Abstract
Background:
Postmenopausal women experience a variety of symptoms, among which sleep disorder is one of the most common problems. Acupressure and Pilates exercise programs are effective nonpharmaceutical treatments which can improve sleep quality. In the present study, we aimed to compare the effects of acupressure and Pilates-based exercises on the sleep quality of postmenopausal women referred to medical clinics.
Materials and Methods:
In this single-blinded randomized controlled clinical trial, we recruited 108 women aged 40–60 years who were randomly assigned into one control and two intervention groups using balanced block randomization method (three groups of 36 each). The patients in the Pilates exercise group participated in an exercise training program of three 1-hour sessions per week for 6 consecutive weeks. The participants of acupressure group received acupressure intervention three times a week for 6 weeks. The sleep quality of all participants was assessed and recorded using the Pittsburgh Sleep Quality Index (PSQI) once before and once after the intervention.
Results:
The results showed no statistically significant difference among the three groups on the total scores of sleep quality after the intervention. The intragroup comparison revealed that the changes in the mean total scores were significant in both the intervention groups (P < 0.001) but not in the control group (P = 0.76).
Conclusions:
Pilates-based exercises and acupressure can effectively improve women's sleep quality. Both techniques can be applied as effective alternative and complementary methods for improving sleep quality during the postmenopausal period.
Keywords: Acupressure, exercise movement techniques, Iran, post menopause, sleep
Introduction
Menopause is a normal and important aging phenomenon that occurs in women's life. It also causes a transition to a new biological situation which results in a gradual loss of fertility.[1,2] Transition to menopause starts with a change in menstrual cycle length of more than 7 days different from the normal length in the presence of high levels of follicle-stimulating hormone. Menopause, which is diagnosed after 12 months of amenorrhea, marks the end of menstrual cycles.[3]
Menopause is a manifestation of aging as well as a predictor of diseases and health-related problems in old ages.[2] During this period, reduced ovarian activity is associated with reduction in hormone levels, hot flashes, menstrual disorders, feeling a constant urge to urinate, urinary bladder inflammation, and being prone to urinary tract infections.[4] It typically occurs in women aged between 40 and 60 years. At present, the average age of menopause in women is 51 years.[5]
The various complications experienced by postmenopausal women are divided into short-term and long-term types. Short-term complications include vasomotor symptoms (hot flashes and night sweats that affect 80% of women at some point in the menopausal transition) and physical symptoms (including cardiac diseases, sleep disturbances, joint and muscle pain, and urogenital symptoms such as sexual and urinary bladder problems) as well as psychological problems (depression, irritability, mood swings, anxiety, dysphoria, feelings of sadness, and restlessness). However, long-term complications include cardiovascular diseases and osteoporosis.[6,7]
In general, 30–40% of postmenopausal women suffer from psychosocial problems such as fatigue and insomnia.[8] Moreover, the prevalence of symptoms among such women has been reported up to 65%. Several factors can affect sleep disorders in postmenopausal women. Among these factors, which cause sleep disorders in such women, snoring is more common. As women age, their sleep becomes lighter. Hot flashes and night sweats also intensify the problem.[9]
Hypnotic drugs are known as the first-line treatment of insomnia. However, such medications have serious potential side effects that can be minimized by using nonpharmaceutical methods.[10,11]
Acupressure is one of the mentioned methods. This alternative medicine technique is derived from acupuncture therapy, in which the acupuncture points are stimulated using finger and palm pressure.[12] Energy channels (usually called meridians) start at the direction of pressure points on the skin and then connect to the brain and a particular meridian associated with a specific organ. Meridians are distinct channels which circulate electrical energy throughout the body. A master communication system of life energy helps to achieve a better connection of the organs with all sensory, physiological, and emotional aspects of the body.[13]
