Abstract
Background and Aims:
Controlled hypotension with balanced anaesthesia minimises blood loss. This study was done to evaluate the effectiveness of intravenous clonidine as a single bolus dose to establish controlled hypotension during functional endoscopic sinus surgery (FESS).
Methods:
This randomised, double-blind, placebo-controlled study was done in a tertiary hospital in India. Sixty American Society of Anesthesiologists physical status I and II patients (18–65 years) undergoing FESS were randomly allocated to one of the two groups. Placebo group (group A, n = 30) received sterile water whereas the clonidine group (group B, n = 30) received 3μg/kg of clonidine intravenously, 30 min prior to induction of anaesthesia. The primary outcome was to achieve a target mean arterial blood pressure (MAP) of 55–65 mmHg intraoperatively. The secondary outcomes measured were requirement of additional fentanyl and metoprolol, intra-operative blood loss, surgeon's opinion on the surgical field, pain, sedation score and complications requiring treatment.
Results:
Target MAP was easily achieved in clonidine group as against the placebo group (P < 0.001). Significant reduction in intra-operative blood loss (P = 0.0449), a better surgical site scoring (P = 0.02), less requirement of additional hypotensive drugs and good analgesia (P = 0.01) were seen in clonidine group. The complication rates were similar in both the groups.
Conclusion:
Clonidine is effective in achieving controlled hypotension in patients undergoing FESS. It reduces intra-operative blood loss, requirement of additional hypotensive drugs, improves the surgical field and offers good analgesia without significant side effects.
Key words: Balanced anaesthesia, clonidine, controlled hypotension
INTRODUCTION
Excessive blood in the field of operation obscures visibility and may lead to complications during functional endoscopic sinus surgery (FESS).[1] Hence, an almost bloodless surgery would provide the surgeon with a clear field minimising the risk of injury to vital structures, minimising the intra-operative blood loss and the surgical time. 'Bloodless surgical field' can be achieved by inducing controlled hypotension with various agents such as inhalational anaesthetics,[2] beta blockers, magnesium, total intravenous anaesthetic agent such as propofol,[3,4] vasodilators such as nitrate and sodium nitroprusside[5] and alpha 2 agonists such as clonidine and dexmedetomidine. Inhalational agents used on their own can cause a delay in awakening and shivering during the recovery period. Metoprolol is one of the commonly used drugs to reduce cardiac output, heart rate and blood pressure (BP). Its effect is neither quick nor long lasting and it cannot be given as an infusion. Vasodilators, such as nitrates and sodium nitroprusside, are short-acting agents requiring infusions for a continuous steady state plasma concentration and their effect can be immediately terminated on stopping the infusion. They cause a rapid fall in the systemic vascular resistance (SVR) and BP requiring titration of the rate of infusion and beat-to-beat BP monitoring. Propofol reduces SVR resulting in fall of BP and causes dose-dependent cortical depression also. However, the recovery from propofol is rapid due to redistribution. Therefore, for a continuous hypotensive effect, propofol infusion with a target plasma concentration is required which may become expensive. In addition, metoprolol and propofol lack analgesic properties.
Alpha 2 agonists have potentially favourable effects. In addition to their hypotensive effect, they have analgesic and sedative properties. They provide haemodynamic stability as a result of the central sympatholytic effect. Clonidine and more recently dexmedetomidine have been used in anaesthetic practice to achieve controlled hypotension.[6] In this study, we evaluated the hypotensive effect of single bolus dose of clonidine in patients undergoing FESS.
METHODS
This study was a randomised, double-blind, placebo-controlled interventional trial. After obtaining approval from the research and ethics committee of our institution, it was registered in the Clinical Trial Registry of India as CTRI/2012/07/002790. Sixty American Society of Anesthesiologists class I and II patients who were scheduled for FESS were enrolled in the study.
