellar mobility, instability, or crepitus. The surgical limb is placed in a leg holder and the nonoperative leg is flexed and held in an abduction holder. A well-padded thigh tourniquet is placed on the upper thigh of the operative leg to maintain a bloodless field. The surgical leg is prepped and draped in a sterile fashion, the leg exsanguinated, and the tourniquet inflated. Standard anterolateral and anteromedial portals are now performed. The joint is insufflated with normal saline and visualized with a 30° arthroscope through the anterolateral portal. An arthroscopic shaver is inserted through the anteromedial portal into the knee and any notable adhesions or loose bodies are removed. All compartments of the knee are explored, and if there are any concomitant pathologies, they are addressed at this time. The knee is flexed and extended to directly visualize the impingement of the lateral patellar facet and the amount of overriding bone against the lateral aspect of the trochlea, as well as the chondral lesion. Next, a radiofrequency probe is used to outline the area to be resected along the lateral patella. Of note, care should be taken not to make damage to the lateral retinaculum. While maintaining the knee at 20° of flexion, a 5.5-mm burr is introduced through the anterolateral portal, and under arthroscopic visualization from the anteromedial portal, the lateral patellar osteophyte is carefully resected. Once resection is complete, the knee is dynamically re-evaluated for residual impingement and to ensure that patellar mobility is improved. Patellar tracking is assessed to verify that there is no catching in flexion. If any impingement does remain, it can be addressed at this point. Hemostasis is performed with a radiofrequency probe to avoid postoperative bleeding. The skin is closed and the procedure is complete.
References
- 1.Davies A.P., Vince A.S., Shepstone L., Donell S.T., Glasgow M.M. The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res. 2002;(402):206–212. doi: 10.1097/00003086-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Iwano T., Kurosawa H., Tokuyama H., Hoshikawa Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990;(252):190–197. [PubMed] [Google Scholar]
- 3.Schiphof D., van Middelkoop M., de Klerk B.M. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthritis Cartilage. 2014;22:631–638. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Mills K., Hunter D.J. Patellofemoral joint osteoarthritis: An individualised pathomechanical approach to management. Best Pract Res Clin Rheumatol. 2014;28:73–91. doi: 10.1016/j.berh.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Callaghan M.J., Parkes M.J., Hutchinson C.E. A randomised trial of a brace for patellofemoral osteoarthritis targeting knee pain and bone marrow lesions. Ann Rheum Dis. 2015;74:1164–1170. doi: 10.1136/annrheumdis-2014-206376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crossley K., Bennell K., Green S., Cowan S., McConnell J. Physical therapy for patellofemoral pain: A randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30:857–865. doi: 10.1177/03635465020300061701. [DOI] [PubMed] [Google Scholar]
- 7.Lun V.M., Wiley J.P., Meeuwisse W.H., Yanagawa T.L. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15:235–240. doi: 10.1097/01.jsm.0000171258.16941.13. [DOI] [PubMed] [Google Scholar]
- 8.Arroll B., Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: Meta-analysis. BMJ. 2004;328:869. doi: 10.1136/bmj.38039.573970.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Jonbergen H.P., Poolman R.W., van Kampen A. Isolated patellofemoral osteoarthritis. Acta Orthop. 2010;81:199–205. doi: 10.3109/17453671003628756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arciero R.A., Toomey H.E. Patellofemoral arthroplasty. A three- to nine-year follow-up study. Clin Orthop Relat Res. 1988;(236):60–71. [PubMed] [Google Scholar]
- 11.Becker R., Ropke M., Krull A., Musahl V., Nebelung W. Surgical treatment of isolated patellofemoral osteoarthritis. Clin Orthop Relat Res. 2008;466:443–449. doi: 10.1007/s11999-007-0071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McAlindon T.E., Snow S., Cooper C., Dieppe P.A. Radiographic patterns of osteoarthritis of the knee joint in the community: The importance of the patellofemoral joint. Ann Rheum Dis. 1992;51:844–849. doi: 10.1136/ard.51.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der List JP, Chawla H, Zuiderbaan HA, Pearle AD. Survivorship and functional outcomes of patellofemoral arthroplasty: A systematic review [published online November 21, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3878-z. [DOI] [PubMed]
- 14.Dy C.J., Franco N., Ma Y., Mazumdar M., McCarthy M.M., Gonzalez Della Valle A. Complications after patello-femoral versus total knee replacement in the treatment of isolated patello-femoral osteoarthritis. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20:2174–2190. doi: 10.1007/s00167-011-1677-8. [DOI] [PubMed] [Google Scholar]
- 15.Donell S.T., Glasgow M.M. Isolated patellofemoral osteoarthritis. Knee. 2007;14:169–176. doi: 10.1016/j.knee.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Martens M., De Rycke J. Facetectomy of the patella in patellofemoral osteoarthritis. Acta Orthop Belg. 1990;56:563–567. [PubMed] [Google Scholar]
- 17.Yercan H.S., Ait Si Selmi T., Neyret P. The treatment of patellofemoral osteoarthritis with partial lateral facetectomy. Clin Orthop Relat Res. 2005;(436):14–19. doi: 10.1097/00003086-200507000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Montserrat F., Alentorn-Geli E., Leon V., Gines-Cespedosa A., Rigol P. Partial lateral facetectomy plus Insall's procedure for the treatment of isolated patellofemoral osteoarthritis: Survival analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:88–96. doi: 10.1007/s00167-012-2286-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed supine on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent pathology and to assess for knee range of motion, patellar mobility, instability, or crepitus. The surgical limb is placed in a leg holder and the nonoperative leg is flexed and held in an abduction holder. A well-padded thigh tourniquet is placed on the upper thigh of the operative leg to maintain a bloodless field. The surgical leg is prepped and draped in a sterile fashion, the leg exsanguinated, and the tourniquet inflated. Standard anterolateral and anteromedial portals are now performed. The joint is insufflated with normal saline and visualized with a 30° arthroscope through the anterolateral portal. An arthroscopic shaver is inserted through the anteromedial portal into the knee and any notable adhesions or loose bodies are removed. All compartments of the knee are explored, and if there are any concomitant pathologies, they are addressed at this time. The knee is flexed and extended to directly visualize the impingement of the lateral patellar facet and the amount of overriding bone against the lateral aspect of the trochlea, as well as the chondral lesion. Next, a radiofrequency probe is used to outline the area to be resected along the lateral patella. Of note, care should be taken not to make damage to the lateral retinaculum. While maintaining the knee at 20° of flexion, a 5.5-mm burr is introduced through the anterolateral portal, and under arthroscopic visualization from the anteromedial portal, the lateral patellar osteophyte is carefully resected. Once resection is complete, the knee is dynamically re-evaluated for residual impingement and to ensure that patellar mobility is improved. Patellar tracking is assessed to verify that there is no catching in flexion. If any impingement does remain, it can be addressed at this point. Hemostasis is performed with a radiofrequency probe to avoid postoperative bleeding. The skin is closed and the procedure is complete.