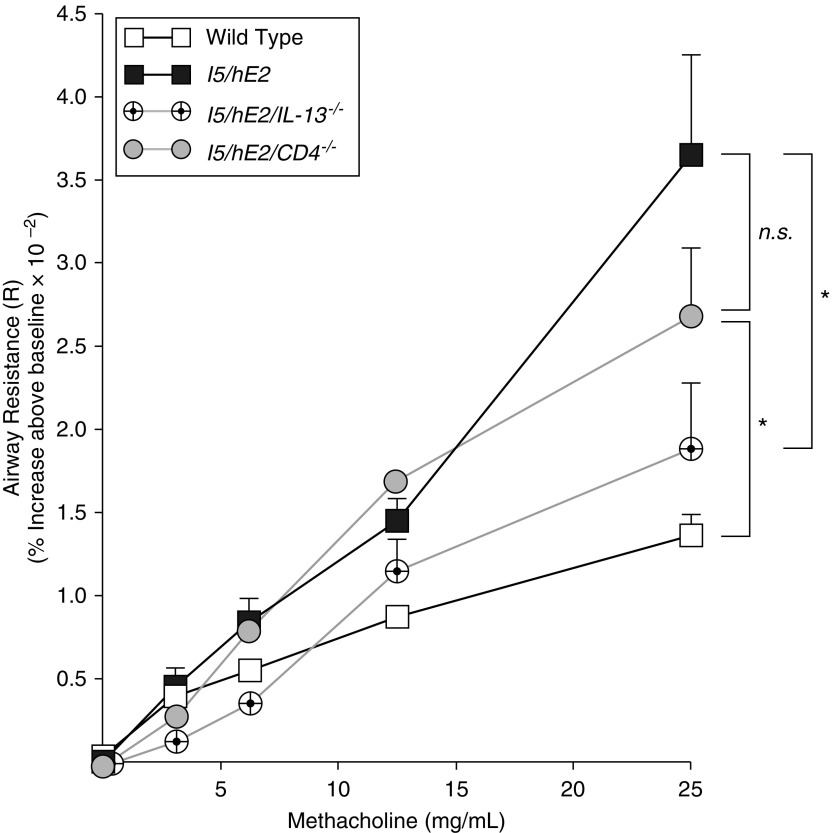
Figure 3.
The induced airway hyperresponsiveness linked with the pulmonary eosinophilia of I5/hE2 mice is dependent on IL-13 expression and not the presence/absence of CD4+ T cells. Aerosolized methacholine-induced airway resistance was assessed using an invasive ventilator-based technique (flexi-Vent; SCIREQ). I5/hE2 mice displayed an increase in airway resistance (relative to wild-type C57BL/6J mice) as a function of exposure to increasing concentrations of aerosolized methacholine. In contrast, the absence of IL-13 expression (i.e., I5/hE2/IL-13−/−) resulted in a significant reduction in methacholine responses, which became comparable wild-type C57BL/6J mice. A deficiency in CD4+ T cells (i.e., I5/hE2/CD4−/−) resulted only in a small decrease in airway resistance compared with the parental I5/hE2 model at the highest dose of methacholine exposure, but this reduction did not achieve statistical significance. Baseline airway resistance (cm H2O⋅s/ml) of each experimental cohort (mean ± SEM): C57BL/6J wild-type, 0.95 ± 0.05; I5/hE2, 0.95 ± 0.04; I5/hE2/IL-13−/−, 0.94 ± 0.07; and I5/hE2/CD4−/−, 0.82 ± 0.05. Cohort sizes: C57BL/6J, n = 11; I5/hE2, n = 12; I5/hE2/CD4−/−, n = 7; I5/hE2/IL-13−/−, n = 7. Error bars represent SEM. *P < 0.05; n.s. = not significant.