The inclusion criteria were all adults, in the age group of 18–65 years, undergoing limited or full FESS. Patients with hypertension, diabetes with autonomic dysfunction, patients on beta-blocker therapy, those with heart blocks, ischaemic heart disease, on pacemakers and parturients were excluded from the study.
A written consent was obtained, and the patients were pre-medicated with diazepam (0.1 mg/kg) and metoclopramide (0.1 mg/kg) orally, an hour prior to induction of anaesthesia. The patients were randomly allocated to the comparator group (placebo n = 30) or intervention group (clonidine n = 30).
A computer-generated randomisation table was generated prior to commencement of the study by the statistician and concealed in sealed opaque envelopes. The patients were randomised into two groups using block randomisation. A qualified anaesthesia technician not involved in the operation list opened the sealed envelope and loaded the assigned drug. The patients received either the placebo or the study drug based on the randomisation. Patients, all medical and paramedical personnel in operating room, recovery room and the primary investigator were blinded to the intervention.
In the operating room, routine pre-operative monitoring, namely, electrocardiogram, non-invasive BP and pulse-oximetry (Philips Viridia V24C) were established. A peripheral intravenous cannula was inserted and intravenous fluid was commenced. Baseline vital parameters as mentioned above were recorded and repeated every 5 min from the pre-anaesthetic to intra-operative period till the patient was shifted to the recovery room. Based on randomisation, the patients received 3 μg/kg of clonidine or an equal volume of sterile water for injection intravenously 30 min prior to induction of anaesthesia, administered over 10 min. General anaesthesia was induced with intravenous thiopentone (5 mg/kg) and fentanyl (up to 1.5 μg/kg). After ensuring the ability to ventilate, endotracheal intubation was facilitated with IV vecuronium (0.1 mg/kg). Anaesthesia was maintained with oxygen, air and isoflurane (Datex Ohmeda Excel 210 SE). End-tidal anaesthetic concentration was monitored to maintain a minimum alveolar concentration (MAC) of 1.0 of isoflurane during the surgery (Philips Anaesthesia Gas Module M1026B).
All patients were given a 15° reverse Trendelenburg position to improve the venous drainage. Balanced salt solution at 3 ml/kg/h IV was given intraoperatively. Further doses of fentanyl in 10–20 μg IV aliquots were given up to a total of 4 μg/kg at 10 min interval for control of mean arterial pressure (MAP) between 55 and 65 mmHg.
If MAP control was not achieved after a total of 4 μg/kg of fentanyl and isoflurane MAC of 1.0, metoprolol IV in 0.5 mg boluses was administered. If the BP was not in the target range with the above measures, 10 mg IV boluses of propofol were administered. If there was sinus bradycardia of <50/min, it was treated with atropine (0.02 mg/kg) IV, and if MAP was <55 mmHg, the inspired isoflurane concentration was reduced by 0.5%, till MAC reached 0.75. If hypotension persisted, ephedrine 3 mg in incremental dosage was administered. At the end of the procedure, the anaesthetic agent was discontinued, throat pack was removed and residual paralysis was reversed with IV neostigmine (0.05 mg/kg) and IV glycopyrrolate (0.02 mg/kg). The patients were extubated when awake and were monitored in recovery room. Vital parameters, namely, BP, pulse rate, respiration and oxygen saturation were measured at 5 min interval from the time of intervention till discharge to the ward. Sedation and pain scores were measured in recovery room.
Blood loss was estimated by measuring the volume in the suction bottle and the number of swabs soaked in blood accounting for any saline flush use during the procedure. The surgeons graded the surgical field at the end of the procedure using Fromme–Boezaart scale [Annexure 1].[7] Clear surgery field with no suctioning required was defined as 'bloodless' field.
Pain was assessed using the numerical rating scale (NRS) from 0 (no pain) to 10 (worst pain imaginable) and sedation was assessed using Brussel's sedation score [Annexure 2].[8]
The primary outcome was the achievement of controlled hypotension with MAP of 55–65 mmHg. The secondary outcomes measured were blood loss, usage and dose of metoprolol and fentanyl, volatile anaesthetic requirement, quality of the surgical field, analgesia in the immediate post-operative period and incidence of complications/side effects, namely, prolonged sedation, bradycardia and hypotension.