Similar to acupuncture, this technique can effectively cause muscle relaxation, decrease pain, and increase comfort by raising the level of endorphins in the brain. It also regulates physical mechanisms that induce muscle relaxation and improve sleep quality.[12] Manipulating this pressure point can strengthen, relax, and spread Chi, which is the fundamental life energy, such that it can ultimately flow easily and smoothly throughout the body. Accordingly, a balanced and harmonious relationship between the mind and body is created which, in turn, can reduce or eliminate the symptoms and complications of the disease.[11]
Acupressure is now used increasingly because it is inexpensive and does not require specialized equipment. It is also an effective, safe, quick, and noninvasive treatment.[14] Moreover, it can be easily applied and learned. Nurses are in an excellent position to apply such techniques. Furthermore, because many patients become nervous when facing the needle, acupressure is a more convenient alternative to acupuncture.[12]
Pilates-based exercise is another nonpharmaceutical approach. Pilates (or Contrology) is defined as the complete coordination of body, mind, and spirit. During the exercise sessions, individuals initially take complete control of their own body through Contrology in a purposeful manner and then achieve a normal coordination by repeating exercises gradually and progressively.[15] Pilates-based exercise program has been approved by physicians as a unique method of physical fitness in which a combination of techniques, such as muscle strengthening, lengthening, and breathing, has been used to develop trunk muscles and restore muscle balance.[16]
Unlike traditional resistance exercises in which the muscles are trained in isolation, such program needs activation and coordination of several muscle groups at a same time with a holistic approach.[17] Contrology fosters coordination among body organs, modifies incorrect body position and movement, restores life energy to the body, and increases mental capacity. Pilates-based exercises are trained in a manner that helps prevent sports injuries.[18] Both acupressure and Pilates exercise program create a balanced and harmonious relationship between the body and mind.
Nordio and Romanelli consider stimulation of wrist acupoint (Shenman point) as a reliable and effective method without any side effects.[19] Another study proved the efficacy of acupressure in the treatment of cancer-related insomnia.[20] The results of several studies showed that acupressure and acupuncture techniques can lead to the release of neurotransmitters, such as serotonin, which induce a sense of relaxation.[21] Another study reported that certain peptides are released during acupuncture which have analgesic and sedative effects.[22]
Considering the high prevalence of sleep disorders among women and the lack of clinical trials available on Pilates-based exercises in the field of nursing science and gynecology, the researchers attempted to establish a connection between the mentioned sciences and traditional medicine by relying on authentic and reliable scientific articles and teachings of traditional medicine elders. In the present study, we aimed to compare the effects of acupressure and Pilates-based exercises on sleep quality of postmenopausal women, aged 40–60 years who were referred to medical clinics affiliated to the Shiraz University of Medical Sciences in 2014.
Materials and Methods
This study was a single-blinded randomized controlled clinical trial registered in the registry of clinical trials (IRCT registration number: IRCT2014042017344N1) 2014 year of the study. After obtaining approval from the Ethics Committee of Shiraz University of Medical Sciences, we recruited all 108 women aged 40–60 years who were referred to Motahari, Imam Reza, Hafez, and Zeynabiyeh medical clinics affiliated to the Shiraz University of Medical Sciences in Shiraz, southwest Iran, during May to September 2014. Afterwards, the participants were randomly assigned into one control and two intervention groups using a balanced block randomization method (three groups of 36 each) [Figure 1].
Figure 1.
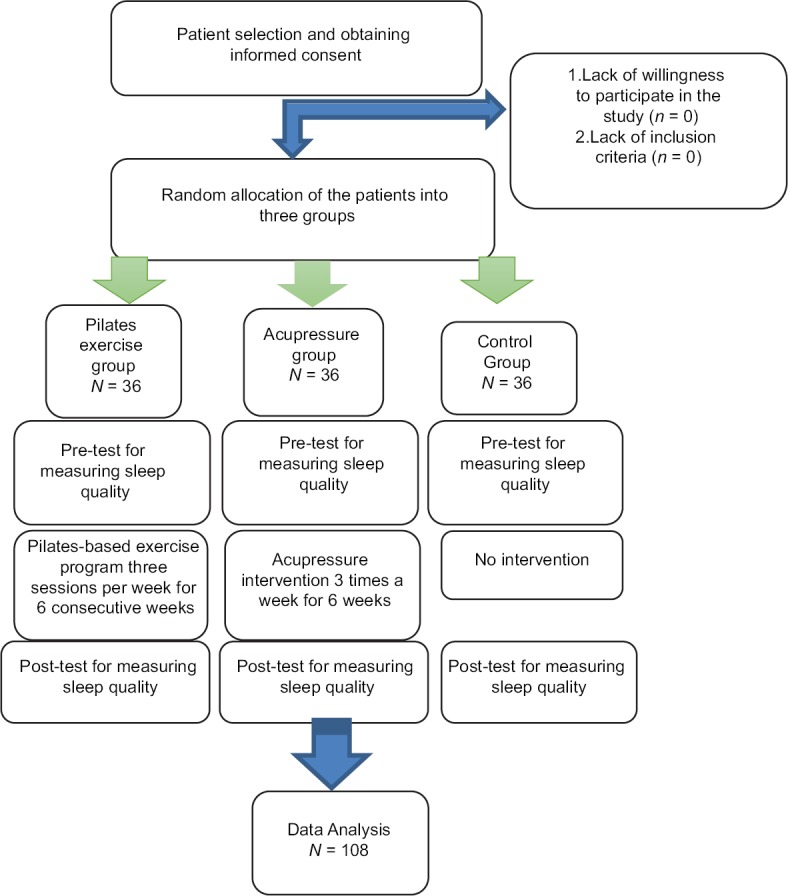
Flow Diagram for progression of participants through a Randomized Clinical Trial
Inclusion criteria were age ranging 40–60 years; willingness to participate in the study; cessation of menstrual periods for at least 12 months before the reference date; natural menopause; lack of any diseases including insulin-dependent diabetes, cancer, lupus, heart failure, severe pulmonary diseases, anxiety-producing diseases, mental and physical disabilities and chronic pain; scored 5 or above on the Pittsburgh Sleep Quality Index (PSQI), having full consciousness; and an acceptable ability of listening and speaking. Exclusion criteria were absence of more than two sessions and acute diseases requiring hospitalization.
The sample size was calculated to be 36 in each group based on the data of a similar study by Basampur et al. and the following formula using Power PASS statistical software (Power: 80%; α : 0.05; mean difference: 3.1; loss rate: 10% and MAX integrated SD: 1.6; minimum effect size: 1).[23]
Data were collected using a demographic and PSQI questionnaires. Demographic data included age, educational level, employment status, history of diseases, and menopausal status. PSQI is a self-report questionnaire that assesses the sleep quality of an individual over a 1-month interval. It comprises 9 questions measuring seven components including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disorder (sleep fragmentation), use of sleeping medication, and daytime dysfunction. Obtained score ranges from 1 to 21, whereby a score of ≥5 indicates poor quality of sleep. Scientific validity of the index has been confirmed by several studies using content validity.[24] Malekzadegan and Moradkhani determined the scale's validity and reliability by content validity and test–retest methods, respectively.[25]
After explaining the purpose and method of the study, written informed consent was obtained from all the participants who met the inclusion criteria, and their anonymity and confidentiality were guaranteed. The participants were assured that their participation was voluntary and that they could withdraw from the study, if they desired, at any time without any consequences.
The patients in the Pilates exercise group participated in an exercise training program of three 1-hour sessions per week for 6 consecutive weeks. The participants of the acupressure group received acupressure intervention 3 times a week for 6 weeks so that their wrist acupoints (hand Shenmen) was pressed by finger pressure of 3 kg/cm2 for 5 minutes continuously. Participants in the control group received no intervention. The sleep quality of all participants was assessed and recorded using PSQI by a research assistant, who was blind to group allocation, once at the enrollment and once after the 6th week of the intervention.