Sample size was calculated based on a previous study which was done on a European population.[9]
To find a difference of 40% in hypotension between the study groups, sample size was calculated to be 30 in each group. Power of the study was assumed to be 80% and level of significance was fixed at 5%.
Normally distributed values were summarised using mean with standard deviation (SD). Variables with skewed distributions were described with median and range. Chi-square test was used to compare outcome variables. All calculated P values were two sided. Analysis was done using STATA 10.0 (Statacorp, College Station, TX, USA). Intention-to-treat analysis was used for all the outcomes.
RESULTS
Thirty patients who were allocated to placebo group received placebo and were analysed as Group A. Similarly, clonidine group received clonidine as the study drug and was analysed as Group B. Analysis was done on an intention-to-treat basis. There was no crossover or interchange of the intervention drug [Figure 1].
Figure 1.
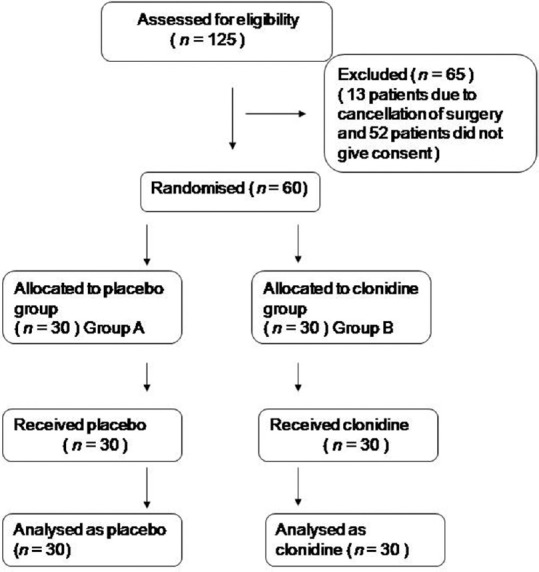
Participant flow
The most common pre-operative diagnosis in both the groups was chronic sinusitis and nasal polyposis. There was no statistical difference in the pre-operative diagnosis criterion. The age, gender and body weight were comparable between the two groups.
Target BP was achieved in 2 patients in Group A (placebo group) and 14 patients in Group B (clonidine group) with the induction dose of fentanyl alone (P < 0.001). In 13 patients from Group B, target BP was achieved with additional fentanyl up to a total maximum dose of 4 μg/kg compared to six in Group A (P < 0.001). Only one patient in Group B as against 20 in Group A needed metoprolol to achieve target BP (P < 0.001). The trend of mean arterial BP (MAP) between the two groups is shown in Figure 2. In two patients in group A and one patient in group B, propofol was administered to control BP when fentanyl and metoprolol failed to control BP [P = 0.55, Table 1].
Figure 2.
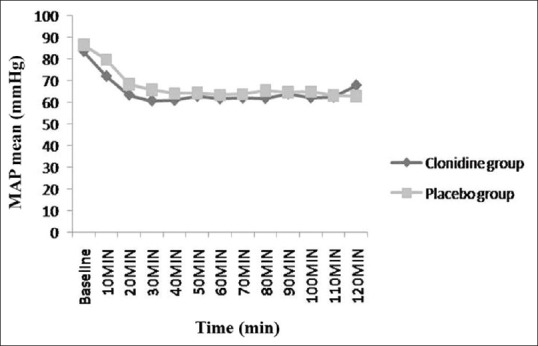
Mean arterial pressure (mmHg) trend in the two groups. X axis: time (min) Y axis: MAP mean (mmHg)
Table 1.