The collected data were analyzed using SPSS software, version 16 (version 16, SPSS, Inc, chicago, USA). Statistical descriptive tests, Chi-square test, independent and paired t-tests, one-way analysis of variance (one-way ANOVA) and post-hoc multiple comparisons (Tukey's or Dunnett's), as well as non-parametric tests were used as appropriate. The significance level was set at <0.05.
Ethical considerations
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran (Ethics Committee Approval Number: 6982). All the participants were informed about the study objectives and signed written informed consents for taking part in the study. They were also reassured that not participating in the study had no effects on their status. Besides, they were free to leave the study at any time. Moreover, the participants' privacy and confidentiality were observed all through the study Maryam Ahmadinezhad.
Results
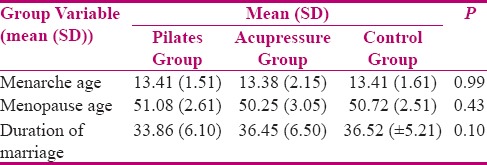
The participants were in the age range of 40–60 years and their mean (SD) ages was 54.08 (3.84). There was no significant difference between the three groups with respect to their mean age, educational level, employment status, the mean age of menarche and menopause, as well as the duration of marriage (P > 0.05). Majority of the participants were married (95.37%) and housewives (90.74%). The mean (SD) age of menarche was 13.41 (1.51), 13.38 (2.15), and 13.41 (1.61) in the Pilates, acupressure, and control groups, respectively. Furthermore, the mean (SD) age of menopause was 51.08 (2.61), 50.25 (3.05), and 50.72 (2.51) in the Pilates, acupressure, and control groups, respectively. Accordingly, we found no significant difference between the groups with respect to the mean age of menarche and menopause and the duration of marriage (P > 0.05) [Table 1].
Table 1.
Comparison of the mean (SD) age of menarche, menopause and duration of marriage between the groups
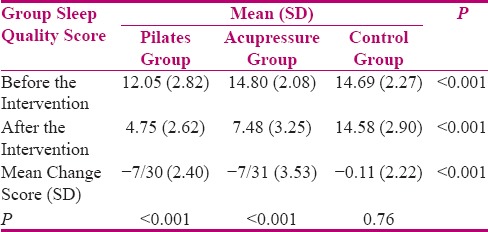
One-way ANOVA and post-hoc tests were used to investigate the differences among the three groups on total scores of sleep quality before and after the intervention. The results showed statistically significant difference among the three groups in this regard (P < 0.001). Moreover, there was a statistically significant difference between the Pilates and acupressure groups (P < 0.001) and between the Pilates and control groups (P < 0.001) before the intervention. A significant difference was also observed between each pair of groups after the intervention (P < 0.001). The intragroup comparison with paired t-test revealed that the changes in the mean total scores were significant in both the intervention groups (P < 0.001) but not in the control group (P = 0.76).
The differences were compared using one-way ANOVA and Tukey's post-hoc tests to compare the changes among the three groups. The obtained results indicated that the differences observed among the three groups were significant due to the differences between the Pilates and control groups (P < 0.001) and those between the acupressure and control groups (P < 0.001). The mean total scores significantly decreased in the Pilates and acupressure groups after the intervention (P < 0.001). However, the difference between the two intervention groups was not statistically significant (P > 0.999) reflecting that the two interventions had almost similar effects on decreasing sleep quality scores [Table 2].
Table 2.
Comparison of the mean (SD) scores of sleep quality between the groups before and after the intervention
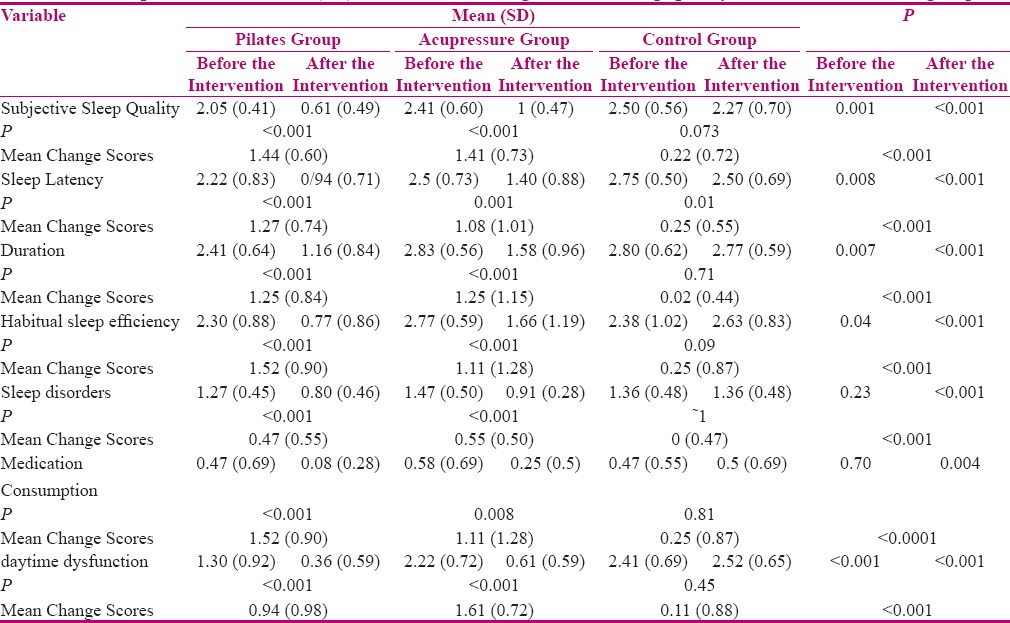
The differences between the three groups in all subscales were significant due to the differences between the Pilates and control groups (P < 0.001) and those between acupressure and control groups (P < 0.001). The difference between the Pilates and acupressure groups was only significant in the subscale of dysfunction (P = 0/005). Our results showed that acupressure could decrease total score of PSQI and its subscales including sleep quality (P < 0.001), sleep latency (P = 0.001), sleep duration (P < 0.001), habitual sleep efficiency (P = 0.001), sleep disorders (P < 0.001), sleep medication consumption (P < 0.008), and daytime dysfunction (P < 0.001). Pilates-based exercise program could also reduce the total score of PSQI and its subscales including subjective sleep quality (P < 0.001), sleep latency (P < 0.001), sleep duration (P < 0.001), habitual sleep efficiency (P < 0.001), sleep disorders (P < 0.001), sleep medication consumption (P < 0.001), and daytime dysfunction (P < 0.001) [Table 3].
Table 3.
Comparison of the mean (SD) and the mean change scores of sleep quality subscales between the groups
Discussion
Postmenopausal women experience a variety of symptoms, among which insomnia is more common and cause disruptions in the sufferers' social, family, and occupational life. Almost 50% of postmenopausal women suffer from sleep disorders which can negatively affect their quality of life.[26] Considering the growing population of postmenopausal women, raising the level of their health seems quite important. Currently, several therapeutic methods have been employed in the treatment and management of insomnia, among which pharmaceutical treatment has been the most commonly used.[27] Because of various side effects such medications may cause, recently nonpharmaceutical interventions have been strongly recommended.
According to traditional Chinese medicine, there are several acupoints on human's body, such as Shenman, Yanglingquan, and Anmian, and stimulating them can help to induce sedation and improve sleep quality. Similarly, stimulation of Fengchi, Shenman, Yanglingquan, and Anmian acupoints increase the brain's levels of serotonin and melatonin, induce relaxation, and naturally enhance sleep quality.[28,29]
Furthermore, several studies have shown that taking deep diaphragmatic breaths during Pilates exercise program helps to control stress, and thereby reduces sympathetic nerve activity, which is effective in recovery of health-related symptoms such as sleep disorder.[30]
Intergroup comparison showed no significant difference between the two intervention groups indicating that both acupressure and Pilates-based interventions had almost similar effects on increasing sleep quality scores (P ~ 1). There was also no significant difference between the groups with respect to the mean scores of sleep quality subscales, except the subscale of daytime dysfunction, reflecting that Pilates-based exercises were more effective than acupressure in improving daily functioning.