A comparison of requirement of additional hypotensive drugs for attainment of controlled hypotension

Median blood loss was significantly less (63.5 mL [range: 40–200 mL]) in Group B as compared to (180 mL [range: 70–300 mL]) Group A (P = 0.0449). Eleven patients in Group B and 3 in Group A had an excellent field of surgery (P = 0.02).
There was a significant difference in the pain score in both the groups in the immediate post-operative period, with NRS score ranging from 0 to 5 in patients from Group A and 0–3 range in patients from Group B (P = 0.01). Out of sixty patients, only six patients required lower anaesthetic concentration (isoflurane MAC <1.0) at one set point of time. One patient in Group A and 5 in Group B needed <1 MAC isoflurane at 1 h. This was not statistically significant. There was no difference seen in heart rate between the two groups. The trend of heart rate between the two groups is shown in [Figure 3].
Figure 3.
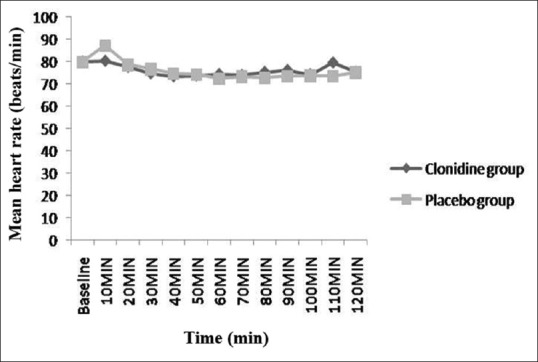
Mean heart rate (beats/min) trend in the two groups. X axis: time (min) Y axis: Mean heart rate (beats/min)
In terms of side effects, three patients in Group A and two in Group B had a prolonged duration of sedation. Nine patients in Group A and 10 in Group B had hypotension needing treatment. None in Group A and one patient in Group B had bradycardia. All these side effects were not statistically significant.
DISCUSSION
Controlled hypotension has become a very helpful technique in surgeries where a bloodless field is desired. Hypotensive techniques are used widely in procedures where major blood loss is expected or to aid a 'bloodless surgical field'. Minimising blood loss has potential benefits in terms of duration of procedure, less complications and transfusion requirements. Inhalational anaesthetic technique based on agents such as isoflurane, total intravenous anaesthetic technique using propofol, drugs with primary cardiovascular effect such as beta-blockers and vasodilators such as glyceryl trinitrate and sodium nitroprusside are being employed in surgeries such as FESS. However, the need of better results and improvement in the surgical field has always been a reason for further research.
FESS is the treatment modality that is preferred for the inflammatory disease of the paranasal sinuses.[10,11] Any operation involving the nasal mucosa results in a severe sympathetic response causing tachycardia as well as hypertension, and being very vascular, the nasal and paranasal regions tend to bleed easily. This has led to studies on many drugs that can be used for minimising bleeding by achieving controlled hypotension. Clonidine has sedative and analgesic properties in addition to the hypotensive effect. This study was designed to evaluate the hypotensive effect of clonidine when used with balanced anaesthesia, along with its other benefits. A body weight-based dose of clonidine through intravenous route administered 30 min before induction was chosen to maximise the bioavailability and standardise the timing and dose of clonidine. Dexmedetomidine is another α 2 agonist drug which has been used successfully for controlled hypotension in endoscopic sinus surgeries.[12] The cost factor and the requirement of an infusion are the undesirable features of dexmedetomidine. Clonidine is less expensive and is used as a one-time bolus, which is an advantage, especially in developing countries.
In this study, it was possible to achieve the target mean BP of 55–65 mmHg in all the patients. There was a decrease in MAP in the first 30 min of pre-induction period in clonidine group, whereas in placebo group, MAP remained the same as baseline. The target MAP was readily achieved in most patients in the clonidine group whereas in placebo group many patients required boluses of metoprolol to achieve the target MAP. This suggested that, at different intervals, there were periods of high MAP readings that warranted the use of metoprolol more so in placebo group, which is similar to a previous study done in European population where the requirement of metoprolol was significantly less in clonidine group (P < 0.00035).[9] The majority of patients in clonidine group did not require metoprolol. Hence, clonidine was able to achieve controlled hypotension solely along with balanced anaesthetic technique. However, there were two patients in group A and one patient in group B, who needed propofol in addition to fentanyl and metoprolol to achieve the target MAP.