Many studies have confirmed the effectiveness of Pilates-based exercises and acupressure in improving sleep quality. Similar to our findings, Mohammad et al. demonstrated the positive effects of Pilates-based exercises on sleep quality.[31] Arab et al. also reported that acupressure intervention could decrease the total score of PSQI and its subscales including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disorders, and daytime dysfunction.[32]
Similarly, Hoseinabadi et al.[24] proved the effect of acupressure on sleep quality in Iranian elderly nursing home residents. A review article on acupuncture analgesia revealed that acupressure on the Shenman point could improve insomnia up to 2 weeks after the intervention.[12] Moreover, Caldwell et al.[33] proved that Pilates exercise is an effective intervention, which can help to improve mental parameters in college-age individuals. Likewise, we can conclude that Pilates-based exercises can positively affect sleep quality, mood, and self-efficacy (mental parameters) in all age groups.
The results of the present study showed a significant improvement in our participants sleep quality after a 12-week intervention. Our findings were consistent with those of Leopoldino et al.[34] who studied the effect of Pilates exercises on sleep quality in a sedentary population and found that their sleep quality significantly improved after the exercise program. Similarly, in a study by Rizk, sleep problems significantly improved among the participants of the intervention group as either absent or mild among the majority (80–85%) compared to only 20–25% of their peers in the control group after 2 and 3 weeks of intervention, respectively.[35]
Various studies have also reported that energy level rises by taking deep diaphragmatic breaths while exercising as active muscles and other involved respiratory muscles begin to consume energy. Moreover, deep breathing increases oxygen delivery to active muscles and oxidation of fat cells, lowers estrogen, and increases progesterone levels.[36] Accordingly, it can improve individuals' psychological symptoms as well as their sleep quality.[37] It seems that physical activity can improve sleep-affecting mood symptoms (stress and anxiety) through the mechanism which affects brain endorphins.[38]
The results of the present study indicate that Pilates-based exercises and acupressure can both be applied in all therapeutic, preventive, and supportive fields as effective alternative and complementary methods. Such techniques can improve sleep quality and reduce the complications caused by drug use and dependence.
Conclusion
It can be concluded that Pilates-based exercises and acupressure can effectively improve sleep quality. Considering the efficacy and novelty of these approaches in Iran, it seems that proposing and applying such methods in the treatment of insomnia not only would be welcomed by clinicians but can also be used as a background for further and broader studies. Considering special attention that has been recently paid to women, the results of the present study helps to take effective steps to improve women's health.
Financial support and sponsorship
Vice Chancellor for Research Affairs, Shiraz University of Medical Sciences (Grant No: 6982).
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This manuscript has been derived from the dissertation of Ms. Maryam Ahmadinejad for the Master's degree in community health nursing. This study was financially supported by Vice Chancellor for Research Affairs, Shiraz University of Medical Sciences (Grant No: 6982). The authors hereby thank all the respected officials of Vice Chancellor for Research Affairs of Shiraz University of Medical Sciences, the officials of medical clinics affiliated to Shiraz University of Medical Sciences and the patients who took part in this investigation.
References
- 1.Staessen J, Celis H, Fagard R. The epidemiology of the association between hypertension and menopause. J Hum Hypertens. 1998;12:587–92. doi: 10.1038/sj.jhh.1000670. [DOI] [PubMed] [Google Scholar]
- 2.Pérez JAM, Garcia FC, Palacios S, Pérez M. Epidemiology of risk factors and symptoms associated with menopause in Spanish women. Maturitas. 2009;62:30–6. doi: 10.1016/j.maturitas.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Gynecology. 2, editor. Tehran: Sobhan; 2008. Danfurs. [Google Scholar]
- 4.Fritz M, Speroff L. Clinical gynecologic endocrinology and infertility. Westford: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 5.Sakala EP. High-yield obstetrics and gynecology. Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 6.Taibi DM, Landis CA, Vitiello MV. Concordance of polysomnographic and actigraphic measurement of sleep and wake in older women with insomnia. J Clin Sleep Med. 2013;9:217–25. doi: 10.5664/jcsm.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blackwell T, Redline S, Ancoli-Israel S, Schneider JL, Surovec S, Johnson NL, et al. Comparison of sleep parameters from actigraphy and polysomnography in older women: The SOF study. Sleep. 2008;31:283–91. doi: 10.1093/sleep/31.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott JR, Disaia PJ, Hammond CB, Spellacy WN, Gordon JD. Danforth's handbook of obstetrics and gynecology. Philadelphia, PA: Lippincott-Raven; 1996. [Google Scholar]
- 9.Gooneratne NS. Complementary and alternative medicine for sleep disturbances in older adults. Clin Geriatr Med. 2008;24:121–38. doi: 10.1016/j.cger.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherniack EP. The use of alternative medicine for the treatment of insomnia in the elderly. Psychogeriatrics. 2006;6:21–30. [Google Scholar]
- 11.Agarwal A, Ranjan R, Dhiraaj S, Lakra A, Kumar M, Singh U. Acupressure for prevention of pre-operative anxiety: A prospective, randomised, placebo controlled study. Anaesthesia. 2005;60:978–81. doi: 10.1111/j.1365-2044.2005.04332.x. [DOI] [PubMed] [Google Scholar]
- 12.Sun JL, Sung MS, Huang MY, Cheng GC, Lin CC. Effectiveness of acupressure for residents of long-term care facilities with insomnia: A randomized controlled trial. Int J Nurs Stud. 2010;47:798–805. doi: 10.1016/j.ijnurstu.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Kober A, Scheck T, Schubert B, Strasser H, Gustorff B, Bertalanffy P, et al. Auricular acupressure as a treatment for anxiety in prehospital transport settings. J Am Soc Anesthesiol. 2003;98:1328–32. doi: 10.1097/00000542-200306000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Tsay SL, Rong JR, Lin PF. THIS ARTICLE HAS BEEN RETRACTED Acupoints massage in improving the quality of sleep and quality of life in patients with end-stage renal disease. J Adv Nurs. 2003;42:134–42. doi: 10.1046/j.1365-2648.2003.02596.x. [DOI] [PubMed] [Google Scholar]
- 15.Shafiei M, Atri B. Pilates exercise program. 1st. Tehran: Talia; 2006. editor. [In perssion] [Google Scholar]
- 16.Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance, and posture. J Strength Cond Res. 2010;24:661–7. doi: 10.1519/JSC.0b013e3181c277a6. [DOI] [PubMed] [Google Scholar]
- 17.Bernardo LM. The effectiveness of Pilates training in healthy adults: An appraisal of the research literature. J Bodywork Mov Ther. 2007;11:106–10. [Google Scholar]
- 18.Adamany K, Loigerot D. The pilates edge: An athlete's guide to strength and performance: Penguin. 2004 [Google Scholar]
- 19.Nordio M, Romanelli F. Efficacy of wrists overnight compression (HT 7 point) on insomniacs: Possible role of melatonin? Minerva Med. 2008;99:539–47. [PubMed] [Google Scholar]
- 20.Cerrone R, Giani L, Galbiati B, Messina G, Casiraghi M, Proserpio E, et al. Efficacy of HT 7 point acupressure stimulation in the treatment of insomnia in cancer patients and in patients suffering from disorders other than cancer. Minerva Med. 2008;99:535–7. [PubMed] [Google Scholar]