Out of 30 patients, 28 patients in placebo group required additional fentanyl, whereas in the clonidine group, only 16 out of 30 patients required extra fentanyl, in addition to the induction dose. This is similar to a study where clonidine was effective in reducing the requirement of fentanyl, isoflurane and beta-blockers.[13] This study conducted on adolescent children showed that clonidine reduced the requirement of fentanyl, isoflurane and labetalol. Our study did not show significant reduction in the requirement of isoflurane between the two groups.
Our study showed no significant difference between the two groups in terms of heart rate measured at different time intervals as opposed to a previous study where beta-blockers were used for hypotension in FESS.[14] Their study showed a significant difference in overall mean heart rate between the placebo and the beta-blocker groups (P < 0.0001). In the entire group, surgical grade correlated with heart rate (r = 0.36, P < 0.05) but not with MAP. Surgical grade was significantly better in those with a mean heart rate of <60 beats/min (P < 0.02).
Hypotension requiring treatment was seen in 30% of patients in placebo group and 33.3% of patients in clonidine group, which was not statistically significant. In one of the previous study done on use of inhalational agent in FESS, controlled hypotension was achieved in thirty patients undergoing FESS using isoflurane with mean inspired isoflurane of 3.8%.[2] As seen in their study, hypotensive anaesthesia with isoflurane resulted in less bleeding compared to normotensive anaesthesia provided by isoflurane. In another comparative study, esmolol infusion produced better surgical field at an acceptable MAP than SNP infusion which produced similar effect at severe levels of hypotension.[5] In our study, it was observed that many patients achieved controlled hypotension in clonidine group with significantly less mean blood loss when compared to placebo group (P = 0.0449). Surgical field grading showed that the clonidine group had an excellent grade than the placebo group (P = 0.02).
NRS (0–10) was used to assess post-operative pain in the recovery room. It was found that patients who received clonidine had significantly less pain score than the placebo (P = 0.01). Sedation score was found to be similar in both the groups (P = 0.640). The anaesthetic concentration was titrated using the anaesthetic gas analyser, towards the time of extubation. Prolonged sedation was seen in very few patients in both the groups. Other complications namely hypotension (P = 0.781) and bradycardia (P = 0.313) requiring treatment were similar in both the groups.
CONCLUSION
Clonidine, as a single bolus dose, is effective in achieving controlled hypotension when used with balanced anaesthesia in FESS and reduces the intraoperative requirement of additional fentanyl and metoprolol. It effectively reduces the intraoperative blood loss and provides a dry operating field. Clonidine also provides good analgesia without any significant side effects such as sedation, hypotension and bradycardia. Use of clonidine for controlled hypotension is simple, safe and cheap, which makes economic sense for developing and developed countries.
Financial support and sponsorship
The project was funded by the fluid research grant of Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are thankful to the fluid research grant of Christian Medical College and Hospital, Vellore, Tamil Nadu, India, for the financial help provided for the study.
ANNEXURES
Annexure 1. Fromme–Boezaart scale of surgical field grading
Grade 0: No bleeding
Grade 1: Slight bleeding; no suctioning of blood required
Grade 2: Slight bleeding; occasional suctioning required. Surgical field not threatened
Grade 3: Slight bleeding; frequent suctioning required; bleeding threatens surgical field a few seconds after suction is removed
Grade 4: Moderate bleeding; frequent suctioning required, bleeding threatens surgical field directly after suction is removed
Grade 5: severe bleeding: Constant suctioning required, bleeding appears faster than can be removed by suction, surgical field severely threatened and surgery impossible.
Excellent (Grade 0–1)
Good (Grades 2–3)
Poor (Grades 4–5).
Annexure 2. Brussel's sedation score
Unarousable
Responding to pain stimulation (trapezius muscle pinching) and not to auditory stimulation
Responding to auditory stimulation
Awake and calm
Agitated.
REFERENCES
- 1.Stankiewicz JA. Complications of endoscopic intranasal ethmoidectomy. Laryngoscope. 1987;97:1270–3. doi: 10.1288/00005537-198711000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Mandal P. Isoflurane anaesthesia for functional endoscopic sinus surgery. Indian J Anaesth. 2003;47:37–40. [Google Scholar]
- 3.Ankichetty SP, Ponniah M, Cherian V, Thomas S, Kumar K, Jeslin L, et al. Comparison of total intravenous anesthesia using propofol and inhalational anesthesia using isoflurane for controlled hypotension in functional endoscopic sinus surgery. J Anaesthesiol Clin Pharmacol. 2011;27:328–32. doi: 10.4103/0970-9185.83675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boonmak S, Boonmak P, Laopaiboon M. Deliberate hypotension with propofol under anaesthesia for functional endoscopic sinus surgery (FESS) Cochrane Database Syst Rev. 2013;6:CD006623. doi: 10.1002/14651858.CD006623.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside-and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42(5 Pt 1):373–6. doi: 10.1007/BF03015479. [DOI] [PubMed] [Google Scholar]
- 6.Maze M, Tranquilli W. Alpha-2 adrenoceptor agonists: Defining the role in clinical anesthesia. Anesthesiology. 1991;74:581–605. [PubMed] [Google Scholar]
- 7.Athanasiadis T, Beule A, Embate J, Steinmeier E, Field J, Wormald PJ. Standardized video-endoscopy and surgical field grading scale for endoscopic sinus surgery: A multi-centre study. Laryngoscope. 2008;118:314–9. doi: 10.1097/MLG.0b013e318157f764. [DOI] [PubMed] [Google Scholar]
- 8.Detriche O, Berré J, Massaut J, Vincent JL. The Brussels sedation scale: Use of a simple clinical sedation scale can avoid excessive sedation in patients undergoing mechanical ventilation in the Intensive Care Unit. Br J Anaesth. 1999;83:698–701. doi: 10.1093/bja/83.5.698. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Lovell AT, Parry MG, Glaisyer HR, Bromley LM. I.v. clonidine: Does it work as a hypotensive agent with inhalation anaesthesia? Br J Anaesth. 1999;82:639–40. doi: 10.1093/bja/82.4.639. [DOI] [PubMed] [Google Scholar]
- 10.Tewfik MA, Wormald PJ. Ten pearls for safe endoscopic sinus surgery. Otolaryngol Clin North Am. 2010;43:933–44. doi: 10.1016/j.otc.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Baker AR, Baker AB. Anaesthesia for endoscopic sinus surgery. Acta Anaesthesiol Scand. 2010;54:795–803. doi: 10.1111/j.1399-6576.2010.02259.x. [DOI] [PubMed] [Google Scholar]
- 12.Shams T, El Bahnasawe NS, Abu-Samra M, El-Masry R. Induced hypotension for functional endoscopic sinus surgery: A comparative study of dexmedetomidine versus esmolol. Saudi J Anaesth. 2013;7:175–80. doi: 10.4103/1658-354X.114073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hackmann T, Friesen M, Allen S, Precious DS. Clonidine facilitates controlled hypotension in adolescent children. Anesth Analg. 2003;96:976–81. doi: 10.1213/01.ANE.0000052713.72875.13. [DOI] [PubMed] [Google Scholar]
- 14.Nair S, Collins M, Hung P, Rees G, Close D, Wormald PJ. The effect of beta-blocker premedication on the surgical field during endoscopic sinus surgery. Laryngoscope. 2004;114:1042–6. doi: 10.1097/00005537-200406000-00016. [DOI] [PubMed] [Google Scholar]