- 21.Akiyoshi J. Neuropharmacological and genetic study of panic disorder. Nihon Shinkei Seishin Yakurigaku Zasshi. 1999;19:93–9. [PubMed] [Google Scholar]
- 22.Kotani N, Hashimoto H, Sato Y, Sessler DI, Yoshioka H, Kitayama M, et al. Preoperative intradermal acupuncture reduces postoperative pain, nausea and vomiting, analgesic requirement, and sympathoadrenal responses. Anesthesiology. 2001;95:349–56. doi: 10.1097/00000542-200108000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Basampur S, Nikbakht A, Mehran A. Effect of acupressure on anxiety and vital signs of patients before abdominal surgery. J Nurs Midwifery Tehran Univ Med Sci. 2008;2:23–44. [Google Scholar]
- 24.Hoseinabadi R, Nourozi K, Pouresmail Z, Karimlu M, Sadat SM, Cheraghi M. The effect of acupressure on quality of sleep in Iranian elderly nursing home residents. Rehabil Sci Res. 2008;9:8–14. [Google Scholar]
- 25.Malekzadegan A, Moradkhani M. The effect of relaxation on sleep disturbance during the third trimester. J Iran Univ Med Sci. 2010;23:52–8. [Google Scholar]
- 26.Rasuli F, Hagiamiri P. Mental health problems in postmenopausal women. Life Magazine. 2004;20:4–16. [Google Scholar]
- 27.Sedighi J, Maftoon F, Moshrefi F. Complementary and alternative medicine (CAM).knowledge, attitude and practice in Tehran. Iran Payesh. 2004;4:279–89. [Google Scholar]
- 28.Chen ML, Lin LC, Wu SC, Lin JG. The effectiveness of acupressure in improving the quality of sleep of institutionalized residents. J Gerontol A Biol Sci Med Sci. 1999;54:M389–94. doi: 10.1093/gerona/54.8.m389. [DOI] [PubMed] [Google Scholar]
- 29.da Silva JBG, Nakamura MU, Cordeiro JA, Kulay L. Acupuncture for insomnia in pregnancy–A prospective, quasi-randomised, controlled study. Acupuncture Med. 2005;23:47–51. doi: 10.1136/aim.23.2.47. [DOI] [PubMed] [Google Scholar]
- 30.Marques NR, Morcelli MH, Hallal CZ, Gonçalves M. EMG activity of trunk stabilizer muscles during Centering Principle of Pilates Method. J Bodywork Mov Ther. 2013;17:185–91. doi: 10.1016/j.jbmt.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 31.MirMohammadalie M, Ashrafinia F, Rajabi H. Effects of exercise on sleep quality in postpartum women. J Nurs Midwifery Tehran Univ Med Sci. 2012;1:20–9. [Google Scholar]
- 32.Arab Z, Shariaty A, Bahrami H. Effect of acupressure on quality of sleep in patients undergoing hemodialysis. Orumiye School Nurs Midwifery. 2012;2:237–45. [Google Scholar]
- 33.Caldwell K, Harrison M, Adams M, Travis Triplett N. Effect of Pilates and taiji quan training on self-efficacy, sleep quality, mood, and physical performance of college students. J Bodywork Mov Ther. 2009;13:155–63. doi: 10.1016/j.jbmt.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Leopoldino AAO, Avelar NCP, Passos GB, Jr, Santana NÁP, Jr, Teixeira VP, Jr, de Lima VP, et al. Effect of Pilates on sleep quality and quality of life of sedentary population. J Bodywork Mov Ther. 2013;17:5–10. doi: 10.1016/j.jbmt.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Rizk SA. Effect of acupressure on menopausal symptoms among women. J American Sci. 2013;9:416–24. [Google Scholar]
- 36.Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al. Leptin-replacement therapy for lipodystrophy. N Eng J Med. 2002;8:570–8. doi: 10.1056/NEJMoa012437. [DOI] [PubMed] [Google Scholar]
- 37.Karimian N, Rezaeian M, Nassaji F, Velaei N, Gachkar L. The effects of physical activity on premenstrual-syndrome. J Zanjan Univ Med Sci. 2006;13:8–15. [Google Scholar]
- 38.Nikbakht M, Ebadi G. The comparison of two training methods of walking and runing on the premenstrual syndrome (PMS) in high school girls of Ahwaz. Res Sport Sci. 2007;14:54–69. [Google Scholar]


